Upper motor neuron anatomy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper motor neuron anatomy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Upper motor neuron anatomy US Medical PG Question 1: A 75-year-old man is brought to the emergency department by his son. He is suffering from left-sided weakness. The symptoms started 2 hours ago with sudden left-sided weakness. The patient is a known hypertensive, who is inconsistently compliant with his 2 antihypertensive medications and a heavy smoker, with a 40 pack year history. Physical examination shows an elderly male in mild distress. The vital signs include: blood pressure 140/95 mm Hg, pulse 89/min and SpO2 98% on room air. Neurological examination shows left-sided hemiparesis, with no sensory, cognitive, or brain stem abnormalities. A CT scan of the head without IV contrast shows a right-sided ischemic infarct. What other finding is most likely to develop in this patient as his condition progresses?
- A. Loss of deep tendon reflexes
- B. Positive Babinski sign (Correct Answer)
- C. Fasciculations
- D. Flaccid paresis
- E. Muscle atrophy
Upper motor neuron anatomy Explanation: ***Positive Babinski sign***
- The patient has an **acute ischemic stroke** affecting the **right cerebral hemisphere**, leading to left-sided hemiparesis.
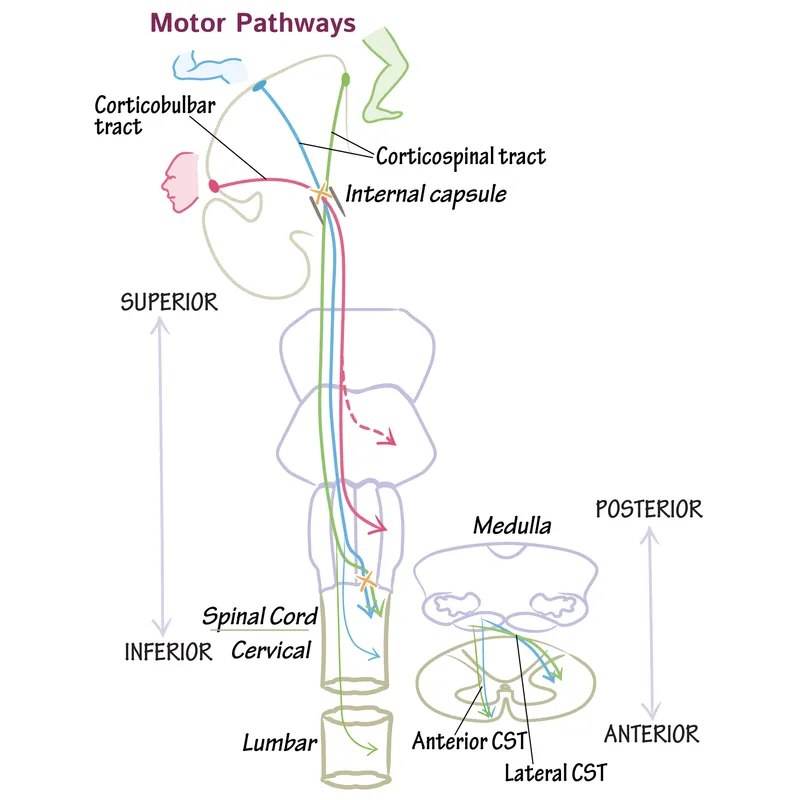
- As the initial **flaccid paralysis** and **spinal shock** phase resolves, **upper motor neuron (UMN) signs** such as spasticity, hyperreflexia, and a positive Babinski sign typically emerge due to damage to the corticospinal tract.
*Loss of deep tendon reflexes*
- This is characteristic of **lower motor neuron (LMN) lesions** or the initial acute phase of an upper motor neuron (UMN) lesion (spinal shock), which is usually transient.
- In a progressive UMN lesion following stroke, **deep tendon reflexes** are expected to become **hyperactive**, not lost.
*Fasciculations*
- **Fasciculations** are spontaneous, visible twitchings of a bundle of muscle fibers and are a hallmark of **lower motor neuron (LMN) pathology**.
- They are not typically seen in **upper motor neuron (UMN) lesions** like an ischemic stroke.
*Flaccid paresis*
- **Flaccid paresis** describes muscle weakness with reduced muscle tone, often seen in the acute phase of a stroke due to **spinal shock**.
