Upper abdominal cross-sections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper abdominal cross-sections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
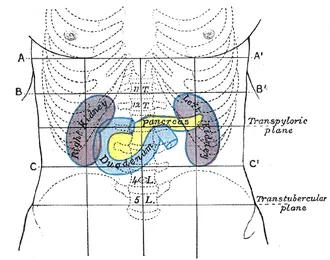
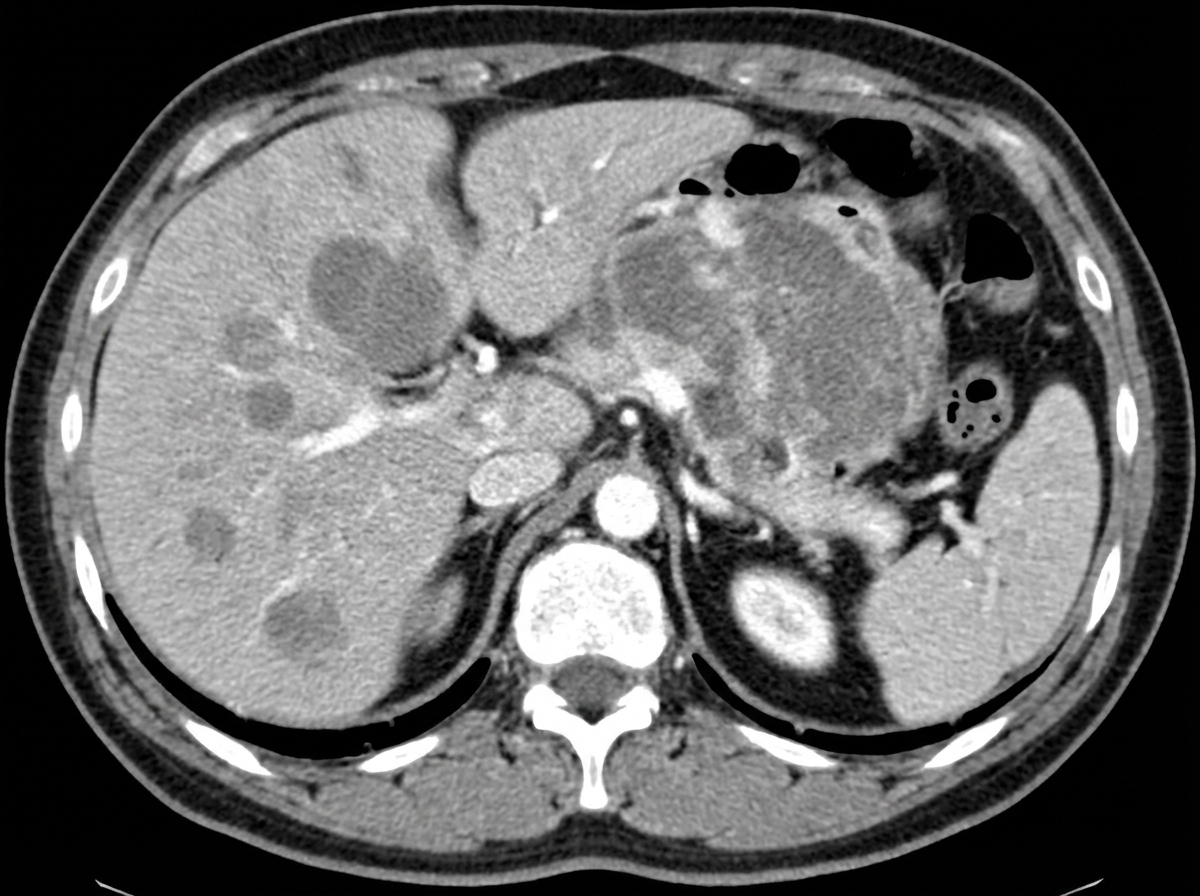
Upper abdominal cross-sections US Medical PG Question 1: A 40-year-old man presents with severe fatigue, dyspnea on exertion, and weight loss. He reports a weight loss of 15 kg (33.0 lb) over the past 3 months and feels full almost immediately after starting to eat, often feeling nauseous and occasionally vomiting. Past medical history is not significant. However, the patient reports a 10-pack-year smoking history. His temperature is 37.0°C (98.6°F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Physical examination reveals paleness and conjunctival pallor. Abdominal examination reveals an ill-defined nontender mass in the epigastric region along with significant hepatomegaly. Routine laboratory studies show a hemoglobin level of 7.2 g/dL. A contrast CT scan of the abdomen is presented below. Which of the following structures is most helpful in the anatomical classification of gastrointestinal bleeding in this patient?
