Lumbar dermatomes and myotomes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lumbar dermatomes and myotomes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lumbar dermatomes and myotomes US Medical PG Question 1: A 49-year-old man comes to the physician because of severe, shooting pain in his lower back for the past 2 weeks. The pain radiates down the back of both legs and started after he lifted a concrete manhole cover from the ground. Physical examination shows decreased sensation to light touch bilaterally over the lateral thigh area and lateral calf bilaterally. Patellar reflex is decreased on both sides. The passive raising of either the right or left leg beyond 30 degrees triggers a shooting pain down the leg past the knee. Which of the following is the most likely underlying cause of this patient's current condition?
- A. Inflammatory reaction in the epidural space
- B. Involuntary contraction of the paraspinal muscles
- C. Compromised integrity of the vertebral body
- D. Inflammatory degeneration of the spine
- E. Herniation of nucleus pulposus into vertebral canal (Correct Answer)
Lumbar dermatomes and myotomes Explanation: ***Herniation of nucleus pulposus into vertebral canal***
- The sudden onset of **bilateral lower back pain** radiating down both legs, associated with **lifting a heavy object**, and presenting with **decreased sensation** in dermatomal patterns (lateral thigh/calf) and **diminished patellar reflexes**, is highly consistent with **acute disc herniation**.
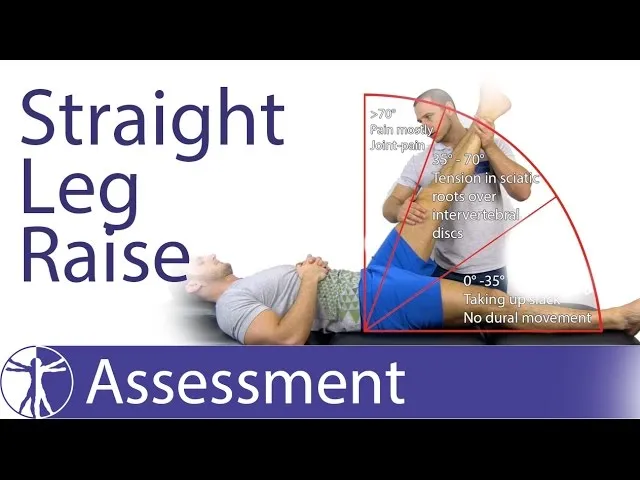
- **Positive straight leg raise test** (pain beyond 30 degrees) further implicates **nerve root compression** due to a herniated disc, specifically affecting the L3/L4 or L4/L5 levels given the reflex and sensory findings.
*Inflammatory reaction in the epidural space*
- While an inflammatory reaction can cause pain, it typically wouldn't present with such specific **neurological deficits** (sensory loss, reflex changes) and **mechanical provocation** (lifting, straight leg raise).
- This option does not explain the **radicular symptoms** so precisely or the classic presentation after acute strain.
*Involuntary contraction of the paraspinal muscles*
- **Muscle spasms** can cause severe back pain but usually do not lead to **bilateral radicular pain**, specific **sensory deficits**, or **reflex changes**.
- The symptoms described point to **nerve root impingement**, not just muscular pain.
*Compromised integrity of the vertebral body*
- Conditions like **vertebral fractures** or **tumors** affecting vertebral body integrity might cause severe localized pain, but wouldn't typically manifest as **bilateral radiculopathy** with specific **neurological deficits** and a clear mechanical trigger in this manner.
- While possible, it's not the most likely cause given the classic disc herniation presentation.
*Inflammatory degeneration of the spine*
- **Inflammatory degeneration** (e.g., degenerative disc disease, spondylosis) tends to have a more **chronic, progressive course** rather than the acute onset described after a specific event.
- While degeneration can predispose to herniation, it is not the immediate cause of the acute clinical picture of nerve impingement.
Lumbar dermatomes and myotomes US Medical PG Question 2: A 38-year-old man is brought to the emergency department after suffering a motor vehicle accident as the passenger. He had no obvious injuries, but he complains of excruciating right hip pain. His right leg is externally rotated, abducted, and extended at the hip and the femoral head can be palpated anterior to the pelvis. Plain radiographs of the pelvis reveal a right anterior hip dislocation and femoral head fracture. Which sensory and motor deficits are most likely in this patient's right lower extremity?
