Upper limb cross-sections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper limb cross-sections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
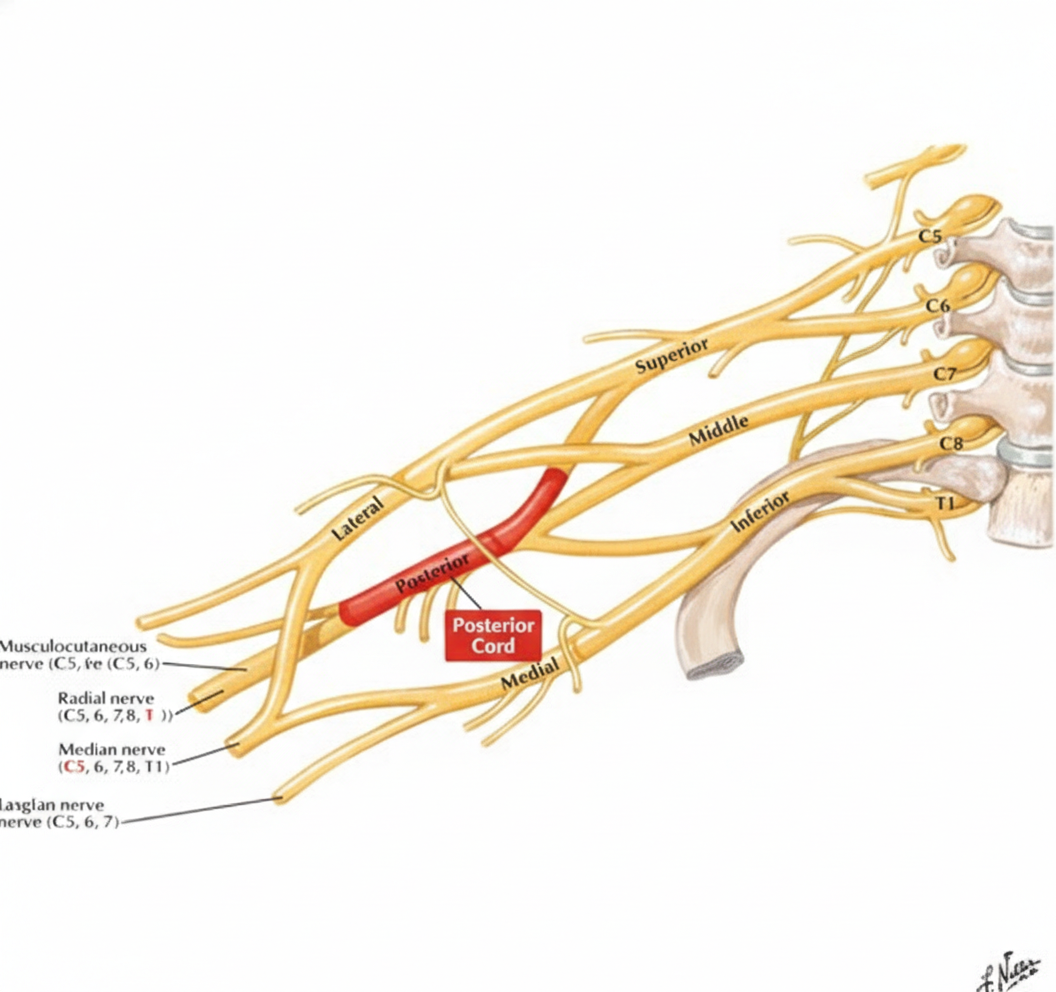
Upper limb cross-sections US Medical PG Question 1: A 43-year-old woman comes to the physician because of tingling and weakness in her left arm for the past 2 days. An image of the brachial plexus is shown. Nerve conduction study shows decreased transmission of electrical impulses in the labeled structure. Physical examination is most likely to show impairment of which of the following movements?
- A. Opposition of the thumb
- B. Flexion of the forearm
- C. Abduction of the shoulder above 100 degrees
- D. Extension of the wrist and fingers (Correct Answer)
- E. Flexion of the metacarpophalangeal joints
Upper limb cross-sections Explanation: ***Extension of the wrist and fingers***
- The image and description indicate the injury affects the **posterior cord** of the brachial plexus, which gives rise to the **radial nerve**.
- The **radial nerve** innervates the muscles responsible for **extension of the wrist and fingers**, so damage to its parent cord would impair these movements.
