Somatotopic organization US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Somatotopic organization. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Somatotopic organization US Medical PG Question 1: A neurology resident sees a stroke patient on the wards. This 57-year-old man presented to the emergency department after sudden paralysis of his right side. He was started on tissue plasminogen activator within 4 hours, as his wife noticed the symptoms and immediately called 911. When the resident asks the patient how he is doing, he replies by saying that his apartment is on Main St. He does not seem to appropriately answer the questions being asked, but rather speaks off topic. He is able to repeat the word "fan." His consciousness is intact, and his muscle tone and reflexes are normal. Upon striking the lateral part of his sole, his big toe extends upward and the other toes fan out. Which of the following is the area most likely affected in his condition?
- A. Caudate nucleus
- B. Broca’s area
- C. Arcuate fasciculus
- D. Temporal lobe (Correct Answer)
- E. Cuneus gyrus
Somatotopic organization Explanation: ***Temporal lobe***
- The patient exhibits features of **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** ("apartment is on Main St." when asked how he is), poor comprehension, and the ability to repeat words. **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus**.
- **Sudden paralysis of the right side** indicates involvement of the left cerebral hemisphere (**contralateral motor cortex** lesion), while speech disturbances point to the dominant hemisphere, which is typically the **left temporal lobe**.
*Caudate nucleus*
- Lesions of the **caudate nucleus** are primarily associated with **movement disorders** (e.g., chorea) and **behavioral changes**, not typically with fluent aphasia as described.
- While it plays a role in cognitive functions, its direct involvement in the specific language deficits presented is less likely.
*Broca’s area*
- Damage to **Broca's area**, located in the **frontal lobe**, causes **Broca's aphasia**, characterized by **non-fluent, halting speech** with good comprehension and poor repetition.
- The patient's speech is **fluent**, though off-topic, which contrasts with the typical presentation of Broca's aphasia.
*Arcuate fasciculus*
- The **arcuate fasciculus** connects Broca's and Wernicke's areas, and damage to it typically causes **conduction aphasia**, characterized by **impaired repetition** despite fluent speech and good comprehension.
- While the patient has impaired comprehension, his ability to repeat "fan" makes conduction aphasia less likely than Wernicke's aphasia, where repetition can vary but comprehension is profoundly affected.
*Cuneus gyrus*
- The **cuneus gyrus** is located in the **occipital lobe** and is primarily involved in **visual processing**.
- Damage to this area would lead to **visual field deficits** (e.g., hemianopia) rather than the language and comprehension problems described.
Somatotopic organization US Medical PG Question 2: A 72-year-old man with longstanding history of diabetes mellitus and hypertension presents to the emergency department with sudden-onset numbness. On your neurological exam, you note that he has loss of sensation on the left side of his face, arm, and leg. His motor strength exam is normal, as are his cranial nerves. Which of the following is the most likely explanation for his presentation?
- A. Middle cerebral artery stroke
- B. Thalamic stroke (Correct Answer)
- C. Conversion disorder
- D. Anterior cerebral artery stroke
- E. Basilar artery stroke
Somatotopic organization Explanation: ***Thalamic stroke***
- A **thalamic stroke** classically presents with pure sensory deficits, often affecting the **contralateral** side of the body without significant motor weakness or cranial nerve involvement.
- The patient's history of **diabetes mellitus** and **hypertension** are significant risk factors for this type of **lacunar stroke**.
*Middle cerebral artery stroke*
- An **MCA stroke** typically causes **contralateral hemiparesis/hemiplegia** (motor weakness), sensory loss, and possibly **aphasia** (if dominant hemisphere) or **hemineglect** (if non-dominant hemisphere).
- The patient's preserved motor strength and normal cranial nerves make a pure MCA stroke unlikely.
*Conversion disorder*
- **Conversion disorder** involves neurological symptoms that are inconsistent with known neurological conditions, often linked to psychological stress.
- While it can manifest as numbness, the specific pattern of **pure sensory loss** and the patient's strong vascular risk factors suggest a physiological rather than psychological cause.
*Anterior cerebral artery stroke*
- An **ACA stroke** primarily affects the **contralateral leg** more than the arm, often with **urinary incontinence** and **abulia** (lack of initiative).