- A. Loss of sensation laterally below the knee, weak thigh extension and knee flexion
- B. Numbness of the ipsilateral scrotum and upper medial thigh
- C. Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop
- D. Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension
- E. Numbness of the medial side of the thigh and inability to adduct the thigh (Correct Answer)
Lumbar dermatomes and myotomes Explanation: ***Numbness of the medial side of the thigh and inability to adduct the thigh***
- An **anterior hip dislocation** is caused by forced **abduction** and **external rotation**, putting the **obturator nerve** at risk due to its anatomical course through the **obturator foramen** and proximity to the hip joint.
- Damage to the **obturator nerve** (L2-L4) results in **sensory loss** over the **medial thigh** and paralysis of the **adductor muscles** (adductor longus, brevis, magnus, gracilis), leading to an inability to adduct the thigh.
*Loss of sensation laterally below the knee, weak thigh extension and knee flexion*
- **Sensory loss laterally below the knee** and **weak thigh extension/knee flexion** are characteristic of **sciatic nerve** or common **peroneal nerve injury**, which is more common in **posterior hip dislocations**.
- The presented case describes an **anterior dislocation**, making **obturator nerve** injury more likely than sciatic nerve injury.
*Numbness of the ipsilateral scrotum and upper medial thigh*
- **Numbness of the ipsilateral scrotum** and **upper medial thigh** is associated with injury to the **ilioinguinal nerve** or **genitofemoral nerve**.
- While these nerves supply portions of the **medial thigh** and **genitalia**, they are not typically injured in **anterior hip dislocations** which primarily affect deeper structures like the **obturator nerve**.
*Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop*
- **Sensory loss to the dorsal surface of the foot**, **anterior lower and lateral leg**, and **foot drop** are classic signs of **common peroneal nerve** injury due to its superficial course around the fibular head.
- Although the common peroneal nerve is a branch of the **sciatic nerve**, direct injury specifically to the **common peroneal nerve** in an anterior hip dislocation is less probable than obturator nerve injury, and foot drop is characteristic of more severe neural compromise, typically seen in **posterior dislocations or direct trauma**.
*Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension*
- **Paresis and numbness of the medial thigh** are consistent with **obturator nerve** injury. However, **numbness of the medial side of the calf** and **weak hip flexion/knee extension** point towards **femoral nerve** injury.
- While the **femoral nerve** can be injured, the prominent clinical picture of **anterior hip dislocation** points more directly to the **obturator nerve** findings of medial thigh numbness and adduction weakness, rather than primarily femoral nerve symptoms.
Lumbar dermatomes and myotomes US Medical PG Question 3: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Lumbar dermatomes and myotomes Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Lumbar dermatomes and myotomes US Medical PG Question 4: A 48-year-old male presents to his primary care provider with a two-week history of low back pain and left leg pain. He reports that his symptoms started while he was working at his job as a construction worker. He has since experienced intermittent achy pain over his lumbar spine. He has also noticed pain radiating into his left leg and weakness in left ankle dorsiflexion. On exam, he demonstrates the following findings on strength testing of the left leg: 5/5 in knee extension, 4/5 in ankle dorsiflexion, 4/5 in great toe extension, 5/5 in ankle plantarflexion, and 5/5 in great toe flexion. The patellar reflexes are 5/5 bilaterally. He is able to toe walk but has difficulty with heel walking. Weakness in which of the following compartments of the leg is most likely causing this patient’s foot drop?
- A. Lateral compartment
- B. Superficial posterior compartment
- C. Deep posterior compartment
- D. Anterior compartment (Correct Answer)
- E. Medial compartment
Lumbar dermatomes and myotomes Explanation: ***Anterior compartment***
- Weakness in **ankle dorsiflexion** and **great toe extension**, coupled with difficulty **heel walking**, indicates a foot drop due to dysfunction of muscles in the anterior compartment, such as the **tibialis anterior**, **extensor hallucis longus**, and **extensor digitorum longus**.
- These muscles are primarily innervated by the **deep fibular nerve**, which is susceptible to compression from conditions like **lumbar radiculopathy** (L4-L5 nerve root involvement).
*Lateral compartment*
- Muscles in the lateral compartment (**fibularis longus** and **brevis**) are responsible for **eversion** of the foot.
- Weakness in this compartment would manifest as difficulty everting the foot, not primarily ankle dorsiflexion or great toe extension deficits.
