Pelvic cross-sections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic cross-sections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
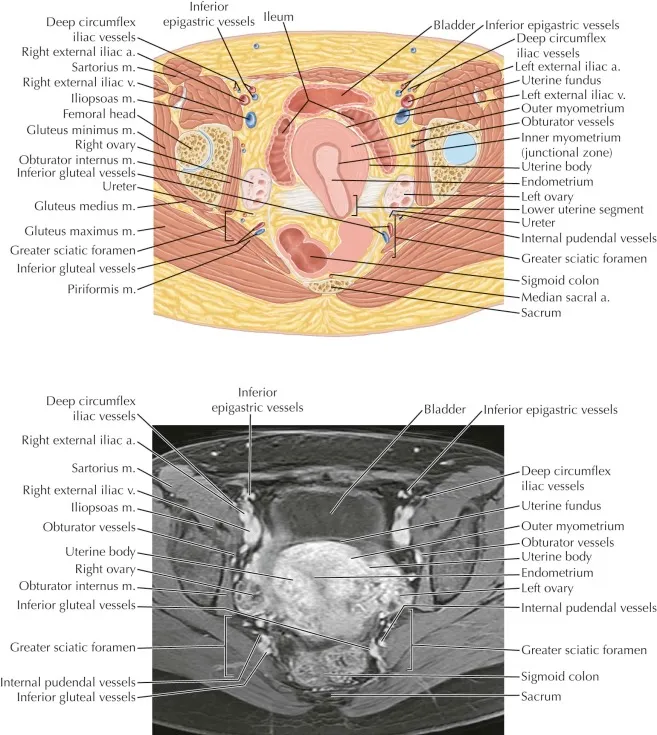
Pelvic cross-sections US Medical PG Question 1: A 60-year-old post-menopausal female presents to her gynecologist with vaginal bleeding. Her last period was over 10 years ago. Dilation and curettage reveals endometrial carcinoma so she is scheduled to undergo a total abdominal hysterectomy and bilateral salpingo-oophorectomy. During surgery, the gynecologist visualizes paired fibrous structures arising from the cervix and attaching to the lateral pelvic walls at the level of the ischial spines. Which of the following vessels is found within each of the paired visualized structure?
- A. Vaginal artery
- B. Superior vesical artery
- C. Uterine artery (Correct Answer)
- D. Artery of Sampson
- E. Ovarian artery
Pelvic cross-sections Explanation: ***Uterine artery***
- The paired fibrous structures described are the **cardinal ligaments (transverse cervical ligaments)**, which contain the **uterine arteries** as they course towards the uterus.
- The uterine artery, a branch of the **internal iliac artery**, crosses over the **ureter** within the cardinal ligament—a critical anatomical relationship during gynecological surgery ("water under the bridge").
- This is the primary vessel within the cardinal ligament and the key vascular structure at risk during hysterectomy.
*Vaginal artery*
- The vaginal artery typically branches from the **uterine artery** or directly from the **internal iliac artery**, but it is not the main vessel found within the cardinal ligament.
- It primarily supplies the **vagina**, not contained within the cardinal ligament support structure.
*Superior vesical artery*
- The superior vesical artery supplies the **upper part of the bladder** and originates from the **umbilical artery** (a branch of the internal iliac artery).
- It is not anatomically associated with the cardinal ligament or uterine support structures.
*Artery of Sampson*
- The Artery of Sampson is a branch of the **uterine artery** that anastomoses with the **ovarian artery** within the **broad ligament**, not the cardinal ligament.
- It is a minor vessel involved in the dual blood supply to the ovaries and uterus, not a primary structure within the cardinal ligament.
*Ovarian artery*
- The ovarian artery originates directly from the **abdominal aorta** and travels within the **suspensory ligament of the ovary (infundibulopelvic ligament)**, not the cardinal ligament.
- It supplies the **ovaries and fallopian tubes**, with a trajectory that is anatomically distinct from structures within the cardinal ligament.