- The patient's involvement of the face, arm, and leg equally, without leg predominance or behavioral changes, is atypical for an ACA stroke.
*Basilar artery stroke*
- A **basilar artery stroke** typically manifests with a wide range of severe neurological deficits, including **ataxia**, **dysarthria**, **diplopia**, **vertigo**, and often with **quadriparesis** or **locked-in syndrome**.
- The patient's isolated sensory loss without other brainstem signs makes a basilar artery stroke highly improbable.
Somatotopic organization US Medical PG Question 3: A 35-year-old man who suffered a motor vehicle accident 3 months ago presents to the office for a neurological evaluation. He has no significant past medical history and takes no current medications. He has a family history of coronary artery disease in his father and Alzheimer’s disease in his mother. On physical examination, his blood pressure is 110/60 mm Hg, the pulse is 85/min, the temperature is 37.0°C (98.6°F), and the respiratory rate is 20/min. Neurological examination is suggestive of a lesion in the anterior spinal artery that affects the anterior two-thirds of the spinal cord, which is later confirmed with angiography. Which of the following exam findings would have suggested this diagnosis?
- A. Loss of vibratory sense below the level of the lesion
- B. Loss of pain and temperature sensation above the level of the lesion
- C. Negative plantar extensor response in his lower limbs
- D. Flaccid paralysis on the right side
- E. Preserved pressure sensation (Correct Answer)
Somatotopic organization Explanation: ***Preserved pressure sensation***
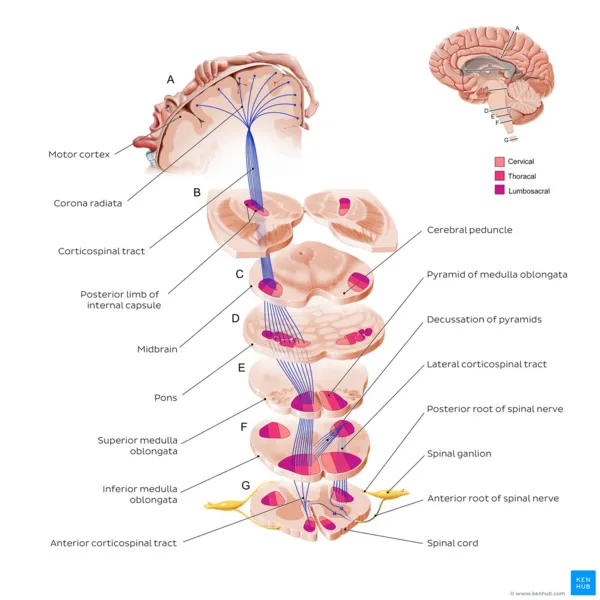
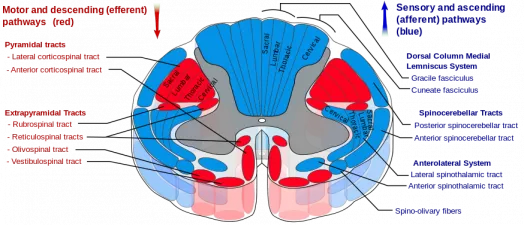
- **Anterior spinal artery** occlusion affects the **spinothalamic tracts** (pain and temperature) and **corticospinal tracts** (motor function), but spares the **dorsal columns**.
- The **dorsal columns** carry **vibration, proprioception, and discriminative (fine) touch and pressure sensation**, which would therefore be preserved.
- While crude touch/pressure via the anterior spinothalamic tract may be impaired, the preservation of dorsal column function allows for intact discriminative pressure sensation, distinguishing this from other cord syndromes.
*Loss of vibratory sense below the level of the lesion*
- **Vibratory sense** is carried by the **dorsal columns**, which are typically spared in **anterior spinal artery syndromes** as they are supplied by the posterior spinal arteries.
- Loss of vibratory sense would suggest involvement of the posterior part of the spinal cord, inconsistent with an anterior spinal artery lesion.
*Loss of pain and temperature sensation above the level of the lesion*
- **Anterior spinal artery syndrome** causes loss of **pain and temperature sensation** *below* the level of the lesion, as the spinothalamic tracts are affected in the anterior cord.
- Sensation *above* the lesion level should be intact, as those pathways have already ascended past the lesion.
