UMN vs LMN lesions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for UMN vs LMN lesions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
UMN vs LMN lesions US Medical PG Question 1: A 57-year-old man presents to his primary care physician with a 2-month history of right upper and lower extremity weakness. He noticed the weakness when he started falling far more frequently while running errands. Since then, he has had increasing difficulty with walking and lifting objects. His past medical history is significant only for well-controlled hypertension, but he says that some members of his family have had musculoskeletal problems. His right upper extremity shows forearm atrophy and depressed reflexes while his right lower extremity is hypertonic with a positive Babinski sign. Which of the following is most likely associated with the cause of this patient's symptoms?
- A. HLA-DR2 haplotype
- B. Mutation in SOD1 (Correct Answer)
- C. Viral infection
- D. HLA-B8 haplotype
- E. Mutation in SMN1
UMN vs LMN lesions Explanation: ***Mutation in SOD1***
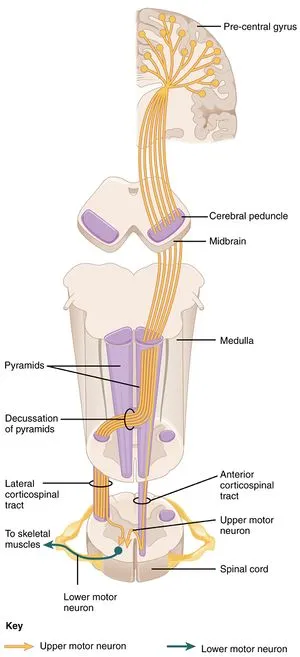
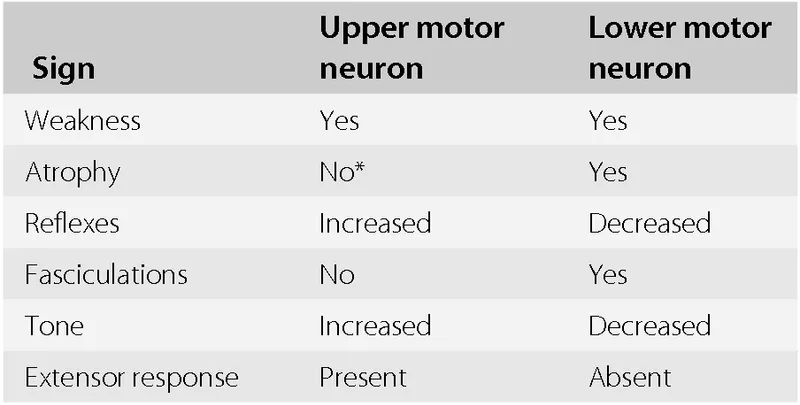
- The patient exhibits features of both **upper motor neuron (UMN)** and **lower motor neuron (LMN)** lesions, specifically **forearm atrophy** and depressed reflexes (LMN) alongside **hypertonicity** and a **positive Babinski sign** (UMN). This combination is characteristic of **amyotrophic lateral sclerosis (ALS)**.
- Mutations in the **superoxide dismutase 1 (SOD1)** gene are responsible for approximately 20% of familial ALS cases, aligning with the patient's report of "some members of his family have had musculoskeletal problems."
*HLA-DR2 haplotype*
- The **HLA-DR2 haplotype** is strongly associated with **multiple sclerosis (MS)**, an autoimmune demyelinating disease.
- While MS can cause UMN symptoms, it typically does not present with the pronounced LMN signs like **atrophy** and **depressed reflexes** seen in this patient.
*Viral infection*
- **Viral infections** can trigger various neurological conditions, such as **Guillain-Barré syndrome** (GBS) which causes demyelination of peripheral nerves.
- GBS primarily results in **ascending motor weakness** and **areflexia** (LMN signs), but it does not cause UMN signs like hypertonicity or a positive Babinski sign.
*HLA-B8 haplotype*
- The **HLA-B8 haplotype** is associated with several autoimmune diseases, including **myasthenia gravis** and **celiac disease**.
- While myasthenia gravis causes **muscle weakness**, it is characterized by **fluctuating weakness** that worsens with activity and improves with rest, affecting specific muscle groups, unlike the progressive UMN and LMN involvement seen here.
*Mutation in SMN1*
- A **mutation in the SMN1 gene** is the primary cause of **spinal muscular atrophy (SMA)**, a genetic disorder.