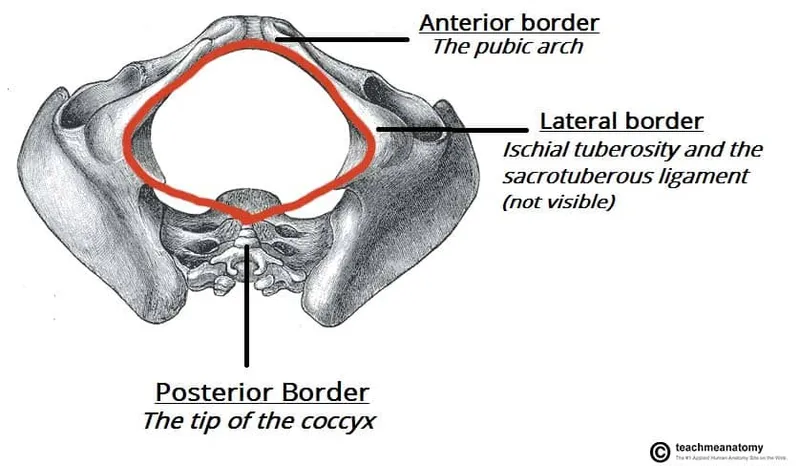
Pelvic cross-sections US Medical PG Question 2: A 36-year-old woman comes to the physician for a 2-month history of urinary incontinence and a vaginal mass. She has a history of five full-term normal vaginal deliveries. She gave birth to a healthy newborn 2-months ago. Since then she has felt a sensation of vaginal fullness and a firm mass in the lower vagina. She has loss of urine when she coughs, sneezes, or exercises. Pelvic examination shows an irreducible pink globular mass protruding out of the vagina. A loss of integrity of which of the following ligaments is most likely involved in this patient's condition?
- A. Infundibulopelvic ligament
- B. Broad ligament of the uterus
- C. Cardinal ligament of the uterus (Correct Answer)
- D. Round ligament of uterus
- E. Uterosacral ligament
Pelvic cross-sections Explanation: ***Cardinal ligament of the uterus***
- The patient's symptoms, including **vaginal mass**, **urinary incontinence** with coughing/sneezing, and history of **multiple vaginal deliveries**, strongly suggest **uterine prolapse**.
- The cardinal ligaments are crucial in providing **lateral cervical support** and are often damaged during childbirth, leading to uterine descent.
*Infundibulopelvic ligament*
- This ligament primarily supports the **ovaries** and contains the **ovarian artery** and vein.
- Damage to this ligament is associated with ovarian prolapse or complications during oophorectomy, not uterine prolapse.
*Broad ligament of the uterus*
- The broad ligament is a **peritoneal fold** that drapes over the uterus, fallopian tubes, and ovaries.
- While it helps to hold these structures in place, its primary role is not in preventing uterine prolapse; it mainly provides a medium for neurovascular structures.
*Round ligament of uterus*
- The round ligament extends from the uterus to the **labia majora** and primarily helps maintain **anteversion** of the uterus.
- It plays a minor role in uterine support and its laxity is not a primary cause of uterine prolapse.
*Uterosacral ligament*
- The uterosacral ligaments provide **posterior support** to the uterus, particularly by anchoring the cervix to the sacrum.
- While damage to these ligaments contributes to **apical prolapse**, the cardinal ligaments are more critical for lateral support and more commonly implicated in overall uterine prolapse following childbirth.
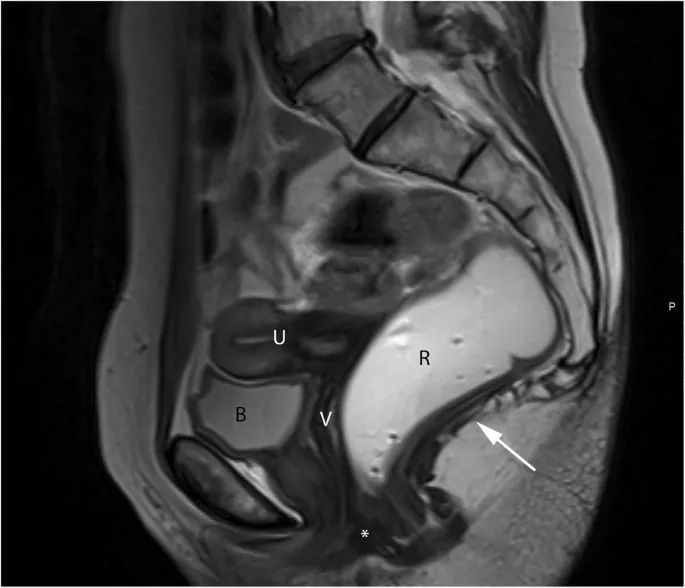
Pelvic cross-sections US Medical PG Question 3: A child is in the nursery one day after birth. A nurse notices a urine-like discharge being expressed through the umbilical stump. What two structures in the embryo are connected by the structure that failed to obliterate during the embryologic development of this child?
- A. Kidney - large bowel
- B. Liver - umbilical vein
- C. Bladder - small bowel
- D. Pulmonary artery - aorta
- E. Bladder - umbilicus (Correct Answer)
Pelvic cross-sections Explanation: ***Bladder - umbilicus***
- A **urine-like discharge** from the umbilical stump indicates a **patent urachus**, which is the embryonic remnant of the allantois.