- However, as the condition progresses and spinal shock resolves, the **flaccid paresis** will typically evolve into **spastic paresis** due to upper motor neuron damage.
*Muscle atrophy*
- **Muscle atrophy** can occur due to disuse after a stroke, but it is a **late complication** and is not a primary neurological sign that *most likely develops* acutely as the condition progresses.
- Significant **neurogenic atrophy** with severe fasciculations is characteristic of **lower motor neuron lesions**.
Upper motor neuron anatomy US Medical PG Question 2: A 65-year-old male presents to the emergency room complaining of a severe headache. He developed a sudden-onset severe throbbing headache while watching a football game on television. His past medical history is significant for migraines and hypertension; however, he states that this headache is different from his normal migraine headaches. He has a 30 pack-year smoking history. His family history is notable for stroke in his mother and father. His temperature is 98.9°F (37.2°C), blood pressure is 150/90 mmHg, pulse is 100/min, and respirations are 14/min. On examination, he is oriented to person, place, and time. Neck motion is limited due to pain. Strength is 5/5 bilaterally in both the upper and the lower extremities and sensation is grossly intact across all the dermatomal distributions. Patellar, brachioradialis, and Achilles reflexes are 2+ bilaterally. The vessel that is most commonly involved in this patient's likely condition directly branches off which of the following vessels?
- A. Middle cerebral artery
- B. Maxillary artery
- C. Anterior cerebral artery
- D. Posterior cerebral artery
- E. Internal carotid artery (Correct Answer)
Upper motor neuron anatomy Explanation: ***Internal carotid artery***
- The patient's presentation with a **sudden-onset, severe "thunderclap" headache**, cervical pain, and normal neurologic examination, particularly in the context of **hypertension and smoking history**, is highly suggestive of a **subarachnoid hemorrhage (SAH)**. SAH is most commonly caused by rupture of a **saccular (berry) aneurysm**.
- Approximately 85% of SAHs result from the rupture of an aneurysm in the **anterior circulation**. The most common site for these aneurysms is the **anterior communicating artery**, which directly branches off the **anterior cerebral artery**. However, the **anterior cerebral artery (ACA)**, the **middle cerebral artery (MCA)**, and the **posterior communicating artery (PCoA)** (which is commonly involved in berry aneurysms) all originate directly or indirectly, through the ACA, from the **internal carotid artery (ICA)**. Therefore, the ICA is the most encompassing and correct option from which the most common aneurysm sites ultimately branch.
*Middle cerebral artery*
- While the **middle cerebral artery (MCA)** is a common location for aneurysms, particularly at its bifurcation, it is generally less common than the anterior communicating artery or the posterior communicating artery.
- Aneurysms of the MCA are also branches of the internal carotid artery.
*Maxillary artery*
- The **maxillary artery** is primarily involved in supplying blood to structures in the deep face, maxilla, and mandible.
- It is not a significant location for intracranial berry aneurysms that lead to subarachnoid hemorrhage.
*Anterior cerebral artery*
- While the **anterior cerebral artery (ACA)** itself can be a site for aneurysms, particularly the **anterior communicating artery** (AComA) which connects the two ACAs, it is a branch off the internal carotid artery.
- The AComA is the single most common site for berry aneurysms; however, the question asks for the vessel from which the commonly involved vessel *directly branches off*. The ACA itself directly branches off the ICA.
*Posterior cerebral artery*
- The **posterior cerebral artery (PCA)** is part of the posterior circulation, originating from the basilar artery.
- Aneurysms in the posterior circulation (vertebrobasilar system) are less common causes of SAH than those in the anterior circulation.