- A. Ampulla of Vater
- B. Hepatoduodenal ligament
- C. Ligament of Treitz (Correct Answer)
- D. Portal vein
- E. Sphincter of Oddi
Upper abdominal cross-sections Explanation: ***Ligament of Treitz***
- The **ligament of Treitz** is a key anatomical landmark that divides the gastrointestinal tract into the upper and lower GI systems.
- Bleeding proximal to this ligament is considered **upper GI bleeding**, while bleeding distal to it is **lower GI bleeding**. This distinction helps narrow down potential causes and guide diagnostic procedures.
*Ampulla of Vater*
- The **Ampulla of Vater** is the junction of the common bile duct and pancreatic duct, emptying into the second part of the duodenum.
- While it can be a source of bleeding (e.g., from an eroded tumor or bleeding peptic ulcer), it is within the upper GI tract and does not serve as a primary dividing line for anatomical classification of GI bleeding as a whole.
*Hepatoduodenal ligament*
- The **hepatoduodenal ligament** contains the portal triad (hepatic artery, portal vein, and common bile duct).
- It does not serve as an anatomical landmark for classifying GI bleeding into upper and lower components.
*Portal vein*
- The **portal vein** carries blood from the GI tract and spleen to the liver.
- It is involved in conditions that can cause GI bleeding (e.g., portal hypertension leading to varices), but it is a blood vessel and not a structural landmark for classifying bleeding into upper vs. lower GI.
*Sphincter of Oddi*
- The **Sphincter of Oddi** controls the flow of bile and pancreatic secretions into the duodenum at the Ampulla of Vater.
- Like the Ampulla of Vater, it is an upper GI structure and does not provide an anatomical classification for differentiating between upper and lower GI bleeding.
Upper abdominal cross-sections US Medical PG Question 2: A 32-year-old man presents to his primary care physician complaining of pain accompanied by a feeling of heaviness in his scrotum. He is otherwise healthy except for a broken arm he obtained while skiing several years ago. Physical exam reveals an enlarged “bag of worms” upon palpation of the painful scrotal region. Shining a light over this area shows that the scrotum does not transilluminate. Which of the following statements is true about the most likely cause of this patient's symptoms?
- A. Equally common on both sides
- B. More common on left due to drainage into renal vein (Correct Answer)
- C. More common on right due to drainage into renal vein
- D. More common on right due to drainage into inferior vena cava
- E. More common on left due to drainage into inferior vena cava
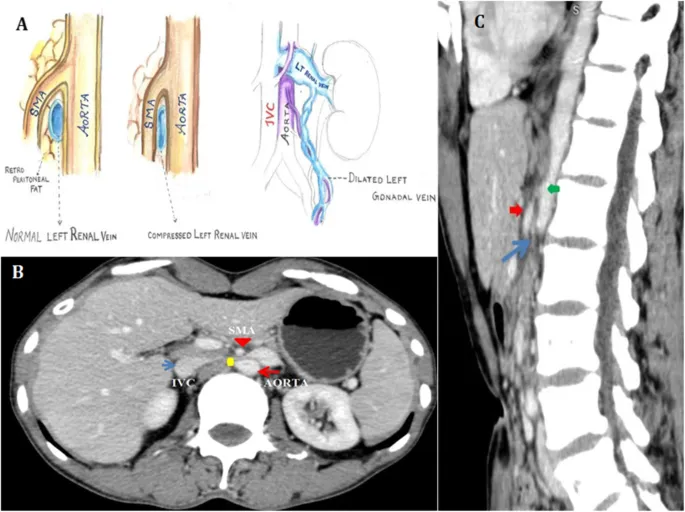
Upper abdominal cross-sections Explanation: ***More common on left due to drainage into renal vein***
- The patient's symptoms of scrotal pain, "bag of worms" on palpation, and lack of transillumination are classic for a **left-sided varicocele**.