- SMA specifically leads to the death of **lower motor neurons** in the spinal cord, resulting in exclusively LMN signs such as **muscle weakness** and **atrophy**, without any UMN involvement (e.g., hypertonicity or Babinski sign).
UMN vs LMN lesions US Medical PG Question 2: A 54-year-old man comes to the physician for the evaluation of difficulty swallowing of both solids and liquids for 1 month. During the past 5 months, he has also had increased weakness of his hands and legs. He sails regularly and is unable to hold the ropes as tightly as before. Ten years ago, he was involved in a motor vehicle collision. Examination shows atrophy of the tongue. Muscle strength is decreased in the right upper and lower extremities. There is muscle stiffness in the left lower extremity. Deep tendon reflexes are 1+ in the right upper and lower extremities, 3+ in the left upper extremity, and 4+ in the left lower extremity. Plantar reflex shows an extensor response on the left foot. Sensation to light touch, pinprick, and vibration is intact. Which of the following is the most likely diagnosis?
- A. Amyotrophic lateral sclerosis (Correct Answer)
- B. Inclusion-body myositis
- C. Subacute combined degeneration of spinal cord
- D. Syringomyelia
- E. Cervical spondylosis with myelopathy
UMN vs LMN lesions Explanation: ***Amyotrophic lateral sclerosis***
- This diagnosis accounts for the combination of **upper motor neuron** (spasticity, hyperreflexia, extensor plantar response) and **lower motor neuron** (weakness, atrophy, dysphagia, tongue atrophy) signs and symptoms.
- The progressive weakness in both hands and legs, alongside **dysphagia** (difficulty swallowing) and **dysarthria** (implied by tongue atrophy), is highly characteristic of ALS, a neurodegenerative disorder affecting motor neurons.
*Cervical spondylosis with myelopathy*
- While it can cause some **upper motor neuron signs** (spasticity, hyperreflexia), it does not typically present with prominent **lower motor neuron signs** like widespread muscle atrophy or tongue atrophy.
- Sensation is usually impaired below the level of compression, but in this patient, sensation is **intact**, making cervical myelopathy less likely.
*Inclusion-body myositis*
- This is a **muscle disease** causing progressive weakness and atrophy, particularly in the quadriceps and forearm flexors, often with **dysphagia**.
- However, it is primarily a **myopathy** and does not cause **upper motor neuron signs** such as spasticity, hyperreflexia, or an extensor plantar response.
*Subacute combined degeneration of spinal cord*
- This condition is caused by **vitamin B12 deficiency** and typically presents with a combination of **sensory ataxia**, weakness, and **paresthesias**, affecting the dorsal and lateral columns.
- It usually presents with **paresthesias** and **sensory deficits** (especially vibratory sense and proprioception), which are specifically noted as intact in this patient.
*Syringomyelia*
- This involves a **fluid-filled cyst (syrinx)** within the spinal cord, leading to a classic "cape-like" distribution of **loss of pain and temperature sensation** in the upper extremities due to damage to the spinothalamic tracts.
- While it can cause weakness and atrophy, it characteristically spares light touch, vibration, and position sense but involves **dissociated sensory loss**, which is not seen in this patient.
UMN vs LMN lesions US Medical PG Question 3: A 75-year-old man is brought to the emergency department by his son. He is suffering from left-sided weakness. The symptoms started 2 hours ago with sudden left-sided weakness. The patient is a known hypertensive, who is inconsistently compliant with his 2 antihypertensive medications and a heavy smoker, with a 40 pack year history. Physical examination shows an elderly male in mild distress. The vital signs include: blood pressure 140/95 mm Hg, pulse 89/min and SpO2 98% on room air. Neurological examination shows left-sided hemiparesis, with no sensory, cognitive, or brain stem abnormalities. A CT scan of the head without IV contrast shows a right-sided ischemic infarct. What other finding is most likely to develop in this patient as his condition progresses?
- A. Loss of deep tendon reflexes
- B. Positive Babinski sign (Correct Answer)
- C. Fasciculations
- D. Flaccid paresis
- E. Muscle atrophy
UMN vs LMN lesions Explanation: ***Positive Babinski sign***
- The patient has an **acute ischemic stroke** affecting the **right cerebral hemisphere**, leading to left-sided hemiparesis.