- The **allantois** (which becomes the urachus) is an embryonic structure that connects the **fetal bladder** to the **umbilicus** during development.
- Normally, the allantois obliterates after birth to form the **median umbilical ligament**, but failure to obliterate results in a patent urachus allowing urine to discharge through the umbilicus.
*Kidney - large bowel*
- These two structures are not directly connected by an obliterating embryonic structure relevant to urine discharge from an umbilical stump.
- The kidneys form urine, and the large bowel is part of the digestive tract, with no direct embryonic communication to the umbilicus for urine expression.
*Liver - umbilical vein*
- The umbilical vein connects the **placenta to the fetal liver** (and ductus venosus) to transport oxygenated blood, not urine.
- Failure of the umbilical vein to obliterate would result in a patent umbilical vein, typically presenting as a vascular anomaly, not urine discharge.
*Pulmonary artery - aorta*
- These structures are connected by the **ductus arteriosus** in fetal circulation, bypassing the pulmonary circulation.
- While important for fetal development, a patent ductus arteriosus (PDA) is a cardiovascular anomaly and would not manifest as urine discharge from the umbilical stump.
*Bladder - small bowel*
- While both structures are involved in waste elimination, there is no normal embryonic structure directly connecting the bladder and small bowel that obliterates to prevent urine discharge from the umbilicus.
- An abnormal connection between the bladder and bowel would typically involve a **fistula** and present with stool in urine or urine in stool, not umbilical discharge.
Pelvic cross-sections US Medical PG Question 4: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Pelvic cross-sections Explanation: ***Bulbous urethra***
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
Pelvic cross-sections US Medical PG Question 5: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Pelvic cross-sections Explanation: ***S3–S4 nerve roots***
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Pelvic cross-sections US Medical PG Question 6: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
Pelvic cross-sections Explanation: ***Cardinal ligament***
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
Pelvic cross-sections US Medical PG Question 7: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Pelvic cross-sections Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Pelvic cross-sections US Medical PG Question 8: A 71-year-old man undergoes CT angiography for suspected mesenteric ischemia. Axial sections at the L1 level show a dissection flap in the superior mesenteric artery with the true lumen severely narrowed. The false lumen extends into a vessel that crosses anterior to the left renal vein. Coronal reconstructions show this vessel arising from the anterolateral aspect of the aorta at L2. The patient has left flank pain and hematuria in addition to abdominal pain. Synthesize the cross-sectional and vascular anatomy to determine the additional vessel involved.
- A. Left gonadal artery arising from the aorta (Correct Answer)
- B. Left middle colic artery from the SMA
- C. Left renal artery from the aorta
- D. Left inferior phrenic artery
- E. Left lumbar artery
Pelvic cross-sections Explanation: ***Left gonadal artery arising from the aorta***
- The **left gonadal artery** originates from the **anterolateral aspect of the aorta** at the **L2 level** and is known to cross **anterior to the left renal vein** as it descends.
- Compromise or dissection involving this artery can cause **flank pain and hematuria** due to its proximity to the ureter and its vascular territory, correlating with the patient's symptoms.
*Left middle colic artery from the SMA*
- The **middle colic artery** arises from the **SMA** at the level of the lower border of the pancreas and supplies the **transverse colon**.
- While it is a branch of the SMA, its course does not classically cross **anterior to the left renal vein**, nor would its involvement typically cause **hematuria**.
*Left renal artery from the aorta*
- The **left renal artery** arises from the aorta at the **L1-L2 level** but typically passes **posterior to the left renal vein**.
- Although renal artery involvement causes hematuria and flank pain, the specific anatomical description of the vessel crossing **anterior to the renal vein** rules it out.
*Left inferior phrenic artery*
- The **inferior phrenic arteries** usually arise from the aorta just above the **celiac trunk** or from the celiac trunk itself at the **T12-L1 level**.
- These vessels supply the **diaphragm and suprarenal glands** and do not descend to cross the **left renal vein at the L2 level**.
*Left lumbar artery*
- **Lumbar arteries** arise from the **posterior aspect** of the abdominal aorta, usually in four pairs corresponding to the L1-L4 vertebrae.
- They travel **posteriorly** to supply the posterior abdominal wall and spinal cord, making the description of an **anterior crossing** of the renal vein anatomically incorrect.
Pelvic cross-sections US Medical PG Question 9: A 29-year-old pregnant woman at 36 weeks gestation presents with severe right upper quadrant pain and elevated liver enzymes. CT (with abdominal shielding) shows a large subcapsular hematoma of the right hepatic lobe. An axial section at the level of T12 shows the hematoma is located between the liver capsule and parenchyma, with the collection tracking along the bare area of the liver. She develops hypotension. Evaluate the anatomical considerations for determining the optimal surgical approach.