- The longer course and perpendicular drainage of the **left testicular vein** into the left renal vein create higher pressure, making varicocele formation more common on the left.
*Equally common on both sides*
- Varicoceles are distinctly asymmetrical, with a well-established higher incidence on the left side due to anatomical differences.
- Bilateral varicoceles can occur but are less common than isolated left-sided ones and do not support an "equally common" distribution.
*More common on right due to drainage into renal vein*
- The right testicular vein typically drains directly into the **inferior vena cava (IVC)**, not the renal vein, which is a lower pressure system compared to the left.
- Therefore, anatomical factors do not favor varicocele formation on the right side due to drainage into the renal vein.
*More common on right due to drainage into inferior vena cava*
- While the right testicular vein drains into the IVC, this direct drainage path is associated with good venous return and a lower risk of varicocele.
- A right-sided varicocele is less common and, if present, should prompt investigation for retroperitoneal mass obstructing the IVC or right testicular vein.
*More common on left due to drainage into inferior vena cava*
- The left testicular vein typically drains into the **left renal vein**, not directly into the inferior vena cava.
- This anatomical description is incorrect and does not explain the higher incidence of left-sided varicoceles.
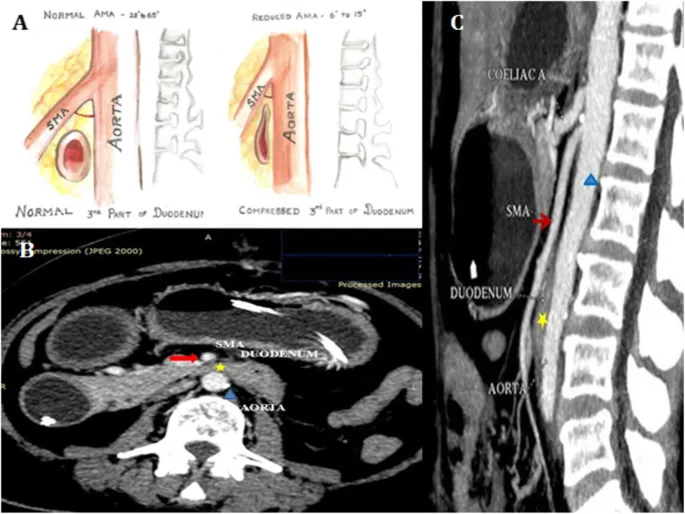
Upper abdominal cross-sections US Medical PG Question 3: A 53-year-old woman presents to the office complaining of an extreme, nonradiating stabbing pain in the epigastric region after having a meal. She states that it has happened several times in the past week approximately 30 minutes after eating and spontaneously resolves. A day before, the patient went to urgent care with the same complaint, but the abdominal X-ray was normal. Surgical history is remarkable for a total knee arthroplasty procedure 6 months ago. She has lost 34 kg (75 lb) since the operation because of lifestyle changes. The vital signs are normal. Laparoscopic surgical scars are well healed. Endoscopy shows benign mucosa to the proximal duodenum. A barium swallow study reveals an extremely narrowed duodenum. Which of the following structures is most likely responsible for this patient’s current symptoms?
- A. Superior mesenteric artery (Correct Answer)
- B. Gastroduodenal artery
- C. Inferior mesenteric artery
- D. Gallbladder
- E. Pylorus of the stomach
Upper abdominal cross-sections Explanation: ***Superior mesenteric artery***
- This patient's symptoms (postprandial epigastric pain, significant weight loss, and narrowed duodenum) are highly suggestive of **superior mesenteric artery (SMA) syndrome**. Weight loss can reduce the **mesenteric fat pad**, decreasing the angle between the SMA and the aorta, thereby compressing the third part of the duodenum.
- The narrow angle between the **aorta** and the **superior mesenteric artery** entraps the third portion of the duodenum, causing a functional obstruction, which explains the pain after meals when food distends the narrowed duodenum.
*Gastroduodenal artery*
- The gastroduodenal artery originates from the **common hepatic artery** and typically passes anterior to the duodenum, making it unlikely to cause compression.
- Compression by the gastroduodenal artery is not a recognized cause of **duodenal obstruction** or postprandial pain in this context.