- As the initial **flaccid paralysis** and **spinal shock** phase resolves, **upper motor neuron (UMN) signs** such as spasticity, hyperreflexia, and a positive Babinski sign typically emerge due to damage to the corticospinal tract.
*Loss of deep tendon reflexes*
- This is characteristic of **lower motor neuron (LMN) lesions** or the initial acute phase of an upper motor neuron (UMN) lesion (spinal shock), which is usually transient.
- In a progressive UMN lesion following stroke, **deep tendon reflexes** are expected to become **hyperactive**, not lost.
*Fasciculations*
- **Fasciculations** are spontaneous, visible twitchings of a bundle of muscle fibers and are a hallmark of **lower motor neuron (LMN) pathology**.
- They are not typically seen in **upper motor neuron (UMN) lesions** like an ischemic stroke.
*Flaccid paresis*
- **Flaccid paresis** describes muscle weakness with reduced muscle tone, often seen in the acute phase of a stroke due to **spinal shock**.
- However, as the condition progresses and spinal shock resolves, the **flaccid paresis** will typically evolve into **spastic paresis** due to upper motor neuron damage.
*Muscle atrophy*
- **Muscle atrophy** can occur due to disuse after a stroke, but it is a **late complication** and is not a primary neurological sign that *most likely develops* acutely as the condition progresses.
- Significant **neurogenic atrophy** with severe fasciculations is characteristic of **lower motor neuron lesions**.
UMN vs LMN lesions US Medical PG Question 4: A 76-year-old woman with hypertension and coronary artery disease is brought to the emergency department after the sudden onset of right-sided weakness. Her pulse is 83/min and blood pressure is 156/90 mm Hg. Neurological examination shows right-sided facial drooping and complete paralysis of the right upper and lower extremities. Tongue position is normal and she is able to swallow liquids without difficulty. Knee and ankle deep tendon reflexes are exaggerated on the right. Sensation to vibration, position, and light touch is normal bilaterally. She is oriented to person, place, and time, and is able to speak normally. Occlusion of which of the following vessels is the most likely cause of this patient's current symptoms?
- A. Ipsilateral anterior cerebral artery
- B. Contralateral middle cerebral artery
- C. Anterior spinal artery
- D. Contralateral lenticulostriate artery (Correct Answer)
- E. Ipsilateral posterior inferior cerebellar artery
UMN vs LMN lesions Explanation: ***Contralateral lenticulostriate artery***
- The patient presents with **pure motor hemiparesis** affecting the face, arm, and leg equally on the right side, with **no sensory deficits, aphasia, or cognitive impairment**.
- This clinical pattern is classic for a **lacunar stroke** affecting the **internal capsule**, which is supplied by the **lenticulostriate arteries** (branches of the middle cerebral artery).
- The internal capsule contains tightly packed corticospinal and corticobulbar fibers; a small infarct here causes complete contralateral motor deficits without cortical signs.
- The **absence of cortical findings** (normal speech, cognition, and sensation) distinguishes this from cortical MCA stroke.
*Contralateral middle cerebral artery*
- A **cortical MCA stroke** would typically present with **cortical signs** such as aphasia (if left hemisphere), neglect (if right hemisphere), sensory loss, and visual field defects.
- MCA strokes usually show **arm and face > leg** weakness (the leg area is supplied by ACA).
- This patient's **pure motor syndrome** without cortical signs points to a subcortical lesion, not cortical MCA occlusion.
*Ipsilateral anterior cerebral artery*
- First, the lateralization is incorrect - symptoms are right-sided, indicating left hemisphere pathology, so it would be **contralateral** ACA.
- ACA occlusion causes weakness predominantly in the **contralateral leg > arm**, with relative sparing of the face.
- This patient has equal involvement of face, arm, and leg, which is inconsistent with ACA territory.
*Anterior spinal artery*
- The **anterior spinal artery** supplies the anterior two-thirds of the spinal cord, including the corticospinal tracts and anterior horn cells.
- Occlusion causes **bilateral** motor weakness below the lesion level and bilateral loss of pain/temperature sensation.
- It does not cause **unilateral facial weakness** or the distribution of deficits seen in this patient.
*Ipsilateral posterior inferior cerebellar artery*
- Again, lateralization is incorrect - symptoms would be from **contralateral** PICA for motor findings, but PICA supplies the lateral medulla and inferior cerebellum.