*Opposition of the thumb*
- **Opposition of the thumb** is primarily mediated by the **median nerve**, which arises from the lateral and medial cords, not the posterior cord.
- Damage to the posterior cord due to injury would not affect this movement directly.
*Flexion of the forearm*
- **Flexion of the forearm** is primarily controlled by the **musculocutaneous nerve** and a portion by the **median nerve**.
- Both of these nerves originate from the lateral and medial cords, not the posterior cord, making impairment unlikely with posterior cord injury.
*Abduction of the shoulder above 100 degrees*
- **Abduction of the shoulder above 100 degrees** primarily requires **scapular rotation** mediated by the **trapezius muscle** (accessory nerve) and **serratus anterior** (long thoracic nerve).
- While the **axillary nerve** (from the posterior cord) innervates the **deltoid** for initial shoulder abduction, the question stem emphasizes **wrist and finger symptoms**, suggesting the labeled structure is specifically the **radial nerve** branch rather than the axillary nerve branch.
- This makes extension deficits more likely than shoulder abduction impairment.
*Flexion of the metacarpophalangeal joints*
- **Flexion of the metacarpophalangeal joints** is predominantly carried out by the **lumbricals and interossei muscles**, which are primarily innervated by the **ulnar nerve** and partially by the **median nerve**.
- These nerves originate from the medial and lateral cords, not the posterior cord, making impairment unlikely.
Upper limb cross-sections US Medical PG Question 2: A 53-year-old woman comes to the physician because of a 3-month history of intermittent severe left neck, shoulder, and arm pain and paresthesias of the left hand. The pain radiates to the radial aspect of her left forearm, thumb, and index finger. She first noticed her symptoms after helping a friend set up a canopy tent. There is no family history of serious illness. She appears healthy. Vital signs are within normal limits. When the patient extends and rotates her head to the left and downward pressure is applied, she reports paresthesias along the radial aspect of her left forearm and thumb. There is weakness when extending the left wrist against resistance. The brachioradialis reflex is 1+ on the left and 2+ on the right. The radial pulse is palpable bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Carpal tunnel syndrome
- B. Syringomyelia
- C. Amyotrophic lateral sclerosis
- D. C5-C6 disc herniation (Correct Answer)
- E. Thoracic outlet syndrome
Upper limb cross-sections Explanation: ***C5-C6 disc herniation***
- The patient's symptoms of neck, shoulder, and arm pain, along with paresthesias radiating to the **radial aspect of the forearm, thumb, and index finger**, are consistent with **C6 dermatomal distribution**.
- The positive **Spurling's maneuver** (extension, rotation, and downward pressure causing paresthesias) and decreased **brachioradialis reflex** (C5-C6 reflex) strongly suggest **cervical radiculopathy**, most likely due to a disc herniation affecting the C6 nerve root.
*Carpal tunnel syndrome*
- Characterized by **median nerve compression** at the wrist, causing paresthesias and pain primarily in the **thumb, index, middle, and radial half of the ring finger**, typically worsening at night.
- Would not explain the neck, shoulder, or upper arm pain, or the positive Spurling's maneuver, which indicates a more proximal nerve root compression.
*Syringomyelia*
- A rare chronic progressive disorder where a **syrinx (fluid-filled cyst)** forms within the spinal cord, often presenting with a **cape-like distribution of sensory loss** (loss of pain and temperature sensation) over the shoulders and upper extremities.
- Motor weakness can occur but the pain and paresthesia pattern, along with the positive Spurling's maneuver, are not typical for syringomyelia.
*Amyotrophic lateral sclerosis*
- A progressive neurodegenerative disease affecting **upper and lower motor neurons**, leading to widespread muscle weakness, atrophy, fasciculations, and spasticity.
- It does not typically present with acute, radicular pain and paresthesias restricted to a specific dermatome, and sensory involvement is absent.
*Thoracic outlet syndrome*
- Involves compression of the **brachial plexus** and/or subclavian vessels in the thoracic outlet, causing neurogenic symptoms (pain, paresthesias) primarily in the **ulnar nerve distribution** and vascular symptoms (edema, discoloration).
- The pain and paresthesias in the radial aspect of the hand and forearm, along with the specific reflex changes and positive neck maneuver, are not characteristic of thoracic outlet syndrome.