*Superficial posterior compartment*
- This compartment contains muscles like the **gastrocnemius** and **soleus**, which are primarily responsible for **ankle plantarflexion**.
- The patient exhibits 5/5 strength in ankle plantarflexion and is able to toe walk, indicating these muscles are functioning well.
*Deep posterior compartment*
- Muscles in the deep posterior compartment (**tibialis posterior**, **flexor digitorum longus**, **flexor hallucis longus**) are involved in **inversion** and **toe flexion**.
- The patient has 5/5 strength in great toe flexion, suggesting intact function of these muscles, and his primary deficit is in dorsiflexion.
*Medial compartment*
- There is no distinct "medial compartment" of the leg in the anatomical sense comparable to the other listed compartments; rather, various muscles contribute to medial actions.
- The symptoms described specifically point to weakness in dorsiflexion and toe extension, localizing the problem to the anterior compartment.
Lumbar dermatomes and myotomes US Medical PG Question 5: A 41-year-old woman presents with back pain for the past 2 days. She says that the pain radiates down along the posterior right thigh and leg. She says the pain started suddenly after lifting a heavy box 2 days ago. Past medical history is irrelevant. Physical examination reveals a straight leg raise (SLR) test restricted to 30°, inability to walk on her toes, decreased sensation along the lateral border of her right foot, and diminished ankle jerk on the same side. Which of the following nerve roots is most likely compressed?
- A. Fourth lumbar nerve root (L4)
- B. Second sacral nerve root (S2)
- C. Third sacral nerve root (S3)
- D. Fifth lumbar nerve root (L5)
- E. First sacral nerve root (S1) (Correct Answer)
Lumbar dermatomes and myotomes Explanation: ***First sacral nerve root (S1)***
- **Inability to walk on toes** (weakness of gastrocnemius and soleus), **decreased sensation along the lateral border of the foot**, and a **diminished ankle jerk** are classic signs of S1 radiculopathy.
- The radiating pain down the posterior leg, restricted straight leg raise due to a sudden onset after lifting, points towards a **disc herniation** compressing the S1 nerve root.
*Fourth lumbar nerve root (L4)*
- Compression of L4 typically causes **weakness in knee extension** (quadriceps), diminished patellar reflex, and sensory loss over the medial aspect of the shin.
- The patient's symptoms (inability to walk on toes, diminished ankle jerk) are not consistent with L4 nerve root involvement.
*Second sacral nerve root (S2)*
- S2 radiculopathy primarily affects sensation in the posterior thigh and calf and can cause **weakness in knee flexion** and **plantarflexion**, but the complete constellation of symptoms (especially ankle jerk reflex) is more indicative of S1.
- Isolated S2 compression without S1 involvement is less common with these specific signs.
*Third sacral nerve root (S3)*
- S3 nerve root compression typically presents with **perineal numbness** and issues with bowel or bladder function due to its involvement in these functions.
- The described motor and sensory deficits are not characteristic of S3 radiculopathy.
*Fifth lumbar nerve root (L5)*
- L5 radiculopathy is characterized by **weakness in foot dorsiflexion** (foot drop) and toe extension, leading to inability to walk on heels, and sensory loss on the dorsum of the foot.
- While L5 compression can cause radiating pain and a restricted straight leg raise, the specific deficit of **inability to walk on toes** and a **diminished ankle jerk** are not typical of L5 involvement.
Lumbar dermatomes and myotomes US Medical PG Question 6: A 25-year-old woman presents with shooting pain along the lateral aspect of her right thigh. The pain is exacerbated by standing or walking for long periods. Physical examination reveals tenderness at the anterior superior iliac spine. Which of the following nerves is most likely affected?
- A. Common peroneal nerve
- B. Obturator nerve
- C. Sciatic nerve
- D. Lateral femoral cutaneous nerve (Correct Answer)
Lumbar dermatomes and myotomes Explanation: ***Lateral femoral cutaneous nerve***
- This presentation is classic for **meralgia paresthetica**, caused by compression of the **lateral femoral cutaneous nerve** as it passes under the inguinal ligament, leading to pain and numbness on the **lateral thigh**.
- Tenderness at the **anterior superior iliac spine** points to the inguinal ligament region where this nerve is most vulnerable to compression.
*Common peroneal nerve*
- Injury to the common peroneal nerve typically causes **foot drop** and sensory deficits over the **dorsum of the foot** and **lateral leg**, not the lateral thigh.