*Inferior mesenteric artery*
- The **inferior mesenteric artery** supplies blood to the distal colon and rectum; its anatomical position is far from the duodenum.
- It does not cross or impinge upon the duodenum and therefore cannot cause **duodenal compression** or the described symptoms.
*Gallbladder*
- Gallbladder issues (e.g., **cholelithiasis**, **cholecystitis**) would typically cause **right upper quadrant pain**, possibly radiating to the back or shoulder, and often associated with fatty meals, but less likely to manifest as extreme epigastric pain 30 minutes post-meal with duodenal narrowing.
- The imaging findings of a narrowed duodenum and the pattern of pain are not characteristic of **gallbladder pathology**.
*Pylorus of the stomach*
- **Pyloric stenosis** would cause symptoms of gastric outlet obstruction, including **vomiting of undigested food**, early satiety, and weight loss, but the endoscopy showed benign mucosa to the proximal duodenum and the barium swallow revealed duodenal narrowing, not pyloric.
- While pyloric issues can cause postprandial symptoms, the **specific finding of a narrowed duodenum** points away from it as the primary cause in this case.
Upper abdominal cross-sections US Medical PG Question 4: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
Upper abdominal cross-sections Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
Upper abdominal cross-sections US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Upper abdominal cross-sections Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Upper abdominal cross-sections US Medical PG Question 6: A 51-year-old homeless man presents to the emergency department with severe abdominal pain and cramping for the past 3 hours. He endorses radiation to his back. He adds that he vomited multiple times. He admits having been hospitalized repeatedly for alcohol intoxication and abdominal pain. His temperature is 103.8° F (39.8° C), respiratory rate is 15/min, pulse is 107/min, and blood pressure is 100/80 mm Hg. He refuses a physical examination due to severe pain. Blood work reveals the following:
Serum:
Albumin: 3.2 gm/dL
Alkaline phosphatase: 150 U/L
Alanine aminotransferase: 76 U/L
Aspartate aminotransferase: 155 U/L
Gamma-glutamyl transpeptidase: 202 U/L
Lipase: 800 U/L
What is the most likely diagnosis of this patient?
- A. Duodenal peptic ulcer
- B. Choledocholithiasis
- C. Pancreatitis (Correct Answer)
- D. Cholecystitis
- E. Gallbladder cancer
Upper abdominal cross-sections Explanation: ***Pancreatitis***
- The patient's history of **repeated alcohol intoxication** and abdominal pain, combined with **severe abdominal pain radiating to the back**, vomiting, and significantly elevated **lipase (800 U/L)**, are highly indicative of **acute pancreatitis**.
- The elevated **liver enzymes (ALT, AST, GGT)** and **alkaline phosphatase** can be associated with cholestasis or liver involvement often seen in alcohol-induced pancreatitis or can be elevated due to a gallstone lodged in the common bile duct, which is also a common cause of pancreatitis.
*Duodenal peptic ulcer*
- While duodenal ulcers cause severe abdominal pain, they typically present with **epigastric pain** that may be relieved by food, and often cause **melena or hematemesis** if bleeding.
- The extremely high **lipase level** and pain radiating to the back are not characteristic of an uncomplicated duodenal ulcer.
*Choledocholithiasis*
- **Choledocholithiasis** (gallstones in the common bile duct) can cause severe right upper quadrant or epigastric pain and elevated liver enzymes, but it doesn't typically present with an isolated, dramatically high **lipase** level without concomitant pancreatitis.
- The main symptom is **biliary colic**, often post-prandial, and usually involves jaundice or cholangitis if infected.
*Cholecystitis*
- **Cholecystitis** presents with **right upper quadrant pain**, often radiating to the shoulder, associated with fever and nausea, and is usually triggered by fatty meals.
- Although there might be some elevation in liver enzymes and amylase/lipase, the **markedly elevated lipase** and pain radiating to the back are more suggestive of pancreatitis.
*Gallbladder cancer*
- **Gallbladder cancer** typically presents with more insidious symptoms, such as chronic right upper quadrant pain, weight loss, jaundice, and anorexia.
- It would not usually present with an acute episode of **severe abdominal pain and drastically high lipase** in this manner.