Upper limb cross-sections US Medical PG Question 3: A 25-year-old woman comes to the physician because of pain and weakness in her right forearm and hand for several months. Two years ago, she sustained a fracture of her ulnar shaft with dislocation of the radial head that was treated surgically. Physical examination shows mild tenderness a few centimeters distal to the lateral epicondyle. She has marked weakness when attempting to extend her right middle finger. There is radial deviation on extension of the wrist. Sensation is not impaired. Which of the following nerves is most likely affected in this patient?
- A. Ulnar nerve
- B. Musculocutaneous nerve
- C. Posterior interosseous nerve (Correct Answer)
- D. Superficial radial nerve
- E. Anterior interosseous nerve
Upper limb cross-sections Explanation: ***Posterior interosseous nerve***
- The symptoms, including weakness in **middle finger extension** and **radial deviation of the wrist on extension**, are classic signs of **posterior interosseous nerve** (PIN) palsy. This nerve primarily innervates the muscles responsible for **finger and thumb extension**, as well as **extensor carpi ulnaris** (ECU) for wrist extension.
- The **radial deviation on wrist extension** occurs because the radial-sided wrist extensors (**extensor carpi radialis longus** and **brevis**) are innervated by the **radial nerve proper** before it branches into PIN, so they remain intact. With loss of ECU (ulnar-sided wrist extensor), unopposed action of ECRL and ECRB causes radial deviation.
- PIN palsy can result from **trauma** or compression, and the patient's history of a **radial head dislocation** two years prior is a significant risk factor for nerve damage in this region, particularly as PIN passes through the **supinator muscle** (arcade of Frohse). Tenderness distal to the **lateral epicondyle** also points to the region where PIN can be compressed.
*Ulnar nerve*
- An **ulnar nerve** injury would primarily cause weakness in **finger adduction and abduction** (especially the little finger and ring finger), **flexion of the ulnar half of the profundus**, and **intrinsic hand muscles**, leading to a "claw hand" deformity if severe.
- Sensation would also be affected in the **palmar and dorsal aspects of the 5th digit** and the **medial half of the 4th digit**, which is not described.
*Musculocutaneous nerve*
- The **musculocutaneous nerve** primarily innervates the **biceps brachii** and **brachialis muscles**, responsible for **elbow flexion** and **forearm supination**.
- Sensory deficits would be noted on the **lateral forearm**, none of which align with the patient's symptoms.
*Superficial radial nerve*
- The **superficial radial nerve** is purely sensory and provides sensation to the **dorsum of the hand** and parts of the thumb, index, and middle fingers.
- It does not have any motor function, so motor weakness would not be a symptom of its injury.
*Anterior interosseous nerve*
- The **anterior interosseous nerve** (AIN) is a purely motor branch of the median nerve, responsible for innervating the **flexor pollicis longus**, **flexor digitorum profundus (index and middle fingers)**, and **pronator quadratus**.
- Injury to the AIN would result in an inability to form an "OK" sign (due to impaired flexion of the thumb IP joint and index finger DIP joint) and no sensory loss.
Upper limb cross-sections US Medical PG Question 4: A 30-year-old man presents with weakness in his right hand. He says he has been an avid cyclist since the age of 20. He denies any recent trauma. Physical examination reveals decreased sensations over the 4th and 5th digits with difficulty extending the 4th and 5th digits. Strength is 4 out of 5 in the extensor muscles of the right hand and wrist. When the patient is asked to extend his fingers, the result is shown in the image. Which of the following nerves is most likely damaged in this patient?
- A. Median nerve
- B. Musculocutaneous nerve
- C. Axillary nerve
- D. Ulnar nerve (Correct Answer)
- E. Radial nerve
Upper limb cross-sections Explanation: ***Ulnar nerve***
- The symptoms, including weakness in the **right hand**, decreased sensation over the **4th and 5th digits**, and difficulty extending the 4th and 5th digits (which suggests **ulnar claw**), are characteristic of **ulnar nerve damage**.
- **Avid cycling** can lead to compression of the ulnar nerve in the **Guyon's canal** (handlebar palsy) or at the **cubital tunnel** in the elbow, causing these specific signs.
*Median nerve*
- Damage to the median nerve typically affects the **thumb**, **index**, **middle finger**, and radial half of the ring finger, causing **ape hand deformity** or **carpal tunnel syndrome**.
- It controls movements like **thumb opposition** and **flexion of the first three digits**, which are not primarily described as impaired here.
*Musculocutaneous nerve*
- This nerve primarily innervates the **biceps brachii**, **brachialis**, and **coracobrachialis muscles**, affecting **elbow flexion** and **forearm supination**.
