Spinal cord injury levels and their effects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spinal cord injury levels and their effects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spinal cord injury levels and their effects US Medical PG Question 1: A 35-year-old man who suffered a motor vehicle accident 3 months ago presents to the office for a neurological evaluation. He has no significant past medical history and takes no current medications. He has a family history of coronary artery disease in his father and Alzheimer’s disease in his mother. On physical examination, his blood pressure is 110/60 mm Hg, the pulse is 85/min, the temperature is 37.0°C (98.6°F), and the respiratory rate is 20/min. Neurological examination is suggestive of a lesion in the anterior spinal artery that affects the anterior two-thirds of the spinal cord, which is later confirmed with angiography. Which of the following exam findings would have suggested this diagnosis?
- A. Loss of vibratory sense below the level of the lesion
- B. Loss of pain and temperature sensation above the level of the lesion
- C. Negative plantar extensor response in his lower limbs
- D. Flaccid paralysis on the right side
- E. Preserved pressure sensation (Correct Answer)
Spinal cord injury levels and their effects Explanation: ***Preserved pressure sensation***
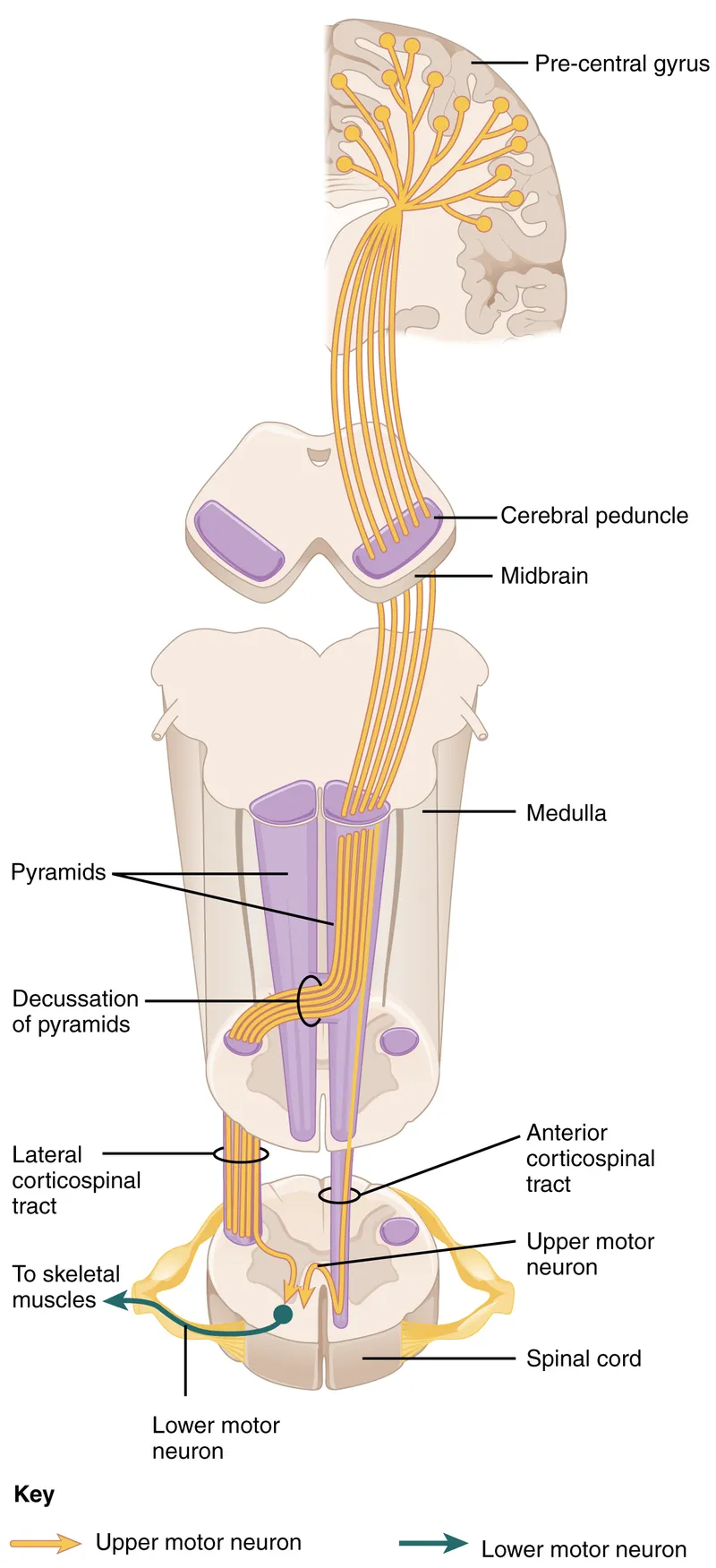
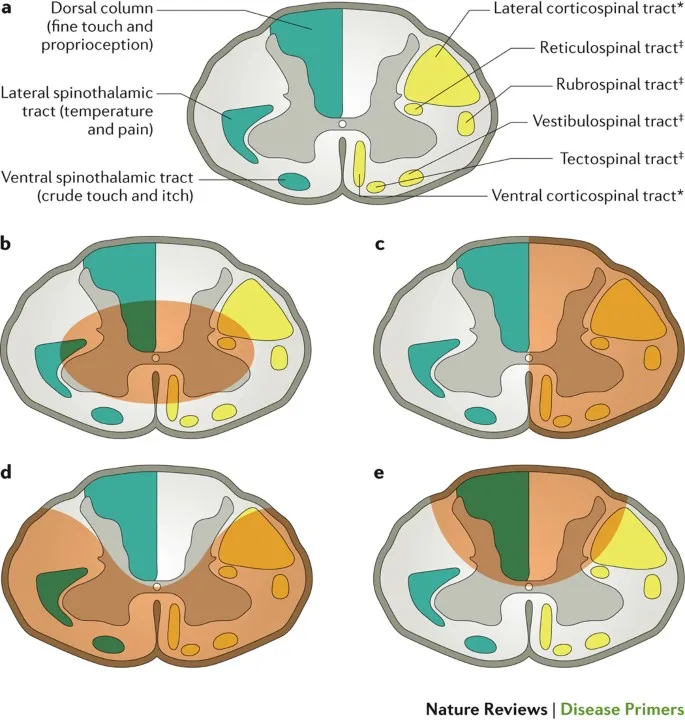
- **Anterior spinal artery** occlusion affects the **spinothalamic tracts** (pain and temperature) and **corticospinal tracts** (motor function), but spares the **dorsal columns**.
- The **dorsal columns** carry **vibration, proprioception, and discriminative (fine) touch and pressure sensation**, which would therefore be preserved.
- While crude touch/pressure via the anterior spinothalamic tract may be impaired, the preservation of dorsal column function allows for intact discriminative pressure sensation, distinguishing this from other cord syndromes.
*Loss of vibratory sense below the level of the lesion*
- **Vibratory sense** is carried by the **dorsal columns**, which are typically spared in **anterior spinal artery syndromes** as they are supplied by the posterior spinal arteries.
