Origin and course of lateral corticospinal tract US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Origin and course of lateral corticospinal tract. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Origin and course of lateral corticospinal tract US Medical PG Question 1: A 74-year-old male is brought to the emergency department 1 hour after he fell from the top of the staircase at home. He reports pain in his neck as well as weakness of his upper extremities. He is alert and immobilized in a cervical collar. He has hypertension treated with hydrochlorothiazide. His pulse is 90/min and regular, respirations are 18/min, and blood pressure is 140/70 mmHg. Examination shows bruising and midline cervical tenderness. Neurologic examination shows diminished strength and sensation to pain and temperature in the upper extremities, particularly in the hands. Upper extremity deep tendon reflexes are absent. Strength, sensation, and reflexes in the lower extremities are intact. Anal sensation and tone are present. Babinski's sign is absent bilaterally. Which of the following is most likely to confirm the cause of this patient's neurologic examination findings?
- A. CT angiography of the neck
- B. MRI of the cervical spine without contrast (Correct Answer)
- C. X-ray of the cervical spine
- D. CT of the cervical spine with contrast
- E. Cervical myelography
Origin and course of lateral corticospinal tract Explanation: ***MRI of the cervical spine without contrast***
- This patient presents with symptoms consistent with **central cord syndrome**, characterized by greater weakness in the upper extremities than the lower extremities, often following a hyperextension injury in older adults with pre-existing cervical spondylosis. **MRI is the gold standard for visualizing soft tissue injuries**, including spinal cord compression, edema, or hemorrhage, which are typical causes of central cord syndrome.
- Given the primary concern for spinal cord injury and the detailed neurological deficits indicating specific cord involvement, **MRI** offers the best resolution for evaluating the extent of cord damage, disc herniation, ligamentous injury, and pre-existing degenerative changes.
*CT angiography of the neck*
- **CT angiography** primarily evaluates the **vascular structures** of the neck (e.g., carotid and vertebral arteries) for dissection, stenosis, or occlusion.
- While vascular injury could occur in trauma, the patient's neurological findings (disproportionate upper extremity weakness, pain and temperature sensation loss) point more directly to **spinal cord pathology** rather than isolated vascular compromise as the primary cause.
*X-ray of the cervical spine*
- **X-rays** are useful for initial screening of **bony fractures** and significant dislocations but offer limited information about soft tissues, such as the spinal cord, ligaments, or intervertebral discs.
- They cannot adequately visualize the spinal cord damage responsible for the patient's specific neurological deficits, making it insufficient for confirming the cause of central cord syndrome.
*CT of the cervical spine with contrast*
- **CT scans** excel at visualizing **bony structures** and acute fractures, but even with contrast, they provide less detail of the **spinal cord parenchyma** and soft tissue ligaments compared to MRI.
- **Contrast** is typically used to highlight vascular structures, inflammatory processes, or tumors, which are not the primary diagnostic concerns suggested by this patient's acute post-traumatic presentation of central cord syndrome.
*Cervical myelography*
- **Myelography** involves injecting contrast into the subarachnoid space, followed by X-ray or CT imaging, to outline the spinal cord and nerve roots.
- While it can identify **spinal cord compression**, it is an **invasive procedure** with risks (e.g., headache, seizures) and has largely been replaced by the non-invasive and superior soft tissue imaging capabilities of MRI, especially in acute trauma.
Origin and course of lateral corticospinal tract US Medical PG Question 2: A 17-year-old boy is brought to the emergency department after being stabbed with a knife during an altercation. Physical examination shows a 4-cm stab wound on the right lateral border of the T1 spinous process. An MRI of the spinal cord shows damage to the area of the right lateral corticospinal tract at the level of T1. Further evaluation will most likely show which of the following findings?