- PICA occlusion causes **lateral medullary syndrome (Wallenberg syndrome)**: ataxia, vertigo, dysphagia, dysarthria, Horner syndrome, and contralateral pain/temperature loss.
- The patient's **pure motor hemiparesis** without cerebellar or brainstem signs is incompatible with PICA occlusion.
UMN vs LMN lesions US Medical PG Question 5: A 17-year-old boy is brought to the emergency department after being stabbed with a knife during an altercation. Physical examination shows a 4-cm stab wound on the right lateral border of the T1 spinous process. An MRI of the spinal cord shows damage to the area of the right lateral corticospinal tract at the level of T1. Further evaluation will most likely show which of the following findings?
- A. Absence of right-sided motor function below T1 (Correct Answer)
- B. Absence of left-sided proprioception below T1
- C. Presence of left-sided Babinski sign
- D. Absence of left-sided fine touch sensation below T1
- E. Absence of right-sided temperature sensation below T1
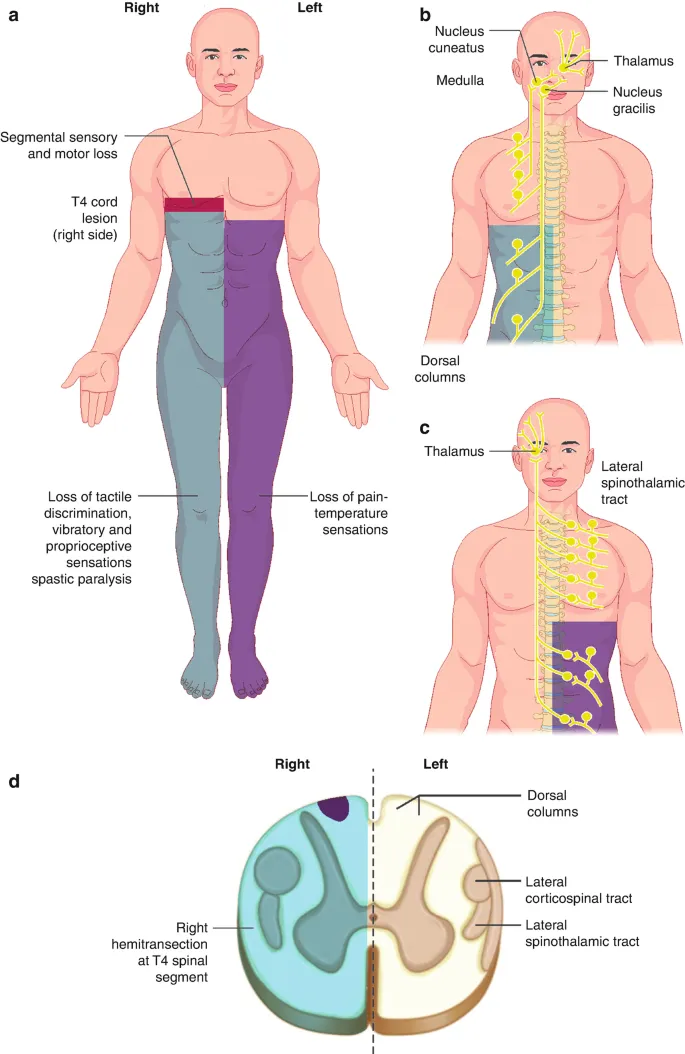
UMN vs LMN lesions Explanation: ***Absence of right-sided motor function below T1***
- The **right lateral corticospinal tract** controls **voluntary motor function** on the **ipsilateral side** of the body.
- Damage to this tract at T1 would therefore lead to a loss of motor function on the right side below the level of the injury.
*Absence of left-sided proprioception below T1*
- **Proprioception** is carried by the **dorsal columns**, which ascend **ipsilaterally** before decussating in the brainstem.
- Damage to the right lateral corticospinal tract would not affect left-sided proprioception.
*Presence of left-sided Babinski sign*
- A **Babinski sign** (upgoing plantar reflex) indicates an **upper motor neuron lesion**.
- Since the corticospinal tract decussates in the **medulla** (before reaching the spinal cord), a lesion in the **right lateral corticospinal tract at T1** affects motor function on the **right side** of the body.
- Therefore, if a Babinski sign were present, it would be on the **right side**, not the left.