- It provides sensory innervation to the **lateral forearm**, symptoms not consistent with this patient's presentation.
*Axillary nerve*
- Damage to the axillary nerve results in weakness of the **deltoid** and **teres minor muscles**, leading to impaired **shoulder abduction** and external rotation.
- Sensory loss would be over the **lateral aspect of the shoulder**, which is unrelated to the described hand symptoms.
*Radial nerve*
- Radial nerve damage typically results in **wrist drop** and impaired **extension of the fingers and thumb** due to innervation of the extensors.
- While there is difficulty extending the 4th and 5th digits, the sensory loss pattern (4th and 5th digits) and specific **ulnar claw** appearance are more indicative of ulnar nerve involvement.
Upper limb cross-sections US Medical PG Question 5: A 61-year-old woman comes to the physician for a follow-up examination 1 week after undergoing right-sided radical mastectomy and axillary lymph node dissection for breast cancer. She says that she has been unable to comb her hair with her right hand since the surgery. Physical examination shows shoulder asymmetry. She is unable to abduct her right arm above 90 degrees. When she pushes against a wall, there is protrusion of the medial aspect of the right scapula. Injury to which of the following nerves is the most likely cause of this patient's condition?
- A. Long thoracic nerve (Correct Answer)
- B. Thoracodorsal nerve
- C. Axillary nerve
- D. Suprascapular nerve
- E. Upper trunk of the brachial plexus
Upper limb cross-sections Explanation: ***Long thoracic nerve***
- Injury to the **long thoracic nerve** leads to paralysis of the **serratus anterior muscle**, causing **scapular winging** (protrusion of the medial scapula) especially when pushing against a wall.
- The serratus anterior is crucial for **scapular protraction** and stabilizing the scapula during **abduction of the arm above 90 degrees**, explaining her inability to comb her hair.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, which is responsible for **adduction**, extension, and internal rotation of the arm.
- Injury to this nerve would primarily affect these movements, not shoulder abduction above 90 degrees or scapular winging.
*Axillary nerve*
- The **axillary nerve** innervates the **deltoid muscle** and **teres minor**.
- Damage would primarily result in impaired **arm abduction up to 90 degrees** and loss of sensation over the lateral shoulder, but not scapular winging.
*Suprascapular nerve*
- The **suprascapular nerve** supplies the **supraspinatus** and **infraspinatus muscles**, which are involved in the initiation of arm abduction and external rotation, respectively.
- Injury would cause weakness in these movements and shoulder pain, but not scapular winging.
*Upper trunk of the brachial plexus*
- Injury to the **upper trunk of the brachial plexus** (C5-C6) affects several nerves and muscles, leading to conditions like **Erb's palsy**.
- While it can impair shoulder function and abduction, the specific finding of scapular winging points more directly to long thoracic nerve damage rather than a generalized upper trunk injury, as the long thoracic nerve (C5-C7) is often spared in classic Erb's palsy.
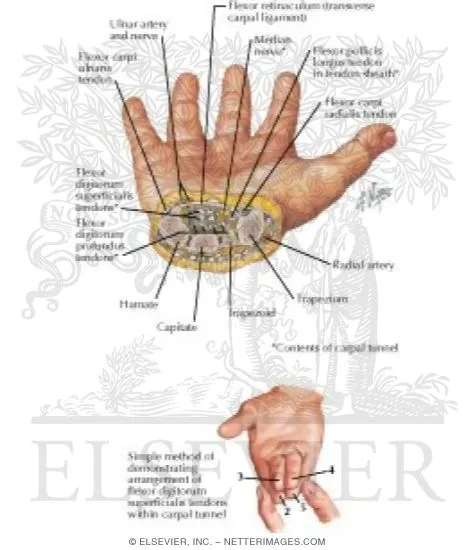
Upper limb cross-sections US Medical PG Question 6: A 61-year-old woman comes to her physician for a burning sensation and numbness in her right hand for 4 weeks. The burning sensation is worse at night and is sometimes relieved by shaking the wrist. In the past week, she has noticed an exacerbation of her symptoms. She has rheumatoid arthritis and type 2 diabetes mellitus. Her medications include insulin, methotrexate, and naproxen. Her vital signs are within normal limits. Examination shows swan neck deformities of the fingers on both hands and multiple subcutaneous nodules over bilateral olecranon processes. There is tingling and numbness over the right thumb, index finger, and middle finger when the wrist is actively flexed. The remainder of the examination shows no abnormalities. Which of the following is the most appropriate next best step in management?