- Loss of vibratory sense would suggest involvement of the posterior part of the spinal cord, inconsistent with an anterior spinal artery lesion.
*Loss of pain and temperature sensation above the level of the lesion*
- **Anterior spinal artery syndrome** causes loss of **pain and temperature sensation** *below* the level of the lesion, as the spinothalamic tracts are affected in the anterior cord.
- Sensation *above* the lesion level should be intact, as those pathways have already ascended past the lesion.
*Negative plantar extensor response in his lower limbs*
- A **negative plantar extensor response** (normal plantar reflex) indicates the toes curl downwards, which is the normal response.
- Lesions of the **corticospinal tract**, such as in anterior spinal artery syndrome, typically cause a **positive Babinski sign** (extensor plantar response), where the big toe extends upwards, indicating upper motor neuron damage.
*Flaccid paralysis on the right side*
- **Anterior spinal artery syndrome** causes **bilateral motor deficits** due to involvement of both **corticospinal tracts** in the anterior cord.
- While initial presentation can be **flaccid paralysis** due to spinal shock below the level of the lesion, it is typically **bilateral**, not unilateral, and evolves to **spastic paralysis** over time.
Spinal cord injury levels and their effects US Medical PG Question 2: A 38-year-old man comes to the physician for a follow-up examination. He has quadriparesis as a result of a burst fracture of the cervical spine that occurred after a fall from his roof 1 month ago. He has urinary and bowel incontinence. He appears malnourished. His temperature is 37.1°C (98.8°F), pulse is 88/min, and blood pressure is 104/60 mm Hg. Examination shows spasticity in all extremities. Muscle strength is decreased in proximal and distal muscle groups bilaterally. Deep tendon reflexes are 4+ bilaterally. Plantar reflex shows extensor response bilaterally. Sensation to pinprick and temperature is absent below the neck. Sensation to vibration, position, and light touch is normal bilaterally. Rectal tone is decreased. There is a 1-cm area of erythema over the sacrum. Which of the following is the most likely cause of this patient's symptoms?