*Negative plantar extensor response in his lower limbs*
- A **negative plantar extensor response** (normal plantar reflex) indicates the toes curl downwards, which is the normal response.
- Lesions of the **corticospinal tract**, such as in anterior spinal artery syndrome, typically cause a **positive Babinski sign** (extensor plantar response), where the big toe extends upwards, indicating upper motor neuron damage.
*Flaccid paralysis on the right side*
- **Anterior spinal artery syndrome** causes **bilateral motor deficits** due to involvement of both **corticospinal tracts** in the anterior cord.
- While initial presentation can be **flaccid paralysis** due to spinal shock below the level of the lesion, it is typically **bilateral**, not unilateral, and evolves to **spastic paralysis** over time.
Somatotopic organization US Medical PG Question 4: A 17-year-old boy is brought to the emergency department after being stabbed with a knife during an altercation. Physical examination shows a 4-cm stab wound on the right lateral border of the T1 spinous process. An MRI of the spinal cord shows damage to the area of the right lateral corticospinal tract at the level of T1. Further evaluation will most likely show which of the following findings?
- A. Absence of right-sided motor function below T1 (Correct Answer)
- B. Absence of left-sided proprioception below T1
- C. Presence of left-sided Babinski sign
- D. Absence of left-sided fine touch sensation below T1
- E. Absence of right-sided temperature sensation below T1
Somatotopic organization Explanation: ***Absence of right-sided motor function below T1***
- The **right lateral corticospinal tract** controls **voluntary motor function** on the **ipsilateral side** of the body.
- Damage to this tract at T1 would therefore lead to a loss of motor function on the right side below the level of the injury.
*Absence of left-sided proprioception below T1*
- **Proprioception** is carried by the **dorsal columns**, which ascend **ipsilaterally** before decussating in the brainstem.
- Damage to the right lateral corticospinal tract would not affect left-sided proprioception.
*Presence of left-sided Babinski sign*
- A **Babinski sign** (upgoing plantar reflex) indicates an **upper motor neuron lesion**.
- Since the corticospinal tract decussates in the **medulla** (before reaching the spinal cord), a lesion in the **right lateral corticospinal tract at T1** affects motor function on the **right side** of the body.
- Therefore, if a Babinski sign were present, it would be on the **right side**, not the left.
*Absence of left-sided fine touch sensation below T1*
- **Fine touch** sensation is transmitted by the **dorsal columns**, which ascend **ipsilaterally** and decussate in the brainstem.
- Damage to the right lateral corticospinal tract would not affect fine touch sensation on the left side.
*Absence of right-sided temperature sensation below T1*
- **Temperature sensation** is carried by the **spinothalamic tracts**, which decussate at the level of entry into the spinal cord.
- Therefore, a lesion of the right lateral corticospinal tract would not affect temperature sensation on the right side; ipsilateral temperature loss would be due to damage to the right spinothalamic tract, which is located more anterolaterally in the spinal cord.
Somatotopic organization US Medical PG Question 5: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Somatotopic organization Explanation: ***Left anterior cerebral artery***
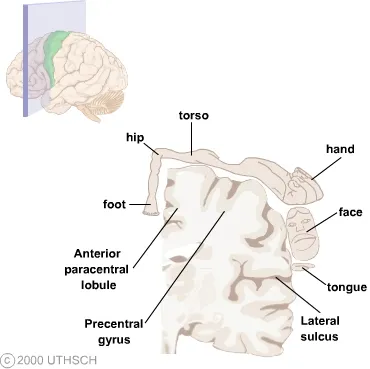
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Somatotopic organization US Medical PG Question 6: A patient with a known spinal cord ependymoma presents to his neurologist for a check up. He complains that he has had difficulty walking, which he attributes to left leg weakness. On exam, he is noted to have 1/5 strength in his left lower extremity, as well as decreased vibration and position sensation in the left lower extremity and decreased pain and temperature sensation in the right lower extremity. Which of the following spinal cord lesions is most consistent with his presentation?
- A. Anterior cord syndrome
- B. Posterior cord syndrome
- C. Syringomyelia
- D. Right-sided Brown-Sequard (hemisection)
- E. Left-sided Brown-Sequard (hemisection) (Correct Answer)
Somatotopic organization Explanation: ***Left-sided Brown-Sequard (hemisection)***
- This syndrome is characterized by **ipsilateral loss of motor function (weakness)** and **proprioception/vibration sensation** below the lesion, along with **contralateral loss of pain and temperature sensation**.