- A. Initiate sulfasalazine therapy
- B. Volar splinting (Correct Answer)
- C. Vitamin B6 supplementation
- D. Initiate azathioprine therapy
- E. Physiotherapy
Upper limb cross-sections Explanation: ***Volar splinting***
- The patient presents with classic symptoms of **carpal tunnel syndrome (CTS)**, including burning, numbness, and tingling in the distribution of the **median nerve** (thumb, index, and middle fingers), worse at night, and relieved by shaking the wrist (**flick sign**).
- **Volar splinting** of the wrist in a neutral position is the first-line treatment for CTS as it reduces pressure on the median nerve, particularly at night.
*Initiate sulfasalazine therapy*
- **Sulfasalazine** is a **disease-modifying antirheumatic drug (DMARD)** used to treat rheumatoid arthritis, but it would not address the acute symptoms of carpal tunnel syndrome.
- The patient is already on **methotrexate**, another DMARD, and there is no indication that her rheumatoid arthritis is poorly controlled in a way that would necessitate adding another DMARD for joint inflammation, separate from her neuropathic symptoms.
*Vitamin B6 supplementation*
- **Vitamin B6 (pyridoxine)** supplementation is sometimes considered for peripheral neuropathies, but there is no strong evidence for its efficacy in treating typical carpal tunnel syndrome.
- While some studies have explored its use in specific cases, it is not a recommended first-line treatment for CTS and is not as effective as splinting.
*Initiate azathioprine therapy*
- **Azathioprine** is an **immunosuppressant** and DMARD used in the treatment of more severe rheumatoid arthritis or when other DMARDs are ineffective.
- Similar to sulfasalazine, it would target systemic inflammation related to rheumatoid arthritis but would not directly treat the localized nerve compression causing carpal tunnel syndrome.
*Physiotherapy*
- While **physiotherapy** can be beneficial for strengthening and improving flexibility in the hand and wrist, it is generally considered a supportive therapy for carpal tunnel syndrome and is not typically the first-line management for acute symptoms.
- **Volar splinting** is usually initiated first to stabilize the wrist and reduce nerve compression, with physiotherapy potentially added later as part of a comprehensive treatment plan or if splinting alone is insufficient.
Upper limb cross-sections US Medical PG Question 7: A 25-year-old man was referred to a neurologist for right-hand weakness. He was involved in a motor vehicle accident 2 months ago in which his right hand was injured. On examination, his grip is weak, especially in fingers 2, 4, and 5 and he is unable to adduct these fingers. Which of the following groups of muscles is most likely affected?
- A. Flexor digitorum profundus
- B. Palmar interossei muscles (Correct Answer)
- C. Lumbrical muscles
- D. Dorsal interossei muscles
- E. Extensor digitorum
Upper limb cross-sections Explanation: ***Palmar interossei muscles***
- The inability to **adduct fingers 2, 4, and 5** (index, ring, and pinky fingers) is the key finding. The **palmar interossei** are responsible for adduction of these fingers towards the middle finger.
- Weak grip in these specific fingers indicates impairment of the muscles controlling their movement and adduction, which are primarily the palmar interossei.
*Flexor digitorum profundus*
- The **flexor digitorum profundus** primarily **flexes the distal interphalangeal (DIP) joints** of the fingers, as well as assists in flexing the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints.
- While it contributes to grip strength, its primary role is flexion, not adduction, and weakness would typically present as difficulty with deep finger flexion rather than specific adduction issues.
*Lumbrical muscles*
- The **lumbrical muscles** **flex the metacarpophalangeal (MCP) joints** and **extend the interphalangeal (IP) joints**. This action is characteristic of the "lumbrical grip" or "writing position."
- Their primary function does not involve adduction of the fingers, and their weakness would manifest differently.
*Dorsal interossei muscles*
- The **dorsal interossei muscles** are responsible for **abduction of the fingers** (spreading them apart).
- The patient's inability to adduct fingers rules out the dorsal interossei as the primary affected group, as these muscles perform the opposite action.
*Extensor digitorum*
- The **extensor digitorum** primarily **extends the metacarpophalangeal (MCP) and interphalangeal (IP) joints** of the medial four fingers.