Upper abdominal cross-sections US Medical PG Question 7: A 30-year-old man comes to the physician because of an episode of bloody vomiting this morning and a 1-week history of burning upper abdominal pain. Two weeks ago, he sustained a head injury and was in a coma for 3 days. An endoscopy shows multiple, shallow hemorrhagic lesions predominantly in the gastric fundus and greater curvature. Biopsies show patchy loss of epithelium and an acute inflammatory infiltrate in the lamina propria that does not extend beyond the muscularis mucosa. Which of the following is the most likely diagnosis?
- A. Type B gastritis
- B. Cushing ulcer (Correct Answer)
- C. Erosive gastritis
- D. Dieulafoy lesion
- E. Penetrating ulcer
Upper abdominal cross-sections Explanation: ***Cushing ulcer***
- A **Cushing ulcer** is a type of **stress ulcer** specifically associated with **intracranial injury**, which causes increased vagal stimulation leading to hypersecretion of gastric acid.
- The patient's history of a **head injury** followed by **bloody vomiting** and **upper abdominal pain**, along with endoscopic findings of shallow, hemorrhagic lesions, is highly consistent with a Cushing ulcer.
*Type B gastritis*
- **Type B gastritis** is primarily caused by **Helicobacter pylori infection**, often leading to chronic inflammation and sometimes ulcers, not acute stress-related lesions after a head injury.
- While it can cause epigastric pain and bleeding, the strong association with a recent head injury makes Cushing ulcer a more specific diagnosis.
*Erosive gastritis*
- **Erosive gastritis** is a broad term encompassing various causes of gastric mucosal erosions, including NSAIDs, alcohol, and stress.
- While Cushing ulcer represents a specific form of stress-related erosive gastritis, **Cushing ulcer is the most specific and accurate diagnosis** given the distinct history of intracranial injury and coma.
- The temporal relationship between head trauma and gastric symptoms is pathognomonic for Cushing ulcer.
*Dieulafoy lesion*
- A **Dieulafoy lesion** is characterized by an abnormally large submucosal artery that erodes the overlying mucosa, leading to sudden, massive gastrointestinal bleeding.
- This condition is typically isolated, not presenting with multiple, shallow hemorrhagic lesions across the gastric fundus and greater curvature, and is not directly linked to head injury.
*Penetrating ulcer*
- A **penetrating ulcer** is a complication of a chronic peptic ulcer where the ulcer extends beyond the muscularis propria into adjacent organs.
- The biopsy findings of inflammation not extending beyond the **muscularis mucosa** indicate superficial damage (erosions), not a deep penetrating ulcer.
Upper abdominal cross-sections US Medical PG Question 8: A 22-year-old Caucasian male is stabbed in his left flank, injuring his left kidney. As the surgeon undertakes operative repair, she reviews relevant renal anatomy. All of the following are correct regarding the left kidney EXCEPT?
- A. The left kidney has a longer renal vein than the right kidney
- B. The left kidney underlies the left 12th rib
- C. The left kidney moves vertically during deep breathing
- D. The left kidney has a longer renal artery than the right kidney (Correct Answer)
- E. The left kidney lies between T12 and L3
Upper abdominal cross-sections Explanation: ***The left kidney has a longer renal artery than the right kidney***
- The **aorta** lies to the left of the midline, so the **right renal artery** must traverse a greater distance to reach the right kidney.
- Therefore, the right renal artery is longer than the left renal artery.
*The left kidney has a longer renal vein than the right kidney*
- The **inferior vena cava (IVC)** is positioned to the right of the midline, requiring the **left renal vein** to cross the aorta to drain.
- This anatomical arrangement makes the left renal vein longer than the right renal vein.
*The left kidney underlies the left 12th rib*
- The kidneys are retroperitoneal organs, and the 12th rib provides significant posterior protection for **both kidneys**.
- The superior pole of the left kidney typically extends to the level of the **11th and 12th ribs**.
*The left kidney moves vertically during deep breathing*
- The kidneys are surrounded by **perirenal fat** and are influenced by the diaphragm's movement.
- During **deep inspiration**, the diaphragm descends, causing both kidneys to move vertically by 2-3 cm.
*The left kidney lies between T12 and L3*
- The kidneys are situated in the retroperitoneum, generally extending from the level of the **T12 vertebra** to the **L3 vertebra**.
- The left kidney is typically positioned slightly higher than the right kidney.