*Absence of left-sided fine touch sensation below T1*
- **Fine touch** sensation is transmitted by the **dorsal columns**, which ascend **ipsilaterally** and decussate in the brainstem.
- Damage to the right lateral corticospinal tract would not affect fine touch sensation on the left side.
*Absence of right-sided temperature sensation below T1*
- **Temperature sensation** is carried by the **spinothalamic tracts**, which decussate at the level of entry into the spinal cord.
- Therefore, a lesion of the right lateral corticospinal tract would not affect temperature sensation on the right side; ipsilateral temperature loss would be due to damage to the right spinothalamic tract, which is located more anterolaterally in the spinal cord.
UMN vs LMN lesions US Medical PG Question 6: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
UMN vs LMN lesions Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
UMN vs LMN lesions US Medical PG Question 7: A 54-year-old man is referred to a tertiary care hospital with a history of 5 months of progressive difficulty in walking and left leg numbness. He first noticed mild gait unsteadiness and later developed gradual right leg weakness. His left leg developed progressive numbness and tingling. His blood pressure is 138/88 mm Hg, the heart rate is 72/min, and the temperature is 36.7°C (98.2°F). On physical examination, he is alert and oriented to person, place, and time. Cranial nerves are intact. Muscle strength is 5/5 in both upper extremities and left lower extremity, but 3/5 in the right leg with increased tone. The plantar reflex is extensor on the right. Pinprick sensation is decreased on the left side below the umbilicus. Vibration and joint position senses are decreased in the right foot and leg. All sensations are normal in the upper extremities. Finger-to-nose and heel-to-shin testing are normal. This patient’s lesion is most likely located in which of the following parts of the nervous system?
- A. Right hemi-spinal cord (Correct Answer)
- B. Right frontal lobe
- C. Left frontal lobe
- D. Left hemi-spinal cord
- E. Right pons
UMN vs LMN lesions Explanation: ***Right hemi-spinal cord***
- The patient presents with **ipsilateral motor weakness** (right leg 3/5 with increased tone and extensor plantar reflex) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the right foot and leg) along with **contralateral spinothalamic loss** (decreased pinprick sensation on the left side below the umbilicus). This classic combination of symptoms is known as **Brown-Séquard syndrome**, which results from a lesion affecting one half of the spinal cord.
- The specific pattern of deficits—motor and proprioceptive loss on the same side as the lesion, and pain/temperature loss on the opposite side—localizes the lesion to the **right half of the spinal cord**.
*Right frontal lobe*
- A lesion in the right frontal lobe would typically cause **contralateral motor weakness** (left-sided) and potentially cognitive or behavioral changes, without the specific sensory dissociation seen in this patient.
- It would not explain the **ipsilateral proprioceptive loss** or the **contralateral pain/temperature loss** at different levels as observed in this case.
*Left frontal lobe*
- A lesion in the left frontal lobe would primarily result in **contralateral motor weakness** (right-sided), similar to the right leg weakness observed, but it would not explain the other sensory deficits, particularly the **contralateral pain/temperature loss** (right-sided in this scenario) and the **ipsilateral proprioceptive loss**.
- **Speech disturbances** (aphasia) are also common with left frontal lobe lesions, depending on the exact location, which are not mentioned here.
*Left hemi-spinal cord*
- A lesion in the left hemi-spinal cord would cause **ipsilateral motor weakness** (left leg weakness) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the left foot and leg), along with **contralateral spinothalamic loss** (decreased pinprick sensation on the right side).
- This pattern is the opposite of the patient's symptoms, which show right-sided weakness and proprioceptive loss, and left-sided pain/temperature loss.
*Right pons*
- A lesion in the pons would typically present with a **combination of cranial nerve deficits** (e.g., facial sensory or motor abnormalities, gaze palsies) **and long tract signs**, often affecting both sides of the body due to the compact nature of the brainstem.
- While it could cause long tract signs, the specific pattern of **dissociated ipsilateral and contralateral sensory/motor deficits** observed below the umbilical level is highly characteristic of a spinal cord lesion and less so of a pontine lesion.