- It is often compressed at the **fibular head**, which is anatomically distinct from the anterior superior iliac spine.
*Obturator nerve*
- The obturator nerve innervates the **medial thigh muscles** and provides sensation to the medial thigh; its compression would cause pain in this region, not the lateral thigh.
- Injury often leads to **adductor weakness** and is typically associated with pelvic trauma or surgery.
*Sciatic nerve*
- Sciatic nerve pain typically radiates down the **posterior aspect of the leg** into the foot (**sciatica**), often associated with lumbar disc herniation.
- Sensory deficits would follow the dermatomal distribution of its branches (**tibial** and **common peroneal nerves**).
Lumbar dermatomes and myotomes US Medical PG Question 7: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Lumbar dermatomes and myotomes Explanation: ***S3–S4 nerve roots***
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Lumbar dermatomes and myotomes US Medical PG Question 8: A 13-year-old girl is brought to the physician by her father because of a 1-month history of pain in her right knee. She is a competitive volleyball player and has missed several games recently due to pain. Examination shows swelling distal to the right knee joint on the anterior surface of the proximal tibia; there is no overlying warmth or deformity. Extension of the right knee against resistance is painful. Which of the following structures is attached to the affected anterior tibial area?
- A. Patellar ligament (Correct Answer)
- B. Iliotibial band
- C. Pes anserinus tendon
- D. Quadriceps tendon
- E. Anterior cruciate ligament
Lumbar dermatomes and myotomes Explanation: ***Patellar ligament***
- The symptoms described, particularly **pain in the right knee worse with activity** in a young, active individual with **swelling distal to the knee joint on the anterior surface of the proximal tibia**, are classic for **Osgood-Schlatter disease**.
- This condition involves inflammation of the **patellar ligament** (also known as the patellar tendon) insertion onto the **tibial tuberosity**, which is the bony prominence on the anterior proximal tibia.
*Iliotibial band*
- The **iliotibial band (IT band)** runs along the lateral aspect of the thigh and inserts on the **lateral condyle of the tibia (Gerdy's tubercle)**, not the anterior proximal tibia.
- **IT band syndrome** typically causes lateral knee pain, often seen in runners, and not central anterior tibial swelling.
*Pes anserinus tendon*
- The **pes anserinus tendon** is formed by the conjoined tendons of the **sartorius**, **gracilis**, and **semitendinosus muscles**, inserting on the **medial proximal tibia**.
- Inflammation here (**pes anserinus bursitis/tendinitis**) would cause pain and swelling on the medial side of the knee, not the anterior aspect.
*Quadriceps tendon*
- The **quadriceps tendon** connects the quadriceps muscles to the **superior pole of the patella**, not the anterior proximal tibia.
- Conditions affecting this tendon typically cause pain above or at the patella, not distal to the knee joint.
*Anterior cruciate ligament*
- The **anterior cruciate ligament (ACL)** is an intra-articular ligament that connects the **femur to the tibia within the knee joint**.
- An **ACL injury** typically presents with acute pain, instability, and a "popping" sensation, not chronic swelling on the anterior aspect of the proximal tibia.
Lumbar dermatomes and myotomes US Medical PG Question 9: A 57-year-old man presents to the ED complaining of back and left leg pain. He was lifting heavy furniture while helping his daughter move into college when all of sudden he felt a sharp pain at his back. The pain is described as severe, worse with movement, and shoots down his lateral thigh. The patient denies any bowel/urinary incontinence, saddle anesthesia, weight loss, or weakness. He denies any past medical history but endorses a family history of osteoporosis. He has been smoking 1 pack per day for the past 20 years. Physical examination demonstrated decreased sensation at the left knee, decreased patellar reflex, and a positive straight leg test. There is diffuse tenderness to palpation at the lower back but no vertebral step-offs were detected. What is the most likely etiology for this patient’s pain?
- A. Vertebral compression fracture
- B. Disc herniation at the L4/L5 vertebra
- C. Spinal metastasis from lung cancer
- D. Disc herniation at the L3/L4 vertebra (Correct Answer)
- E. Lumbar muscle sprain
Lumbar dermatomes and myotomes Explanation: ***Disc herniation at the L3/L4 vertebra***
- The patient's symptoms of **acute back pain radiating down the lateral thigh** after lifting, combined with **decreased sensation at the left knee** and a **decreased patellar reflex**, are classic signs of L3/L4 nerve root compression.