Upper abdominal cross-sections US Medical PG Question 9: A 45-year-old male is brought to the emergency department by emergency medical services after sustaining a gunshot wound to the abdomen. He is unresponsive. His temperature is 99.0°F (37.2°C), blood pressure is 95/58 mmHg, pulse is 115/min, and respirations are 20/min. Physical examination reveals an entry wound in the left abdominal quadrant just inferior to the left lateral costal border. Abdominal CT shows the bullet trajectory through the left abdominal cavity. Which of the following structures has the bullet most likely penetrated?
- A. Transverse colon
- B. Ascending colon
- C. Descending colon (Correct Answer)
- D. Sigmoid colon
- E. Superior duodenum
Upper abdominal cross-sections Explanation: ***Descending colon***
- The **descending colon** is located in the left abdominal cavity, specifically in the left upper quadrant and extending into the left lower quadrant, making it highly susceptible to injury from a gunshot wound in the **left abdominal quadrant** just inferior to the left lateral costal border.
- Its position aligns directly with the described entry point and bullet trajectory.
*Transverse colon*
- The **transverse colon** lies more centrally in the upper abdomen, spanning from the right to the left upper quadrants.
- While possible to be hit by a left-sided entry wound, the trajectory described as "inferior to the left lateral costal border" makes the descending colon a more direct and likely target.
*Ascending colon*
- The **ascending colon** is located in the **right abdominal cavity**, specifically in the right upper and lower quadrants.
- A wound inferior to the left lateral costal border would be on the opposite side of the abdomen and thus unlikely to penetrate the ascending colon.
*Sigmoid colon*
- The **sigmoid colon** is located more inferiorly in the **left lower quadrant** and pelvis.
- While on the left side, the entry wound described as "inferior to the left lateral costal border" is generally higher than the typical location of the sigmoid colon.
*Superior duodenum*
- The **superior duodenum** is located in the **right upper quadrant** of the abdomen, anterior to the head of the pancreas.
- Its position on the right side makes it highly unlikely to be penetrated by a gunshot wound to the left abdominal quadrant.
Upper abdominal cross-sections US Medical PG Question 10: A 55-year-old man comes to the physician because of a 3-week history of intermittent burning epigastric pain. His pain improves with antacid use and eating but returns approximately 2 hours following meals. He has a history of chronic osteoarthritis and takes ibuprofen daily. Upper endoscopy shows a deep ulcer located on the posterior wall of the duodenal bulb. This ulcer is most likely to erode into which of the following structures?
- A. Splenic vein
- B. Descending aorta
- C. Pancreatic duct
- D. Gastroduodenal artery (Correct Answer)
- E. Transverse colon
Upper abdominal cross-sections Explanation: ***Gastroduodenal artery***
- A deep ulcer on the **posterior wall of the duodenal bulb** is anatomically very close to the **gastroduodenal artery**.
- Erosion into this artery can lead to **life-threatening upper gastrointestinal bleeding**, a severe complication of peptic ulcer disease.
*Splenic vein*
- The **splenic vein** is located more posteriorly and superiorly, primarily in relation to the pancreas and spleen, making it less likely to be eroded by a duodenal bulb ulcer.
- While erosion into major vessels can occur, the gastroduodenal artery is in a much more direct and immediate proximity to the posterior duodenal bulb.
*Descending aorta*
- The **descending aorta** is a retroperitoneal structure located much more posteriorly and medially, far from the duodenal bulb.
- Erosion into the aorta is an extremely rare and catastrophic event, not typically associated with duodenal ulcers.
*Pancreatic duct*
- The **pancreatic duct** (Wirsung's duct) is located within the pancreas, which lies posterior to the duodenum. While a *deep* ulcer could hypothetically penetrate the pancreas, the primary structure at risk for hemorrhage from a posterior duodenal bulb ulcer is the gastroduodenal artery.
- Erosion into the pancreatic duct would likely cause **pancreatitis** or **fistula formation**, rather than acute hemorrhage.
*Transverse colon*
- The **transverse colon** is located inferior to the duodenum, separated by the greater omentum.
- Ulcers would typically erode anteriorly or directly posteriorly, not inferiorly into the transverse colon, which would involve fistula formation rather than arterial erosion.
More Upper abdominal cross-sections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.