Upper motor neuron anatomy US Medical PG Question 3: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Upper motor neuron anatomy Explanation: ***Left anterior cerebral artery***
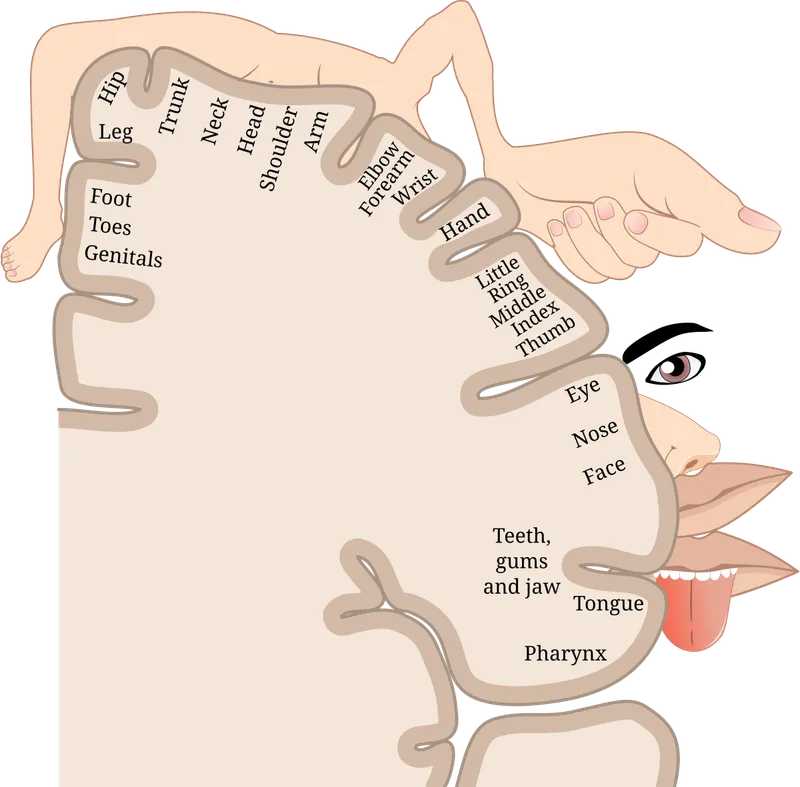
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Upper motor neuron anatomy US Medical PG Question 4: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
Upper motor neuron anatomy Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Upper motor neuron anatomy US Medical PG Question 5: A 80-year-old man is brought to the emergency department with complaints that he "can't control his left leg". His symptoms started a few hours ago. He was outside taking a walk with his wife when suddenly his leg shot out and kicked her. His past medical history is notable for diabetes, hypertension, and a myocardial infarction 5 years ago. He smokes 1-2 cigarettes/day. He does not use alcohol or illicit drugs. On exam, the patient has intermittent wide, flinging movements that affect his proximal left arm and left leg. Which of the following parts of his brain is most likely damaged?
- A. Ventral posterior thalamic nucleus
- B. Left internal capsule
- C. Right subthalamic nucleus (Correct Answer)
- D. Left subthalamic nucleus
- E. Right internal capsule
Upper motor neuron anatomy Explanation: ***Right subthalamic nucleus***
- The patient's symptoms of sudden, uncontrolled, wide-flinging movements, affecting the contralateral (left) side of the body, are characteristic of **hemiballism**.
- **Hemiballism** is almost exclusively caused by a lesion in the **contralateral subthalamic nucleus (STN)**, or its afferent/efferent connections, most commonly due to a **lacunar infarct**.
*Ventral posterior thalamic nucleus*
- Damage to the **ventral posterior thalamic nucleus** primarily causes **sensory deficits**, such as loss of touch, pain, and temperature sensation, on the contralateral side of the body.
- While it can be involved in motor control, it does not typically cause the characteristic flinging movements seen in hemiballism.
*Left internal capsule*
- A lesion in the **left internal capsule** would result in contralateral (right-sided) motor and sensory deficits, including **hemiparesis** or **hemiplegia**, but not the ballistic, uncontrollable movements described.
- The internal capsule carries major motor and sensory pathways to and from the cerebral cortex.
*Left subthalamic nucleus*
- Damage to the **left subthalamic nucleus** would cause hemiballism on the **contralateral (right) side** of the body.
- The patient's symptoms are on the left side, indicating a lesion in the right subthalamic nucleus.
*Right internal capsule*
- A lesion in the **right internal capsule** would primarily cause contralateral (left-sided) motor and sensory deficits, such as **hemiparesis** or **hemiplegia**.
- While it affects the contralateral side as described in the patient, it would typically present as weakness rather than uncontrolled flinging movements.