- Weakness in this muscle would result in difficulty extending the fingers, leading to a "dropped finger" appearance or inability to straighten the fingers, which is contrary to the described adduction deficit.
Upper limb cross-sections US Medical PG Question 8: A 47-year-old woman presents to her primary care provider because of numbness and tingling on the palmar aspects of both hands. She denies any symptoms at the base of her thumbs. The symptoms are worse on the right (dominant hand) and are increased with activities such as driving or brushing her hair. She frequently wakes up with pain and has to shake her hand for pain relief. She has had rheumatoid arthritis for 9 years, for which she takes methotrexate. Her blood pressure is 124/76 mm Hg, the heart rate is 75/min, and the respiratory rate is 15/min. Lightly tapping over the middle of the anterior aspect of the right wrist leads to a tingling sensation in the palm. In this patient, electromyography (EMG) will most likely show which of the following results?
- A. Neuropathic changes in the palmar branch of the median nerve
- B. Denervation in C7 innervated paraspinal, arms, and shoulder muscles
- C. Focal slowing of conduction velocity in the median nerve in the carpal tunnel (Correct Answer)
- D. Widespread symmetrical neuropathic changes without focal abnormalities
- E. Widespread denervation in proximal muscles with normal sensory nerves
Upper limb cross-sections Explanation: ***Focal slowing of conduction velocity in the median nerve in the carpal tunnel***
- The patient's symptoms (numbness, tingling in palmar hands, worsening with activity, nocturnal pain relieved by shaking, **Tinel's sign** at the wrist) are classic for **carpal tunnel syndrome (CTS)**, caused by compression of the **median nerve** at the wrist.
- **Electromyography (EMG)** and **nerve conduction studies (NCS)** are confirmatory tests for CTS, demonstrating slowed conduction velocity specifically through the carpal tunnel.
*Neuropathic changes in the palmar branch of the median nerve*
- The **palmar cutaneous branch** of the median nerve typically branches off **proximal to the carpal tunnel** and supplies sensation to the base of the thumb.
- Since the patient specifically denies symptoms at the base of her thumbs, isolated involvement of the palmar cutaneous branch is unlikely in this case, pointing to compression within the carpal tunnel.
*Denervation in C7 innervated paraspinal, arms, and shoulder muscles*
- **C7 radiculopathy** would involve symptoms in the C7 dermatome and myotome, potentially affecting muscles in the arm and shoulder.
- Her symptoms are primarily wrist and hand-focused, without signs of cervical spine involvement or widespread muscle weakness.
*Widespread symmetrical neuropathic changes without focal abnormalities*
- This pattern suggests a **generalized peripheral neuropathy**, which would likely present with more diffuse and possibly symmetrical symptoms, often involving the feet first.
- This patient's symptoms are distinctly focal and related to the distribution of the median nerve in the hand.
*Widespread denervation in proximal muscles with normal sensory nerves*
- This presentation is more consistent with a **motor neuron disease** or a **myopathy**, where there is primarily motor involvement and sensory nerves are typically spared.
- The patient's primary symptoms are sensory (numbness and tingling), and there is no indication of widespread muscle weakness or atrophy typical of denervation in proximal muscles.
Upper limb cross-sections US Medical PG Question 9: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Upper limb cross-sections Explanation: ***Teres minor***
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
Upper limb cross-sections US Medical PG Question 10: A 35-year-old man is brought to the trauma bay by ambulance after sustaining a gunshot wound to the right arm. The patient is in excruciating pain and states that he can't move or feel his hand. The patient states that he has no other medical conditions. On exam, the patient's temperature is 98.4°F (36.9°C), blood pressure is 140/86 mmHg, pulse is 112/min, and respirations are 14/min. The patient is alert and his Glasgow coma scale is 15. On exam, he has a single wound on his right forearm without continued bleeding. The patient has preserved motor and sensation in his right elbow; however, he is unable to extend his wrist or extend his fingers further. He is able to clench his hand, but this is limited by pain. On sensory exam, the patient has no sensation to the first dorsal web space but has preserved sensation on most of the volar surface. Which of the following structures is most likely injured?
- A. Recurrent motor branch of the median nerve
- B. Main median nerve
- C. Lower trunk
- D. Ulnar nerve
- E. Radial nerve (Correct Answer)
Upper limb cross-sections Explanation: ***Radial nerve***
- The inability to **extend the wrist and fingers** (wrist drop) is a classic sign of **radial nerve injury**, as it innervates the extensors of the forearm and hand.