- A. Absence of right-sided motor function below T1 (Correct Answer)
- B. Absence of left-sided proprioception below T1
- C. Presence of left-sided Babinski sign
- D. Absence of left-sided fine touch sensation below T1
- E. Absence of right-sided temperature sensation below T1
Origin and course of lateral corticospinal tract Explanation: ***Absence of right-sided motor function below T1***
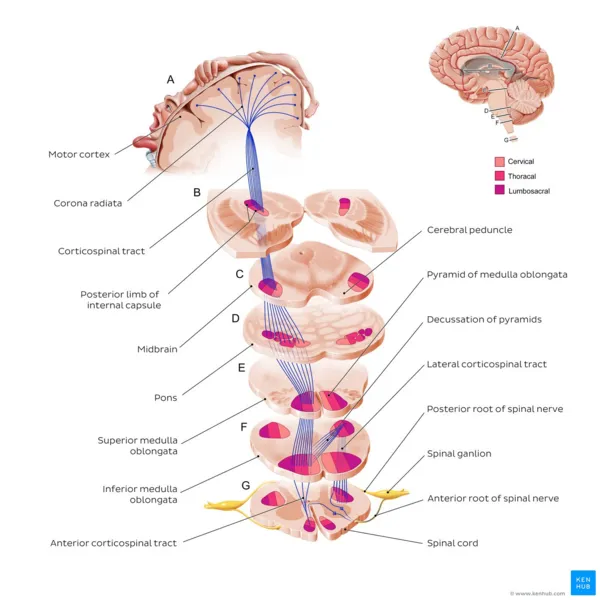
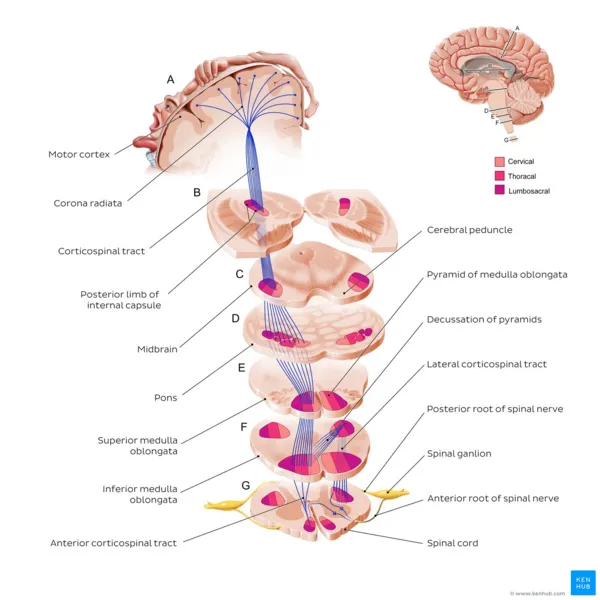
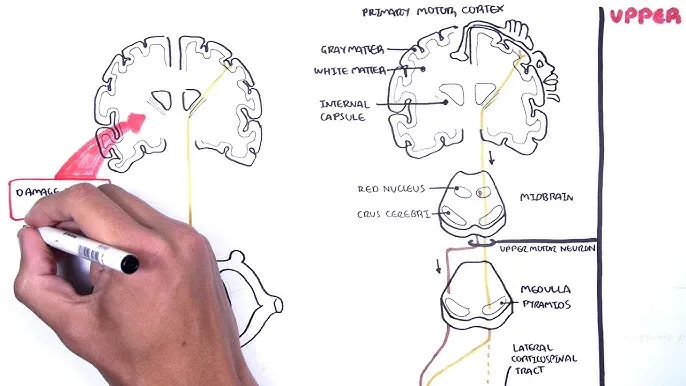
- The **right lateral corticospinal tract** controls **voluntary motor function** on the **ipsilateral side** of the body.
- Damage to this tract at T1 would therefore lead to a loss of motor function on the right side below the level of the injury.
*Absence of left-sided proprioception below T1*
- **Proprioception** is carried by the **dorsal columns**, which ascend **ipsilaterally** before decussating in the brainstem.