- A. Access requires mobilization of the hepatic flexure of the colon first
- B. The hematoma can be accessed extraperitoneally via the bare area without entering the peritoneal cavity (Correct Answer)
- C. Immediate laparotomy through the ligamentum teres is required for vascular control
- D. The falciform ligament must be divided to access the hematoma
- E. Supracolic omental bursa entry provides the safest approach
Pelvic cross-sections Explanation: ***The hematoma can be accessed extraperitoneally via the bare area without entering the peritoneal cavity***
- The **bare area** of the liver is a region on the posterior-superior surface that lacks a **visceral peritoneum** coating, putting it in direct contact with the diaphragm.
- Because this area is continuous with the **retroperitoneal space**, a hematoma localized here can be managed surgically without violating the peritoneal cavity, which may help limit the spread of hemorrhage.
*Access requires mobilization of the hepatic flexure of the colon first*
- Mobilizing the **hepatic flexure** (Cattell-Braasch maneuver) is used to expose the **inframesocolic** space and the second part of the duodenum.
- The bare area is located superiorly and posteriorly on the liver, making colonic mobilization unnecessary and geographically irrelevant for direct access.
*Immediate laparotomy through the ligamentum teres is required for vascular control*
- The **ligamentum teres** is the obliterated umbilical vein located in the free edge of the **falciform ligament**, extending from the umbilicus to the liver notch.
- Opening the ligamentum teres does not provide vascular control of the hepatic parenchyma or the retroperitoneal bare area regions.
*The falciform ligament must be divided to access the hematoma*
- The **falciform ligament** attaches the liver to the anterior abdominal wall and diaphragm, separating the left and right anatomical lobes.
- Dividing it allows for liver mobilization during **intraperitoneal** surgery, but it is not the anatomical gateway to a posterior, extraperitoneal hematoma tracking along the bare area.
*Supracolic omental bursa entry provides the safest approach*
- The **omental bursa** (lesser sac) is located posterior to the stomach and anterior to the pancreas, providing access to the **posterior surface of the stomach**.
- It does not communicate directly with the **bare area** of the liver, which lies between the layers of the **coronary ligament** at the superior/posterior aspect.
Pelvic cross-sections US Medical PG Question 10: A 58-year-old man with esophageal cancer undergoes staging with CT and endoscopic ultrasound. An axial CT at the level of T6 shows the tumor extending from the esophagus into the space between the descending aorta and the left main bronchus. He develops massive hemoptysis during esophagoscopy. The patient is hemodynamically unstable despite resuscitation. Evaluate the anatomical basis for this complication and predict the most likely vessel injured.
- A. Penetration of the left pulmonary artery
- B. Involvement of intercostal arteries
- C. Direct invasion of the descending thoracic aorta
- D. Erosion into the left inferior pulmonary vein
- E. Fistula formation with a bronchial artery (Correct Answer)
Pelvic cross-sections Explanation: ***Fistula formation with a bronchial artery***
- At the level of **T5-T6**, the esophagus is in close proximity to the **bronchial arteries**, which often arise from the descending thoracic aorta and follow the posterior aspect of the bronchi.
- Erosion by an esophageal tumor into high-pressure systemic **bronchial vessels** is a common cause of **massive hemoptysis** and rapid hemodynamic instability in mid-esophageal malignancies.
*Penetration of the left pulmonary artery*
- The **left pulmonary artery** is located more anteriorly and superiorly relative to the esophagus at the level described.
- While it carries a large volume of blood, it is a **low-pressure system** compared to systemic arteries like the bronchial arteries.
*Involvement of intercostal arteries*
- The **posterior intercostal arteries** run in the intercostal spaces along the ribs, further away from the midline esophageal path.
- Injury to these vessels might cause bleeding, but it would not typically manifest as direct **massive hemoptysis** into the airway during esophagoscopy.
*Direct invasion of the descending thoracic aorta*
- While **aortoesophageal fistulas** lead to catastrophic hematemesis, the clinical presentation of massive **hemoptysis** specifically implies an abnormal communication with the **respiratory tract**.
- The tumor's location described between the aorta and the bronchus makes the smaller **bronchial arteries** the more likely intermediary site of erosion leading to airway bleeding.
*Erosion into the left inferior pulmonary vein*
- The **left inferior pulmonary vein** is situated lower in the mediastinum and is more anterior than the esophageal-aortic interface at T6.
- Injury to a pulmonary vein is less likely to produce the rapid, high-pressure **arterial-grade hemorrhage** seen with bronchial or aortic involvement.
More Pelvic cross-sections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.