- A **positive straight leg test** also supports nerve root irritation, and the absence of red flag symptoms like incontinence or saddle anesthesia makes a simple disc herniation more likely than other serious conditions.
*Vertebral compression fracture*
- While lifting heavy objects can cause compression fractures, these usually present with more **severe, localized pain** that is not typically radiating with specific dermatomal or reflex changes.
- Absence of **vertebral step-offs** or significant predisposing factors for a fracture (e.g., severe osteoporosis, trauma) makes this less likely given the specific neurological findings.
*Disc herniation at the L4/L5 vertebra*
- An L4/L5 disc herniation would typically cause symptoms related to the **L5 nerve root**, such as pain radiating down the **lateral leg into the foot**, **weakness in dorsiflexion of the ankle** or **big toe**, and potentially a **decreased medial hamstring reflex**.
- The patient's reported symptoms (lateral thigh pain, decreased knee sensation, decreased patellar reflex) are more consistent with **L4 nerve root** involvement.
*Spinal metastasis from lung cancer*
- Although the patient has a **smoking history** and could be at risk for lung cancer, this diagnosis typically presents with more **insidious onset** of unexplained back pain, often with **weight loss**, and sometimes with more profound neurological deficits or bone pain not relieved by rest.
- The acute onset after an inciting event and specific neurological findings of a single nerve root are less suggestive of metastasis.
*Lumbar muscle sprain*
- A muscle sprain would typically present with **localized back pain**, often worsened by movement, but would **not involve radicular pain** shooting down the leg, nor would it cause specific **neurological deficits** like decreased sensation or reflex changes.
- The positive straight leg test and neurological findings rule out a simple muscle sprain.
Lumbar dermatomes and myotomes US Medical PG Question 10: A 59-year-old woman presents to the emergency room with severe low back pain. She reports pain radiating down her left leg into her left foot. She also reports intermittent severe lower back spasms. The pain started after lifting multiple heavy boxes at her work as a grocery store clerk. She denies bowel or bladder dysfunction. Her past medical history is notable for osteoporosis and endometrial cancer. She underwent a hysterectomy 20 years earlier. She takes alendronate. Her temperature is 99°F (37.2°C), blood pressure is 135/85 mmHg, pulse is 85/min, and respirations are 22/min. Her BMI is 21 kg/m^2. On exam, she is unable to bend over due to pain. Her movements are slowed to prevent exacerbating her muscle spasms. A straight leg raise elicits severe radiating pain into her left lower extremity. The patient reports that the pain is worst along the posterior thigh and posterolateral leg into the fourth and fifth toes. Palpation along the lumbar vertebral spines demonstrates mild tenderness. Patellar reflexes are 2+ bilaterally. The Achilles reflex is decreased on the left. Which nerve root is most likely affected in this patient?
- A. L5
- B. S2
- C. L3
- D. L4
- E. S1 (Correct Answer)
Lumbar dermatomes and myotomes Explanation: ***S1***
- Pain radiating to the **posterior thigh**, **posterolateral leg**, and into the **fourth and fifth toes** is characteristic of **S1 dermatome involvement**.
- A **decreased Achilles reflex** (ankle jerk reflex) specifically points to compromise of the **S1 nerve root**.
*L5*
- **L5 radiculopathy** typically causes pain and sensory deficits in the **dorsum of the foot** and into the **first, second, and third toes**.
- Motor weakness often affects **foot dorsiflexion** and **toe extension**, not primarily the Achilles reflex.
*S2*
- **S2 radiculopathy** would primarily affect sensation along the **posterior thigh** and **calf**, with possible involvement of the **plantar aspect of the foot**.
- It does not typically cause a decrease in the **Achilles reflex**, which is predominantly S1.
*L3*
- **L3 radiculopathy** typically presents with pain and sensory changes along the **anterior thigh** and possibly the **medial knee**.
- It can affect the **patellar reflex**, which is intact in this patient, and does not cause pain in the posterior leg or foot.
*L4*
- **L4 radiculopathy** typically causes pain and sensory changes over the **anterior thigh**, **medial leg**, and potentially the **medial malleolus**.
- It often presents with weakness in **quadriceps muscle** and can cause a diminished **patellar reflex**, which is normal in this patient.
More Lumbar dermatomes and myotomes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.