- Damage to the right lateral corticospinal tract would not affect left-sided proprioception.
*Presence of left-sided Babinski sign*
- A **Babinski sign** (upgoing plantar reflex) indicates an **upper motor neuron lesion**.
- Since the corticospinal tract decussates in the **medulla** (before reaching the spinal cord), a lesion in the **right lateral corticospinal tract at T1** affects motor function on the **right side** of the body.
- Therefore, if a Babinski sign were present, it would be on the **right side**, not the left.
*Absence of left-sided fine touch sensation below T1*
- **Fine touch** sensation is transmitted by the **dorsal columns**, which ascend **ipsilaterally** and decussate in the brainstem.
- Damage to the right lateral corticospinal tract would not affect fine touch sensation on the left side.
*Absence of right-sided temperature sensation below T1*
- **Temperature sensation** is carried by the **spinothalamic tracts**, which decussate at the level of entry into the spinal cord.
- Therefore, a lesion of the right lateral corticospinal tract would not affect temperature sensation on the right side; ipsilateral temperature loss would be due to damage to the right spinothalamic tract, which is located more anterolaterally in the spinal cord.
Origin and course of lateral corticospinal tract US Medical PG Question 3: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
Origin and course of lateral corticospinal tract Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Origin and course of lateral corticospinal tract US Medical PG Question 4: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
Origin and course of lateral corticospinal tract Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
Origin and course of lateral corticospinal tract US Medical PG Question 5: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Origin and course of lateral corticospinal tract Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Origin and course of lateral corticospinal tract US Medical PG Question 6: A 61-year-old man is brought to the emergency department by his son after collapsing to the ground while at home. His son immediately performed cardiopulmonary resuscitation and later the patient underwent successful defibrillation after being evaluated by the emergency medical technician. The patient has a medical history of hypertension, hyperlipidemia, and type II diabetes mellitus. He has smoked one-half pack of cigarettes for approximately 30 years. The patient was admitted to the cardiac intensive care unit, and after a few days developed acute onset right upper extremity weakness. His temperature is 99°F (37.2°C), blood pressure is 145/91 mmHg, pulse is 102/min and irregularly irregular, and respirations are 16/min. On physical examination, the patient is alert and orientated to person, place, and time. His language is fluent and he is able to name, repeat, and read. His strength is 5/5 throughout except in the right hand, wrist, and arm, which is 2/5. Based on this patient's clinical presentation, the affected neuronal fibers decussate at which level of the central nervous system?
- A. Caudal medulla (Correct Answer)
- B. Pons
- C. Spinal cord
- D. Primary motor cortex
- E. Thalamus
Origin and course of lateral corticospinal tract Explanation: ***Caudal medulla***
- The patient's **acute right upper extremity weakness** following a cardiac event suggests a **stroke** affecting the left motor pathways.
- The **pyramidal decussation**, where the vast majority of the **corticospinal tracts** cross to the contralateral side, occurs in the **caudal medulla**.
*Pons*
- While the corticospinal tracts pass through the pons, they generally do not decussate at this level.
- Lesions in the pons often present with **ipsilateral cranial nerve** deficits and **contralateral body weakness**.
*Spinal cord*
- Only a small percentage (about 10-15%) of the corticospinal fibers decussate in the spinal cord, and these form the **anterior corticospinal tract**, mainly supplying axial muscles.
- Significant contralateral upper extremity weakness implies a lesion higher up, before the spinal cord.
*Primary motor cortex*
- Lesions in the primary motor cortex would cause contralateral weakness, but the decussation itself occurs in the brainstem, not the cortex.
- The motor cortex is where the motor commands originate, not where they cross over.
*Thalamus*
- The thalamus is a major **sensory relay station** and also plays a role in motor control, but it is not the site of decussation for the corticospinal tracts.
- Thalamic lesions typically cause **sensory deficits** (e.g., contralateral hemianesthesia) and sometimes ataxia or dyskinesias.