UMN vs LMN lesions US Medical PG Question 8: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
UMN vs LMN lesions Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
UMN vs LMN lesions US Medical PG Question 9: A 39-year-old woman is brought to the emergency department following a stab wound to the neck. Per the patient, she was walking her dog when she got robbed and was subsequently stabbed with a knife. Vitals are stable. Strength examination reveals 2/5 right-sided elbow flexion and extension, wrist extension, and finger motions. Babinski sign is upward-going on the right. There is decreased sensation to light touch and vibration on the patient's right side up to her shoulder. She also reports decreased sensation to pinprick and temperature on her left side, including her lower extremities, posterior forearm, and middle finger. The patient's right pupil is 2 mm smaller than the left with drooping of the right upper eyelid. Which of the following is the most likely cause of the patient’s presentation?
- A. Hemisection injury (Correct Answer)
- B. Syringomyelia
- C. Anterior cord syndrome
- D. Posterior cord syndrome
- E. Central cord syndrome
UMN vs LMN lesions Explanation: ***Hemisection injury***
- The combination of **ipsilateral motor weakness** and **dorsal column deficits** (vibration, light touch) along with **contralateral loss of pain and temperature sensation** (spinothalamic tract) is the hallmark of a Brown-Séquard syndrome, which results from a hemisection injury to the spinal cord.
- The presence of **ipsilateral Horner's syndrome** (miosis and ptosis) indicates sympathetic nerve damage, further localizing the injury to the cervical spinal cord and supporting a hemisection.
*Syringomyelia*
- This condition is characterized by a **cavity (syrinx)** within the spinal cord, typically leading to a **cape-like distribution of pain and temperature loss** due to damage to the decussating spinothalamic fibers.
- It usually spares the dorsal columns and motor tracts in early stages, which contradicts the described ipsilateral motor and dorsal column deficits.
*Anterior cord syndrome*
- Results from damage to the **anterior spinal artery**, leading to **bilateral loss of motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts) below the level of injury.
- **Proprioception and vibration sensation** (dorsal columns) are typically preserved in this syndrome, which is inconsistent with the patient's presentation.
*Posterior cord syndrome*
- Involves damage primarily to the **dorsal columns**, resulting in **loss of proprioception, vibration, and light touch** below the level of injury.
- **Motor function, pain, and temperature sensation** are generally preserved, which is not consistent with the motor deficits and contralateral pain/temperature loss described.
*Central cord syndrome*
- Most commonly seen after **hyperextension injuries**, leading to greater **motor weakness in the upper extremities** than the lower extremities.
- It typically causes varying degrees of **sensory loss** and can preserve sacral sensation, but the specific pattern of ipsilateral motor/dorsal column deficits and contralateral spinothalamic loss is not characteristic of central cord syndrome.
UMN vs LMN lesions US Medical PG Question 10: A 12-year-old boy is brought to his orthopedic surgeon for evaluation of leg pain and positioning. Specifically, over the past several months he has been complaining of thigh pain and has more difficulty sitting in his wheelchair. His medical history is significant for spastic quadriplegic cerebral palsy since birth and has undergone a number of surgeries for contractures in his extremities. At this visit his legs are found to be scissored such that they cross each other at the knees and are difficult to separate. Surgery is performed and the boy is placed into a cast that keeps his legs abducted to prevent scissoring. Overactivity of the muscles innervated by which of the following nerves is most consistent with this patient's deformity?
- A. Nerve to the iliopsoas
- B. Sciatic nerve
- C. Femoral nerve
- D. Superior gluteal nerve
- E. Obturator nerve (Correct Answer)
UMN vs LMN lesions Explanation: ***Obturator***
- The **obturator nerve** innervates the **adductor muscles** of the thigh (adductor longus, brevis, magnus, gracilis, and obturator externus).
- **Overactivity** of these muscles leads to thigh adduction, causing the characteristic **"scissoring" gait** seen in some patients with cerebral palsy.
*Nerve to the iliopsoas*
- The **iliopsoas muscle** is a primary **hip flexor**, important for activities like sitting and standing.
- While involvement of hip flexors can cause contractures, it would manifest as difficulty extending the hip, not a scissoring deformity.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and most muscles of the leg and foot.
- Its overactivity or spasticity would primarily affect knee flexion and foot movements, not hip adduction or scissoring.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, medialis, intermedius) and the sartorius.
- Overactivity would lead to strong knee extension and hip flexion, not the adducted and scissored leg position described.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles, which are primarily hip abductors and internal rotators.
- Overactivity of these muscles would cause hip abduction, which is the opposite of the scissoring deformity.
More UMN vs LMN lesions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.