- A. Hemi-transection of the spinal cord
- B. Cavitation within the spinal cord
- C. Injury to gray matter of the spinal cord
- D. Occlusion of the posterior spinal artery
- E. Damage to the anterior spinal artery (Correct Answer)
Spinal cord injury levels and their effects Explanation: ***Damage to the anterior spinal artery***
- This typically results in **anterior cord syndrome**, characterized by bilateral loss of pain and temperature sensation, motor function (quadriparesis), and autonomic dysfunction (bowel/bladder incontinence below the level of injury).
- The **preservation of posterior column functions** (vibration, proprioception, light touch) is a hallmark of anterior spinal artery ischemia, as the posterior columns are supplied by the posterior spinal arteries.
*Hemi-transection of the spinal cord*
- This describes **Brown-Séquard syndrome**, which involves ipsilateral loss of motor function, vibration, and proprioception, and contralateral loss of pain and temperature sensation.
- The patient's symptoms are inconsistent with Brown-Séquard syndrome due to the **bilateral presentation of motor and sensory deficits**.
*Cavitation within the spinal cord*
- This condition, known as **syringomyelia**, typically presents with a **cape-like distribution of pain and temperature loss** (due to central cord involvement affecting the decussating spinothalamic fibers).
- It would usually spare motor function initially and would not explain the sudden, severe quadriparesis and complete sensory loss described.
*Injury to gray matter of the spinal cord*
- Isolated gray matter injury, often seen in conditions like **central cord syndrome**, primarily affects the pain and temperature pathways and may cause upper extremity weakness.
- It would not explain the **complete loss of motor function and pain/temperature sensation below the neck** while preserving posterior column function.
*Occlusion of the posterior spinal artery*
- Occlusion of the posterior spinal artery would primarily affect the **dorsal columns**, leading to loss of vibration, proprioception, and light touch.
- This patient, however, has **preserved sensation to vibration, position, and light touch**, making posterior spinal artery occlusion unlikely.
Spinal cord injury levels and their effects US Medical PG Question 3: A 22-year-old man is rushed to the emergency department after a motor vehicle accident. The patient states that he feels weakness and numbness in both of his legs. He also reports pain in his lower back. His airway, breathing, and circulation is intact, and he is conversational. Neurologic exam is significant for bilateral lower extremity flaccid paralysis and impaired pain and temperature sensation up to T10-T11 with normal vibration sense. A computerized tomography scan of the spine is performed which shows a vertebral burst fracture of the vertebral body at the level of T11. Which of the following findings is most likely present in this patient?
- A. Intact vibration sense
- B. Bowel incontinence (Correct Answer)
- C. Flaccid paralysis at the level of the lesion
- D. Spasticity below the lesion
- E. Impaired proprioception sense
Spinal cord injury levels and their effects Explanation: ***Bowel incontinence***
- The presented symptoms of acute **bilateral lower extremity flaccid paralysis**, **impaired pain and temperature sensation**, and a T11 **vertebral burst fracture** are highly indicative of **anterior cord syndrome**.
- **Anterior cord syndrome** characteristically involves damage to the **anterior two-thirds of the spinal cord**, affecting the **corticospinal tracts** (motor control), **spinothalamic tracts** (pain and temperature sensation), and the **autonomic fibers** that control bladder and bowel function, leading to **bowel and bladder dysfunction**.
*Intact vibration sense*
- The sensation of **vibration** and **proprioception** is carried by the **dorsal columns** (posterior part of the spinal cord), which are typically **spared** in **anterior cord syndrome**.
- Therefore, **intact vibration sense** is an expected finding, but the question asks for the **most likely finding** that represents a significant complication of the syndrome.
*Flaccid paralysis at the level of the lesion*
- While **flaccid paralysis** is present in the lower extremities, it occurs **below the level of the lesion** due to damage to the descending motor tracts (corticospinal tracts).