Origin and course of lateral corticospinal tract US Medical PG Question 7: A 54-year-old man is referred to a tertiary care hospital with a history of 5 months of progressive difficulty in walking and left leg numbness. He first noticed mild gait unsteadiness and later developed gradual right leg weakness. His left leg developed progressive numbness and tingling. His blood pressure is 138/88 mm Hg, the heart rate is 72/min, and the temperature is 36.7°C (98.2°F). On physical examination, he is alert and oriented to person, place, and time. Cranial nerves are intact. Muscle strength is 5/5 in both upper extremities and left lower extremity, but 3/5 in the right leg with increased tone. The plantar reflex is extensor on the right. Pinprick sensation is decreased on the left side below the umbilicus. Vibration and joint position senses are decreased in the right foot and leg. All sensations are normal in the upper extremities. Finger-to-nose and heel-to-shin testing are normal. This patient’s lesion is most likely located in which of the following parts of the nervous system?
- A. Right hemi-spinal cord (Correct Answer)
- B. Right frontal lobe
- C. Left frontal lobe
- D. Left hemi-spinal cord
- E. Right pons
Origin and course of lateral corticospinal tract Explanation: ***Right hemi-spinal cord***
- The patient presents with **ipsilateral motor weakness** (right leg 3/5 with increased tone and extensor plantar reflex) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the right foot and leg) along with **contralateral spinothalamic loss** (decreased pinprick sensation on the left side below the umbilicus). This classic combination of symptoms is known as **Brown-Séquard syndrome**, which results from a lesion affecting one half of the spinal cord.
- The specific pattern of deficits—motor and proprioceptive loss on the same side as the lesion, and pain/temperature loss on the opposite side—localizes the lesion to the **right half of the spinal cord**.
*Right frontal lobe*
- A lesion in the right frontal lobe would typically cause **contralateral motor weakness** (left-sided) and potentially cognitive or behavioral changes, without the specific sensory dissociation seen in this patient.
- It would not explain the **ipsilateral proprioceptive loss** or the **contralateral pain/temperature loss** at different levels as observed in this case.
*Left frontal lobe*
- A lesion in the left frontal lobe would primarily result in **contralateral motor weakness** (right-sided), similar to the right leg weakness observed, but it would not explain the other sensory deficits, particularly the **contralateral pain/temperature loss** (right-sided in this scenario) and the **ipsilateral proprioceptive loss**.
- **Speech disturbances** (aphasia) are also common with left frontal lobe lesions, depending on the exact location, which are not mentioned here.
*Left hemi-spinal cord*
- A lesion in the left hemi-spinal cord would cause **ipsilateral motor weakness** (left leg weakness) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the left foot and leg), along with **contralateral spinothalamic loss** (decreased pinprick sensation on the right side).
- This pattern is the opposite of the patient's symptoms, which show right-sided weakness and proprioceptive loss, and left-sided pain/temperature loss.
*Right pons*
- A lesion in the pons would typically present with a **combination of cranial nerve deficits** (e.g., facial sensory or motor abnormalities, gaze palsies) **and long tract signs**, often affecting both sides of the body due to the compact nature of the brainstem.
- While it could cause long tract signs, the specific pattern of **dissociated ipsilateral and contralateral sensory/motor deficits** observed below the umbilical level is highly characteristic of a spinal cord lesion and less so of a pontine lesion.
Origin and course of lateral corticospinal tract US Medical PG Question 8: A 70-year-old man is admitted with fever, chills, and rigor which have lasted for 4 days. He also complains of associated recent-onset fatigue. Past medical history is insignificant. He drinks a can of beer every night. His temperature is 39.0°C (102.2°F), pulse is 120/min, blood pressure is 122/80 mm Hg, and respirations are 14/min. Physical examination reveals splinter hemorrhages in the fingernails, and a 2/6 apical pansystolic murmur is heard which was not present during his last visit a month ago. A transoesophageal echocardiogram shows evidence of vegetations over the mitral valve. Blood cultures are taken from 3 different sites, which reveal the growth of Streptococcus gallolyticus. The patient is started on the appropriate antibiotic therapy which results in rapid clinical improvement. Which of the following would be the best next step in management in this patient after he is discharged?