- **Loss of sensation in the first dorsal web space** is also characteristic of radial nerve damage, as this area is supplied by the superficial radial nerve.
*Recurrent motor branch of the median nerve*
- This nerve primarily innervates the **thenar muscles** (flexor pollicis brevis, abductor pollicis brevis, opponens pollicis), affecting **thumb opposition**.
- Injury would primarily lead to **weakness in thumb movements**, not wrist or finger extension, and would spare sensation in the first dorsal web space.
*Main median nerve*
- The median nerve primarily innervates the **flexors of the forearm and hand**, and contributes to sensation on the **volar aspect of the thumb**, index, middle, and radial half of the ring finger.
- Injury would cause difficulty with **flexion of the wrist and fingers**, and loss of sensation on the volar surface, which is largely preserved in this patient.
*Lower trunk*
- The lower trunk of the brachial plexus (C8-T1) gives rise to the ulnar nerve and part of the median nerve, affecting **flexion of the wrist and fingers**, and intrinsic hand muscles.
- Injury would result in more widespread weakness affecting the **intrinsic hand muscles** and flexion, and would include sensory loss in the **ulnar nerve distribution**, which is not described.
*Ulnar nerve*
- The ulnar nerve primarily innervates the **intrinsic hand muscles** (excluding the thenar group) and the **flexor carpi ulnaris** and **medial half of flexor digitorum profundus**.
- Injury would typically cause **weakness in intrinsic hand functions** (e.g., finger abduction/adduction, ring and little finger flexion) and sensory loss on the **ulnar side of the hand**, not the dorsal web space.
More Upper limb cross-sections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
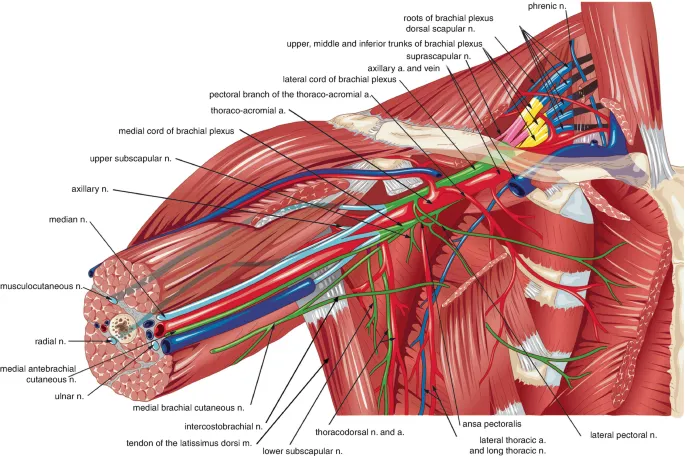 \n\nKey structures organized around the axillary artery, all enclosed within the axillary sheath.\n\n* Neurovascular Bundle:\n - Axillary Artery: Central reference point.\n - Brachial Plexus Cords: Named by their position relative to the axillary artery (Lateral, Medial, Posterior).\n - Axillary Vein: Medial to the axillary artery.\n* Muscular Walls:\n - Anterior: Pectoralis major & minor.\n - Posterior: Subscapularis, Teres major, Latissimus dorsi.\n - Medial: Serratus anterior.\n - Lateral: Intertubercular sulcus of the humerus.\n\n> ⭐ The axillary sheath is a fascial sleeve enclosing the axillary artery, vein, and brachial plexus. Anesthetic injected here for an axillary block anesthetizes the terminal nerves (musculocutaneous, median, ulnar, radial) but often spares the axillary nerve.
\n\nKey structures organized around the axillary artery, all enclosed within the axillary sheath.\n\n* Neurovascular Bundle:\n - Axillary Artery: Central reference point.\n - Brachial Plexus Cords: Named by their position relative to the axillary artery (Lateral, Medial, Posterior).\n - Axillary Vein: Medial to the axillary artery.\n* Muscular Walls:\n - Anterior: Pectoralis major & minor.\n - Posterior: Subscapularis, Teres major, Latissimus dorsi.\n - Medial: Serratus anterior.\n - Lateral: Intertubercular sulcus of the humerus.\n\n> ⭐ The axillary sheath is a fascial sleeve enclosing the axillary artery, vein, and brachial plexus. Anesthetic injected here for an axillary block anesthetizes the terminal nerves (musculocutaneous, median, ulnar, radial) but often spares the axillary nerve.