- Flaccid paralysis *at* the level of the lesion would typically involve damage to the **lower motor neurons** at that specific segment, which is not the primary feature described for a burst fracture causing **anterior cord syndrome**.
*Spasticity below the lesion*
- **Spasticity** typically develops much **later** in spinal cord injuries, after the initial phase of **spinal shock** resolves (usually weeks to months).
- In the acute phase following a significant spinal cord injury, **flaccid paralysis** is the more common finding below the lesion, reflecting spinal shock.
*Impaired proprioception sense*
- Similar to vibration sense, **proprioception** is primarily mediated by the **dorsal columns**, which are generally **spared** in **anterior cord syndrome**.
- Therefore, **proprioception** would likely be **intact**, not impaired, in this specific type of spinal cord injury.
Spinal cord injury levels and their effects US Medical PG Question 4: A 80-year-old man is brought to the emergency department with complaints that he "can't control his left leg". His symptoms started a few hours ago. He was outside taking a walk with his wife when suddenly his leg shot out and kicked her. His past medical history is notable for diabetes, hypertension, and a myocardial infarction 5 years ago. He smokes 1-2 cigarettes/day. He does not use alcohol or illicit drugs. On exam, the patient has intermittent wide, flinging movements that affect his proximal left arm and left leg. Which of the following parts of his brain is most likely damaged?
- A. Ventral posterior thalamic nucleus
- B. Left internal capsule
- C. Right subthalamic nucleus (Correct Answer)
- D. Left subthalamic nucleus
- E. Right internal capsule
Spinal cord injury levels and their effects Explanation: ***Right subthalamic nucleus***
- The patient's symptoms of sudden, uncontrolled, wide-flinging movements, affecting the contralateral (left) side of the body, are characteristic of **hemiballism**.
- **Hemiballism** is almost exclusively caused by a lesion in the **contralateral subthalamic nucleus (STN)**, or its afferent/efferent connections, most commonly due to a **lacunar infarct**.
*Ventral posterior thalamic nucleus*
- Damage to the **ventral posterior thalamic nucleus** primarily causes **sensory deficits**, such as loss of touch, pain, and temperature sensation, on the contralateral side of the body.
- While it can be involved in motor control, it does not typically cause the characteristic flinging movements seen in hemiballism.
*Left internal capsule*
- A lesion in the **left internal capsule** would result in contralateral (right-sided) motor and sensory deficits, including **hemiparesis** or **hemiplegia**, but not the ballistic, uncontrollable movements described.
- The internal capsule carries major motor and sensory pathways to and from the cerebral cortex.
*Left subthalamic nucleus*
- Damage to the **left subthalamic nucleus** would cause hemiballism on the **contralateral (right) side** of the body.
- The patient's symptoms are on the left side, indicating a lesion in the right subthalamic nucleus.
*Right internal capsule*
- A lesion in the **right internal capsule** would primarily cause contralateral (left-sided) motor and sensory deficits, such as **hemiparesis** or **hemiplegia**.
- While it affects the contralateral side as described in the patient, it would typically present as weakness rather than uncontrolled flinging movements.
Spinal cord injury levels and their effects US Medical PG Question 5: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Spinal cord injury levels and their effects Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
Spinal cord injury levels and their effects US Medical PG Question 6: A 74-year-old male is brought to the emergency department 1 hour after he fell from the top of the staircase at home. He reports pain in his neck as well as weakness of his upper extremities. He is alert and immobilized in a cervical collar. He has hypertension treated with hydrochlorothiazide. His pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/70 mmHg. Examination shows bruising and midline cervical tenderness. Neurologic examination shows diminished strength and sensation to pain and temperature in the upper extremities, particularly in the hands. Upper extremity deep tendon reflexes are absent. Strength, sensation, and reflexes in the lower extremities are intact. Anal sensation and tone are present. Babinski's sign is absent bilaterally. Which of the following is most likely to confirm the cause of this patient's neurologic examination findings?
- A. CT angiography of the neck
- B. MRI of the cervical spine without contrast (Correct Answer)
- C. X-ray of the cervical spine
- D. CT of the cervical spine with contrast
- E. Cervical myelography
Spinal cord injury levels and their effects Explanation: ***MRI of the cervical spine without contrast***
- This patient presents with symptoms consistent with **central cord syndrome**, characterized by greater weakness in the upper extremities than the lower extremities, often following a hyperextension injury in older adults with pre-existing cervical spondylosis. **MRI is the gold standard for visualizing soft tissue injuries**, including spinal cord compression, edema, or hemorrhage, which are typical causes of central cord syndrome.