- A. Refer for an outpatient upper GI endoscopy
- B. Repeat the transesophageal echocardiography
- C. Prepare and schedule valve replacement surgery
- D. Perform a transthoracic echocardiogram
- E. Refer for an outpatient colonoscopy (Correct Answer)
Origin and course of lateral corticospinal tract Explanation: ***Refer for an outpatient colonoscopy***
- *Streptococcus gallolyticus* (formerly *Streptococcus bovis* biotype I and II) is strongly associated with **colorectal carcinoma** and other **gastrointestinal pathologies**.
- Given the patient's age and the presence of *S. gallolyticus* endocarditis, a **colonoscopy** is essential to screen for underlying colorectal malignancy.
*Refer for an outpatient upper GI endoscopy*
- While *S. gallolyticus* can be linked to gastrointestinal issues, its association is predominantly with **colonic lesions**, not typically upper GI lesions.
- An upper GI endoscopy would be less targeted and therefore not the *best next step* compared to colonoscopy in this specific scenario.
*Prepare and schedule valve replacement surgery*
- The patient has shown **rapid clinical improvement** with antibiotic therapy, suggesting that the infection is responding well to treatment.
- Valve replacement surgery is typically reserved for cases with **severe heart failure**, large vegetations with embolic risk, or failure of medical therapy, none of which are described here.
*Perform a transthoracic echocardiogram*
- A **transesophageal echocardiogram (TEE)** has already confirmed vegetations on the mitral valve, which is a more sensitive and specific test for endocarditis than a transthoracic echocardiogram (TTE).
- Repeating a less sensitive imaging study would not add significant diagnostic value at this stage, especially given the clinical improvement.
*Repeat the transesophageal echocardiography*
- The initial TEE confirmed the diagnosis and the presence of vegetations; repeating it immediately post-treatment completion is usually performed to ensure clearance, but the **most urgent next step** is to address the underlying cause of the *S. gallolyticus* infection.
- While follow-up imaging is important, evaluating for **colorectal malignancy** takes precedence due to the strong association with this specific organism.
Origin and course of lateral corticospinal tract US Medical PG Question 9: A 60-year-old man is brought to the emergency department because of a 1-hour history of disorientation and slurred speech. He has a 10-year history of hypertension and hypercholesterolemia. His blood pressure is 210/110 mm Hg, and pulse is 90/min. Once the patient is stabilized, an MRI of the brain is performed, which shows an infarct of the left precentral gyrus involving the facial motor cortex. Given the MRI findings, which of the following neurological findings would most be expected?
- A. Inability to raise the right eyebrow
- B. Drooping of the left eyelid
- C. Loss of taste in the posterior third of the right half of the tongue
- D. Decreased lacrimation of the left eye
- E. Flattening of the right nasolabial fold (Correct Answer)
Origin and course of lateral corticospinal tract Explanation: ***Flattening of the right nasolabial fold***
- An infarct in the **left precentral gyrus** affecting the facial nerve region impacts the **contralateral lower face** due to the nature of upper motor neuron innervation.
- This typically results in **weakness or paralysis of the muscles of facial expression** on the right side, manifest as a flattened nasolabial fold.
*Inability to raise the right eyebrow*
- The muscles of the **upper face** (e.g., forehead, eyebrow) receive **bilateral innervation** from the motor cortex.
- Therefore, an upper motor neuron lesion in one hemisphere, such as the left precentral gyrus infarct, usually **does not cause significant weakness** in raising the contralateral eyebrow.