- The patient's left leg weakness, decreased vibration/position sensation in the left lower extremity, and decreased pain/temperature sensation in the right lower extremity perfectly match a **left-sided hemisection of the spinal cord**.
*Anterior cord syndrome*
- This syndrome results in **bilateral motor paralysis** and bilateral loss of **pain and temperature sensation** below the level of the lesion.
- However, **proprioception** and **vibration sense** are typically preserved, which contrasts with the patient's presentation of ipsilateral loss of these senses.
*Posterior cord syndrome*
- This rare syndrome primarily affects the **dorsal columns**, leading to bilateral loss of **vibration and proprioception** below the lesion.
- **Motor function** and **pain/temperature sensation** are largely preserved, which is inconsistent with the patient's significant motor weakness and contralateral pain/temperature loss.
*Syringomelia*
- This condition involves a fluid-filled cavity (syrinx) within the spinal cord, often causing a **cape-like distribution of pain and temperature loss** (crossing the midline) due to damage to the **decussating spinothalamic fibers**.
- While it can cause weakness, the distinct **ipsilateral proprioceptive loss** and **contralateral pain/temperature loss** seen in this patient are not typical for syringomyelia.
*Right-sided Brown-Sequard (hemisection)*
- A right-sided Brown-Sequard syndrome would present with **right-sided weakness** and **loss of proprioception/vibration sensation**, along with **left-sided loss of pain and temperature sensation**.
- This is the **opposite of the patient's presentation** of left-sided weakness and ipsilateral proprioceptive loss.
Somatotopic organization US Medical PG Question 7: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
Somatotopic organization Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
Somatotopic organization US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Somatotopic organization Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Somatotopic organization US Medical PG Question 9: A 68-year-old man is brought to the emergency department by ambulance after he was found to be altered at home. Specifically, his wife says that he fell and was unable to get back up while walking to bed. When she approached him, she found that he was unable to move his left leg. His past medical history is significant for hypertension, atrial fibrillation, and diabetes. In addition, he has a 20-pack-year smoking history. On presentation, he is found to still have difficulty moving his left leg though motor function in his left arm is completely intact. The cause of this patient's symptoms most likely occurred in an artery supplying which of the following brain regions?
- A. Motor cortex (ACA) (Correct Answer)
- B. Cerebellum (PICA/SCA)
- C. Occipital cortex (PCA)
- D. Brainstem (Vertebrobasilar)
- E. Motor cortex (MCA)
Somatotopic organization Explanation: ***Motor cortex (ACA)***
- The patient's inability to move his **left leg** while his **left arm** remains intact points to an injury in the **right cerebral hemisphere** affecting the leg area of the motor cortex.
- The leg area of the **primary motor cortex** is primarily supplied by the **anterior cerebral artery (ACA)**, making an ACA stroke the most likely cause.
*Motor cortex (MCA)*
- The **middle cerebral artery (MCA)** primarily supplies the motor cortex areas responsible for the **face and arm**, not typically isolated leg weakness.
- If the MCA were affected, you would expect to see involvement of the face and/or arm on the contralateral side in addition to leg weakness.
*Brainstem (Vertebrobasilar)*
- A **brainstem stroke** would likely present with more widespread neurological deficits, including **cranial nerve palsies**, ataxia, or altered consciousness.
- Isolated contralateral leg weakness without arm involvement is not characteristic of a brainstem lesion.
*Cerebellum (PICA/SCA)*
- The **cerebellum** is primarily involved in **coordination and balance**, not direct motor strength.
- A cerebellar stroke would present with symptoms like **ataxia**, dysarthria, or nystagmus, not isolated paralysis.
*Occipital cortex (PCA)*
- The **occipital cortex** is primarily responsible for **vision**.
- A posterior cerebral artery (PCA) stroke would typically cause **visual field defects** (e.g., contralateral homonymous hemianopia) rather than motor weakness.
Somatotopic organization US Medical PG Question 10: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Somatotopic organization Explanation: ***5,1,2,3,4***
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
More Somatotopic organization US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.