Upper motor neuron anatomy US Medical PG Question 6: A 5-year-old boy who recently emigrated from Nigeria is brought to the emergency department because of a 2-day history of lower leg weakness, swallowing difficulty, and drooling of saliva. He has not yet received any childhood vaccinations. Two days after admission, the patient develops shortness of breath. Pulse oximetry shows an oxygen saturation of 64%. Despite resuscitative efforts, the patient dies of respiratory failure. At autopsy, examination of the spinal cord shows destruction of the anterior horn cells. Neurological examination of this patient would have most likely shown which of the following findings?
- A. Sensory loss
- B. Positive Babinski sign
- C. Hyporeflexia (Correct Answer)
- D. Myoclonus
- E. Pronator drift
Upper motor neuron anatomy Explanation: ***Hyporeflexia***
- The destruction of **anterior horn cells** in the spinal cord is characteristic of **poliomyelitis**, a disease that primarily affects **lower motor neurons**.
- Lower motor neuron lesions lead to symptoms like **flaccid paralysis**, **weakness**, and **hyporeflexia** (diminished or absent reflexes).
*Sensory loss*
- Poliomyelitis specifically targets **motor neurons** and typically spares **sensory pathways**, meaning sensory function remains intact.
- Therefore, **sensory loss** is not a characteristic finding in poliomyelitis.
*Positive Babinski sign*
- A positive Babinski sign (**upgoing plantar reflex**) is indicative of an **upper motor neuron lesion** affecting the **corticospinal tract**.
- Since poliomyelitis involves lower motor neurons, a positive Babinski sign would not be expected.
*Myoclonus*
- **Myoclonus** refers to brief, involuntary twitching of a muscle or a group of muscles, often associated with disorders affecting the **cerebellum**, **brainstem**, or **cortex**.
- It is not a typical neurological finding in **poliomyelitis**, which primarily causes muscle weakness and paralysis.
*Pronator drift*
- **Pronator drift** is a sign of **upper motor neuron weakness** affecting the **contralateral corticospinal tract**, particularly in the arm.
- As **poliomyelitis** is a **lower motor neuron disease**, pronator drift would not be expected as a primary finding.
Upper motor neuron anatomy US Medical PG Question 7: A 27-year-old man is brought to the emergency department because of a knife wound to his back. His pulse is 110/min, respirations are 14/min, and blood pressure is 125/78 mm Hg. Examination shows a 5-cm deep stab wound at the level of T9. He withdraws the right foot to pain but is unable to sense vibration or whether his right toe is flexed or extended. Sensation in the left leg is normal. Motor strength is 5/5 in all extremities. Rectal tone is normal. Which of the following spinal column structures was most likely affected?
- A. Central spinal cord grey matter
- B. Lateral corticospinal tract
- C. Dorsal root (Correct Answer)
- D. Artery of Adamkiewicz
- E. Posterior spinal artery
Upper motor neuron anatomy Explanation: ***Dorsal root***
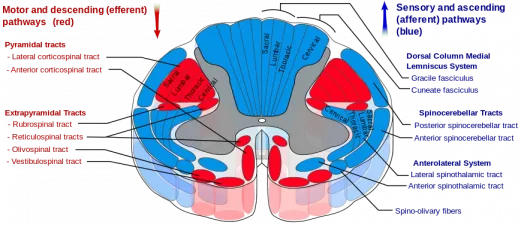
- The patient's inability to sense **vibration** or **proprioception** (flexed/extended toe) on the right side, with intact motor strength, strongly implicates damage to the **dorsal columns** or the **dorsal root** carrying these afferent fibers.
- The dorsal root transmits **sensory** (afferent) information from the periphery to the spinal cord, and injury would selectively impair these specific sensory modalities without affecting motor function.
*Central spinal cord grey matter*
- Damage to the central gray matter, as seen in conditions like **syringomyelia**, typically affects the **spinothalamic tracts** first, leading to a "cape-like" distribution of bilateral loss of **pain** and **temperature sensation**.
- It would not primarily cause isolated **proprioceptive** or **vibration** loss with preserved motor function.
*Lateral corticospinal tract*
- Injury to the **lateral corticospinal tract** results in **motor deficits**, specifically **weakness** or paralysis, usually on the same side or contralateral depending on the location of the lesion (above or below decussation).
- The patient exhibits normal motor strength (5/5), indicating this tract is likely intact.