- Given the primary concern for spinal cord injury and the detailed neurological deficits indicating specific cord involvement, **MRI** offers the best resolution for evaluating the extent of cord damage, disc herniation, ligamentous injury, and pre-existing degenerative changes.
*CT angiography of the neck*
- **CT angiography** primarily evaluates the **vascular structures** of the neck (e.g., carotid and vertebral arteries) for dissection, stenosis, or occlusion.
- While vascular injury could occur in trauma, the patient's neurological findings (disproportionate upper extremity weakness, pain and temperature sensation loss) point more directly to **spinal cord pathology** rather than isolated vascular compromise as the primary cause.
*X-ray of the cervical spine*
- **X-rays** are useful for initial screening of **bony fractures** and significant dislocations but offer limited information about soft tissues, such as the spinal cord, ligaments, or intervertebral discs.
- They cannot adequately visualize the spinal cord damage responsible for the patient's specific neurological deficits, making it insufficient for confirming the cause of central cord syndrome.
*CT of the cervical spine with contrast*
- **CT scans** excel at visualizing **bony structures** and acute fractures, but even with contrast, they provide less detail of the **spinal cord parenchyma** and soft tissue ligaments compared to MRI.
- **Contrast** is typically used to highlight vascular structures, inflammatory processes, or tumors, which are not the primary diagnostic concerns suggested by this patient's acute post-traumatic presentation of central cord syndrome.
*Cervical myelography*
- **Myelography** involves injecting contrast into the subarachnoid space, followed by X-ray or CT imaging, to outline the spinal cord and nerve roots.
- While it can identify **spinal cord compression**, it is an **invasive procedure** with risks (e.g., headache, seizures) and has largely been replaced by the non-invasive and superior soft tissue imaging capabilities of MRI, especially in acute trauma.
Spinal cord injury levels and their effects US Medical PG Question 7: A 58-year-old man comes to the physician because of burning pain in his neck and arms for a year. He has also had paresthesias in his hands during this period. He has had increasing weakness in both hands during the past 3 months. He has type 2 diabetes mellitus, hypercholesterolemia, and hypertension. He was involved in a motor vehicle collision 3 years ago. Current medications include metformin, sitagliptin, enalapril, atorvastatin, and aspirin. He has had 7 sexual partners in his lifetime; he uses condoms inconsistently. He is oriented to time, place, and person. Vital signs are within normal limits. The pupils are equal and reactive to light. Examination of the upper extremities shows decreased muscle strength, absent reflexes, and decreased hand grip with fasciculations bilaterally. Sensation to temperature and pain is absent over the chest and bilateral upper arms. Vibration and joint position sensations are present in the upper limbs. Cranial nerve examination shows no focal findings. Examination of the lower extremities show no abnormalities. Which of the following is the most likely diagnosis?
- A. Brown-Séquard syndrome
- B. Tabes dorsalis
- C. Multiple sclerosis
- D. Syringomyelia (Correct Answer)
- E. Cervical disk prolapse
Spinal cord injury levels and their effects Explanation: ***Syringomyelia***
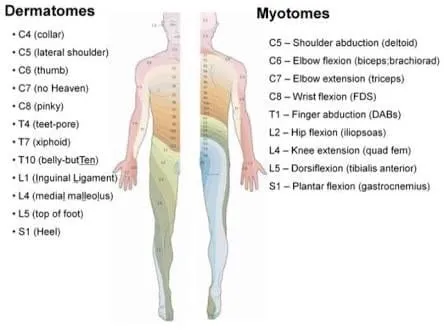
- This condition is characterized by a central canal cavitation (syrinx) in the spinal cord, leading to damage to the **spinothalamic tracts** (loss of pain and temperature sensation) and anterior horn cells (weakness, fasciculations, absent reflexes). The **'cape-like' distribution** of sensory loss over the chest and arms, along with hand weakness, is classic.
- The sensation loss to temperature and pain over the chest and bilateral upper arms with preserved vibration and joint position sensation in upper limbs is a **dissociated sensory loss**, a hallmark of syringomyelia, as the dorsal columns (responsible for vibration and proprioception) are typically spared.