*Drooping of the left eyelid*
- Drooping of the left eyelid (**ptosis**) is often associated with dysfunction of the **oculomotor nerve (CN III)** or **sympathetic pathway** (Horner's syndrome).
- It is not a direct consequence of a precentral gyrus infarct affecting facial nerve motor control.
*Loss of taste in the posterior third of the right half of the tongue*
- Taste sensation from the posterior third of the tongue is primarily mediated by the **glossopharyngeal nerve (CN IX)**.
- An infarct in the precentral gyrus, which is part of the motor cortex, would not directly affect taste sensation.
*Decreased lacrimation of the left eye*
- Lacrimation is controlled by parasympathetic fibers traveling with the **facial nerve (CN VII)**, but these fibers typically originate from the brainstem, not directly from the precentral gyrus.
- A cortical infarct primarily affects **motor control of facial muscles**, not autonomic functions like tearing.
Origin and course of lateral corticospinal tract US Medical PG Question 10: A 52-year-old man with multiple sclerosis presents with progressive bilateral leg weakness and spasticity over 3 years, now requiring a wheelchair. MRI shows demyelinating plaques in the cervical and thoracic spinal cord lateral columns bilaterally, corona radiata, and periventricular white matter. He has no sensory level but has impaired vibration sense in the feet. Upper extremities are minimally affected. Evaluate which anatomical principle best explains the leg-predominant motor disability despite multiple CNS lesions.
- A. Cervical cord lateral corticospinal tract plaques preferentially affect medially positioned leg fibers with longer distance from cortex
- B. Corona radiata lesions selectively damage leg motor fibers due to vascular watershed vulnerability
- C. Thoracic cord lesions interrupt leg motor function while cervical lesions spare arm innervation
- D. Periventricular plaques selectively affect leg motor cortex projections
- E. Demyelination affects longest corticospinal axons (to legs) more than shorter axons (to arms) due to length-dependent vulnerability (Correct Answer)
Origin and course of lateral corticospinal tract Explanation: ***Demyelination affects longest corticospinal axons (to legs) more than shorter axons (to arms) due to length-dependent vulnerability***
- The **corticospinal tract** axons innervating the lower limbs are the longest in the body, traveling from the **motor cortex** all the way to the lumbar/sacral spinal cord.
- Longer axons have a greater **total myelin surface area** and higher metabolic demands, making them more susceptible to cumulative damage from **demyelinating plaques** across multiple CNS levels.
*Cervical cord lateral corticospinal tract plaques preferentially affect medially positioned leg fibers with longer distance from cortex*
- While it is true that leg fibers are found more **medially** in the lateral corticospinal tract compared to arm fibers, distance from the cortex is not the primary anatomical driver in this localized context.
- MS plaques are typically **multifocal** and do not consistently show a preference for the medial aspect of the tract based solely on fiber distance.
*Corona radiata lesions selectively damage leg motor fibers due to vascular watershed vulnerability*
- **Multiple sclerosis** is an inflammatory, immune-mediated disease of **white matter**, not a primary vascular or ischemic stroke-related disorder.
- **Watershed vulnerability** explains specific types of infarctions but does not account for the pattern of progressive demyelination seen in MS.
*Thoracic cord lesions interrupt leg motor function while cervical lesions spare arm innervation*
- This patient has documented lesions in the **cervical spinal cord**, which should theoretically affect both upper and lower limb fibers if localized injury were the only factor.
- This explanation fails to account for why the **cervical plaques** (which contain fibers for both arms and legs) preferentially result in **leg-predominant** deficits.
*Periventricular plaques selectively affect leg motor cortex projections*
- **Periventricular plaques** are common in MS but they do not specifically target fibers for the legs more than those for other body parts based on cortical mapping alone.
- The disability pattern in MS is better explained by the **cumulative effect** of multiple lesions on the longest axonal pathways rather than a specific cortical localization.
More Origin and course of lateral corticospinal tract US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.