*Artery of Adamkiewicz*
- Occlusion or injury to the **Artery of Adamkiewicz** typically causes **anterior spinal artery syndrome**, affecting the **anterior two-thirds of the spinal cord**.
- This leads to bilateral loss of **motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts), with preservation of dorsal column functions (vibration, proprioception).
*Posterior spinal artery*
- The **posterior spinal arteries** supply the **dorsal columns**, and their occlusion would lead to bilateral loss of **vibration** and **proprioception**.
- However, the patient's symptoms are **unilateral** on the right side, suggesting a more localized injury to the dorsal root or dorsal column on that side rather than a bilateral vascular event.
Upper motor neuron anatomy US Medical PG Question 8: A 22-year-old man is brought to the emergency department after he was impaled by a metal rod during a work accident. The rod went into his back around the level of T9 but was removed before arrival. He has no past medical history and does not take any medications. On physical examination, he has significant muscle weakness in his entire left lower body. He also exhibits impaired vibration and proprioception in his left leg as well as loss of pain and temperature sensation in his right leg. Which of the following sections of the spinal cord was most likely damaged in this patient?
- A. Posterior cord
- B. Anterior cord
- C. Left hemicord (Correct Answer)
- D. Central cord
- E. Right hemicord
Upper motor neuron anatomy Explanation: ***Left hemicord***
- The combination of **ipsilateral motor weakness** and **loss of vibration/proprioception** (damage to the **corticospinal tract** and **dorsal column**) along with **contralateral loss of pain/temperature** (damage to the **spinothalamic tract**) is the classic presentation of **Brown-Séquard syndrome**, which results from a lesion affecting one side (hemicord) of the spinal cord.
- The injury at **T9** is consistent with lower body symptoms, as tracts for the legs would be affected at this level.
*Posterior cord*
- Damage to the **posterior cord** primarily affects the **dorsal columns**, leading to **ipsilateral loss of vibration and proprioception**.
- It would not explain the **ipsilateral motor weakness** or the **contralateral loss of pain and temperature sensation**.
*Anterior cord*
- **Anterior cord syndrome** typically presents with **bilateral loss of motor function** (due to damage to the corticospinal tracts) and **bilateral loss of pain and temperature sensation** (due to damage to the spinothalamic tracts).
- **Vibration and proprioception** are usually preserved because the dorsal columns are spared.
*Central cord*
- **Central cord syndrome** most commonly results from hyperextension injuries, particularly in the cervical spine, affecting the central gray matter.
- It typically causes greater **weakness in the upper extremities** than the lower extremities and a variable sensory loss, often in a **"cape-like" distribution**.
*Right hemicord*
- A **right hemicord** lesion would cause **right-sided motor weakness** and **loss of vibration/proprioception**, along with **left-sided loss of pain/temperature sensation**.
- The patient's symptoms are on the **left side for motor/proprioception** and the **right side for pain/temperature**, indicating a left hemicord lesion.
Upper motor neuron anatomy US Medical PG Question 9: A 61-year-old man is brought to the emergency department because of increasing weakness of his right arm and leg that began when he woke up that morning. He did not notice any weakness when he went to bed the night before. He has hypertension and hypercholesterolemia. Current medications include hydrochlorothiazide and atorvastatin. He is alert and oriented to person, time, place. His temperature is 36.7°C (98°F), pulse is 91/min, and blood pressure is 132/84 mm Hg. Examination shows drooping of the right side of the face. Muscle strength is decreased in the right upper and lower extremities. Deep tendon reflexes are 4+ on the right side. Sensation is intact. His speech is normal in rate and rhythm. The remainder of the examination shows no abnormalities. An infarction of which of the following sites is the most likely cause of this patient's symptoms?
- A. Base of the left pons
- B. Left cerebellar vermis
- C. Left posterolateral thalamus
- D. Posterior limb of the left internal capsule (Correct Answer)
- E. Left lateral medulla
Upper motor neuron anatomy Explanation: ***Posterior limb of the left internal capsule***
- The patient presents with sudden onset of **right-sided weakness**, including the face, arm, and leg (hemiparesis), consistent with a **pure motor stroke**.
- The **posterior limb of the internal capsule** contains UMN fibers of the **corticospinal and corticobulbar tracts**, which project to the contralateral side of the body, thus lesions here cause contralateral pure motor deficits.