*Brown-Séquard syndrome*
- This syndrome results from **hemitransaction of the spinal cord**, causing ipsilateral loss of motor function and proprioception/vibration sensation, and contralateral loss of pain and temperature sensation below the lesion.
- The patient's symptoms of **bilateral sensory loss** and **bilateral weakness** do not fit this unilateral lesion pattern.
*Tabes dorsalis*
- This is a late manifestation of **syphilis**, primarily affecting the posterior columns of the spinal cord (dorsal columns), leading to loss of **proprioception and vibration sensation**, along with ataxia and shooting pains.
- The patient presents with loss of pain and temperature sensation, not primarily proprioception and vibration, and has **motor weakness with fasciculations**, which are not typical for tabes dorsalis.
*Multiple sclerosis*
- MS is characterized by **demyelination in the central nervous system**, presenting with diverse neurological symptoms that often wax and wane, affecting multiple areas of the brain and spinal cord.
- While it can cause sensory and motor deficits, the **dissociated sensory loss** (pain/temperature vs. vibration/proprioception) in a "cape-like" distribution with prominent fasciculations points away from MS.
*Cervical disk prolapse*
- A cervical disk prolapse typically causes **radicular pain and neurological deficits** (motor weakness, sensory loss, reflex changes) in a dermatomal or myotomal distribution corresponding to the compressed nerve root.
- While it can cause arm pain and weakness, the **bilateral, "cape-like" dissociated sensory loss** over the chest and arms is not characteristic of a single or multiple cervical nerve root compressions.
Spinal cord injury levels and their effects US Medical PG Question 8: A 39-year-old woman is brought to the emergency department following a stab wound to the neck. Per the patient, she was walking her dog when she got robbed and was subsequently stabbed with a knife. Vitals are stable. Strength examination reveals 2/5 right-sided elbow flexion and extension, wrist extension, and finger motions. Babinski sign is upward-going on the right. There is decreased sensation to light touch and vibration on the patient's right side up to her shoulder. She also reports decreased sensation to pinprick and temperature on her left side, including her lower extremities, posterior forearm, and middle finger. The patient's right pupil is 2 mm smaller than the left with drooping of the right upper eyelid. Which of the following is the most likely cause of the patient’s presentation?
- A. Hemisection injury (Correct Answer)
- B. Syringomyelia
- C. Anterior cord syndrome
- D. Posterior cord syndrome
- E. Central cord syndrome
Spinal cord injury levels and their effects Explanation: ***Hemisection injury***
- The combination of **ipsilateral motor weakness** and **dorsal column deficits** (vibration, light touch) along with **contralateral loss of pain and temperature sensation** (spinothalamic tract) is the hallmark of a Brown-Séquard syndrome, which results from a hemisection injury to the spinal cord.
- The presence of **ipsilateral Horner's syndrome** (miosis and ptosis) indicates sympathetic nerve damage, further localizing the injury to the cervical spinal cord and supporting a hemisection.
*Syringomyelia*
- This condition is characterized by a **cavity (syrinx)** within the spinal cord, typically leading to a **cape-like distribution of pain and temperature loss** due to damage to the decussating spinothalamic fibers.
- It usually spares the dorsal columns and motor tracts in early stages, which contradicts the described ipsilateral motor and dorsal column deficits.
*Anterior cord syndrome*
- Results from damage to the **anterior spinal artery**, leading to **bilateral loss of motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts) below the level of injury.
- **Proprioception and vibration sensation** (dorsal columns) are typically preserved in this syndrome, which is inconsistent with the patient's presentation.
*Posterior cord syndrome*
- Involves damage primarily to the **dorsal columns**, resulting in **loss of proprioception, vibration, and light touch** below the level of injury.
- **Motor function, pain, and temperature sensation** are generally preserved, which is not consistent with the motor deficits and contralateral pain/temperature loss described.
*Central cord syndrome*
- Most commonly seen after **hyperextension injuries**, leading to greater **motor weakness in the upper extremities** than the lower extremities.
- It typically causes varying degrees of **sensory loss** and can preserve sacral sensation, but the specific pattern of ipsilateral motor/dorsal column deficits and contralateral spinothalamic loss is not characteristic of central cord syndrome.
Spinal cord injury levels and their effects US Medical PG Question 9: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Spinal cord injury levels and their effects Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
Spinal cord injury levels and their effects US Medical PG Question 10: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Spinal cord injury levels and their effects Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
More Spinal cord injury levels and their effects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.