*Base of the left pons*
- A lesion here would typically cause **contralateral hemiparesis or hemiplegia** (right side in this case).
- However, pontine lesions also often include **cranial nerve palsies** (e.g., abducens or facial nerve) or **ataxia**, which are not described.
*Left cerebellar vermis*
- Damage to the cerebellar vermis primarily results in **truncal ataxia** and disorders of gait and balance.
- It would not cause contralateral hemiparesis or facial droop, as seen in this patient.
*Left posterolateral thalamus*
- An infarct in this area would primarily cause **contralateral sensory deficits**, such as hemianesthesia or dysesthesia.
- While motor deficits can occur, they are typically less prominent than sensory issues and would not be the isolated pure motor syndrome described.
*Left lateral medulla*
- A lesion in the lateral medulla (e.g., Wallenberg syndrome) typically presents with **contralateral pain and temperature loss**, ipsilateral Horner's syndrome, ataxia, and dysphagia.
- It would not manifest as an isolated pure motor hemiparesis.
Upper motor neuron anatomy US Medical PG Question 10: A 46-year-old man comes to the physician because of a 2-month history of hoarseness and drooling. Initially, he had difficulty swallowing solid food, but now he has difficulty swallowing foods like oatmeal as well. During this period, he also developed weakness in both arms and has had an 8.2 kg (18 lb) weight loss. He appears ill. His vital signs are within normal limits. Examination shows tongue atrophy and pooled oral secretions. There is diffuse muscle atrophy in all extremities. Deep tendon reflexes are 3+ in all extremities. Sensation to pinprick, light touch, and vibration is intact. An esophagogastroduodenoscopy shows no abnormalities. Which of the following is the most likely cause of this patient's symptoms?
- A. Destruction of upper and lower motor neurons (Correct Answer)
- B. Autoimmune destruction of acetylcholine receptors
- C. Multiple cerebral infarctions
- D. Dilation of the central spinal canal
- E. Demyelination of peripheral nerves
Upper motor neuron anatomy Explanation: ***Destruction of upper and lower motor neurons***
- This patient's presentation with **hoarseness, drooling, dysphagia, diffuse muscle atrophy**, and **hyperreflexia (3+ deep tendon reflexes)** points to both **upper motor neuron (UMN)** and **lower motor neuron (LMN)** signs.
- The combination of UMN and LMN involvement, particularly bulbar symptoms (hoarseness, drooling, dysphagia), diffuse muscle atrophy, and progressive weakness, is highly characteristic of **amyotrophic lateral sclerosis (ALS)**, which involves the progressive destruction of UMNs and LMNs.
*Autoimmune destruction of acetylcholine receptors*
- This describes **myasthenia gravis**, which typically presents with **fluctuating muscle weakness** that worsens with activity and improves with rest.
- While it can cause dysphagia and hoarseness, it usually spares deep tendon reflexes, and diffuse muscle atrophy is not a primary feature, nor are UMN signs like hyperreflexia.
*Multiple cerebral infarctions*
- Multiple cerebral infarctions, or **multi-infarct dementia**, can cause various neurological deficits depending on their location, but they rarely present with a diffuse, progressive picture of both UMN and LMN signs.
- The patient's symptoms are more consistent with a **neurodegenerative disease** rather than acute or subacute vascular events affecting widespread motor pathways in this specific, combined fashion.
*Dilation of the central spinal canal*
- This refers to **syringomyelia**, which typically causes **cape-like sensory loss** (loss of pain and temperature sensation across the shoulders and arms) due to damage to the spinothalamic tracts, often with **LMN weakness** in the upper extremities.
- It would not explain the prominent UMN signs (hyperreflexia), diffuse muscle atrophy in all extremities, or bulbar symptoms like hoarseness and drooling.
*Demyelination of peripheral nerves*
- This is characteristic of **peripheral neuropathies** such as **Guillain-Barré syndrome** or chronic inflammatory demyelinating polyneuropathy (CIDP).
- These conditions primarily cause **LMN signs** like **flaccid paralysis**, **hyporeflexia or areflexia**, and sensory loss, which is inconsistent with the prominent hyperreflexia seen in this patient.
More Upper motor neuron anatomy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.