Origin and course of anterior corticospinal tract US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Origin and course of anterior corticospinal tract. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Origin and course of anterior corticospinal tract US Medical PG Question 1: A 45-year-old man is brought to the emergency department by ambulance after a motor vehicle collision. He is not responsive to verbal commands and is unable to provide any history. His pulse is 108/min and regular. Physical examination shows ecchymoses over the neck and back. Neurological examination indicates damage to the spinal cord at the level shown in the illustration. This patient's injury is most likely located at which of the following levels of the spinal cord?
- A. C2
- B. S2
- C. L4
- D. T6 (Correct Answer)
- E. S4
Origin and course of anterior corticospinal tract Explanation: ***T6***
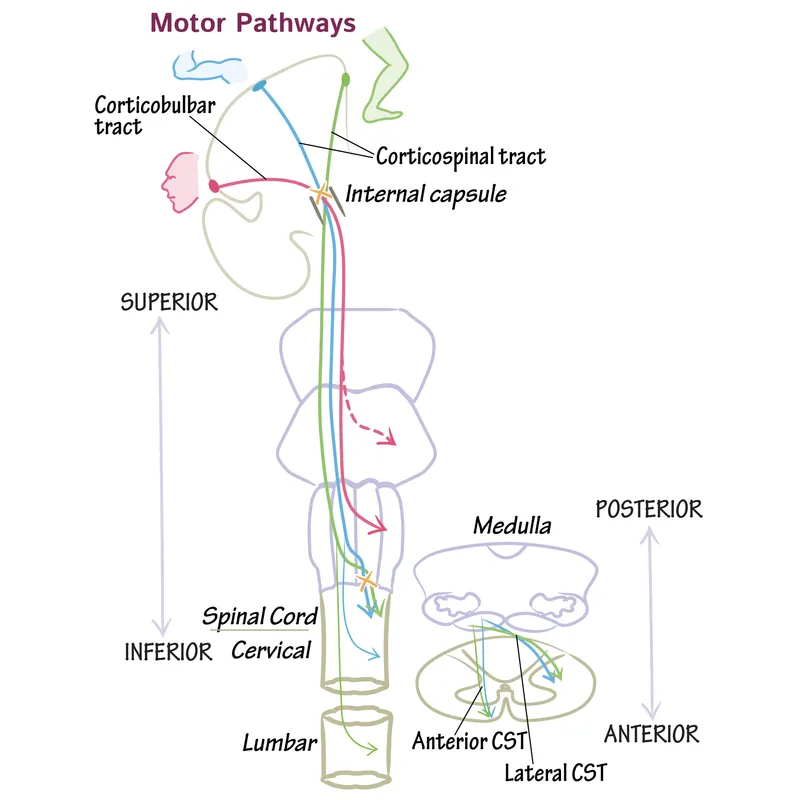
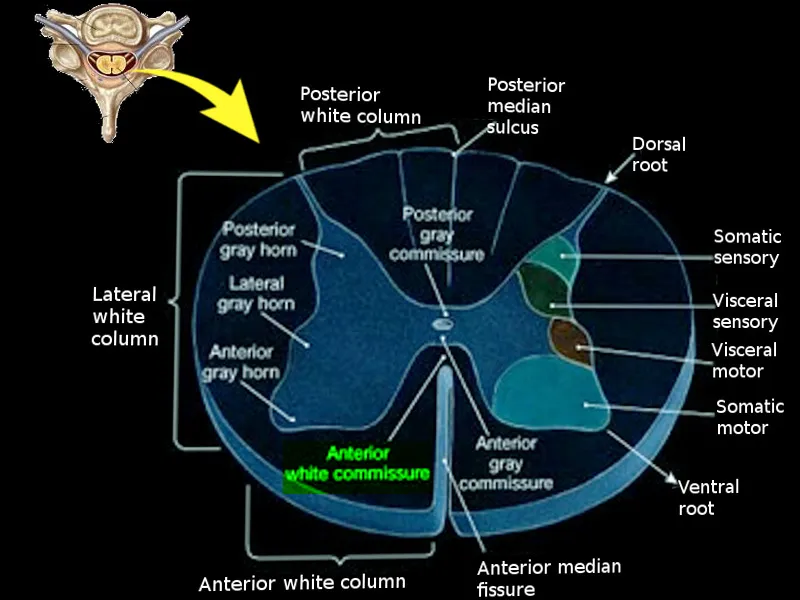
- The correct answer depends on identifying the spinal cord level shown in the illustration (cross-sectional anatomy).
- Injury at **T6** (mid-thoracic level) can present with:
- **Paraplegia** with loss of lower extremity function
- **Sensory level** at approximately the xiphoid process (T6 dermatome)
- Risk of **autonomic dysreflexia** if injury is complete (occurs with injuries at or above T6)
- Preserved upper extremity function and respiratory capacity
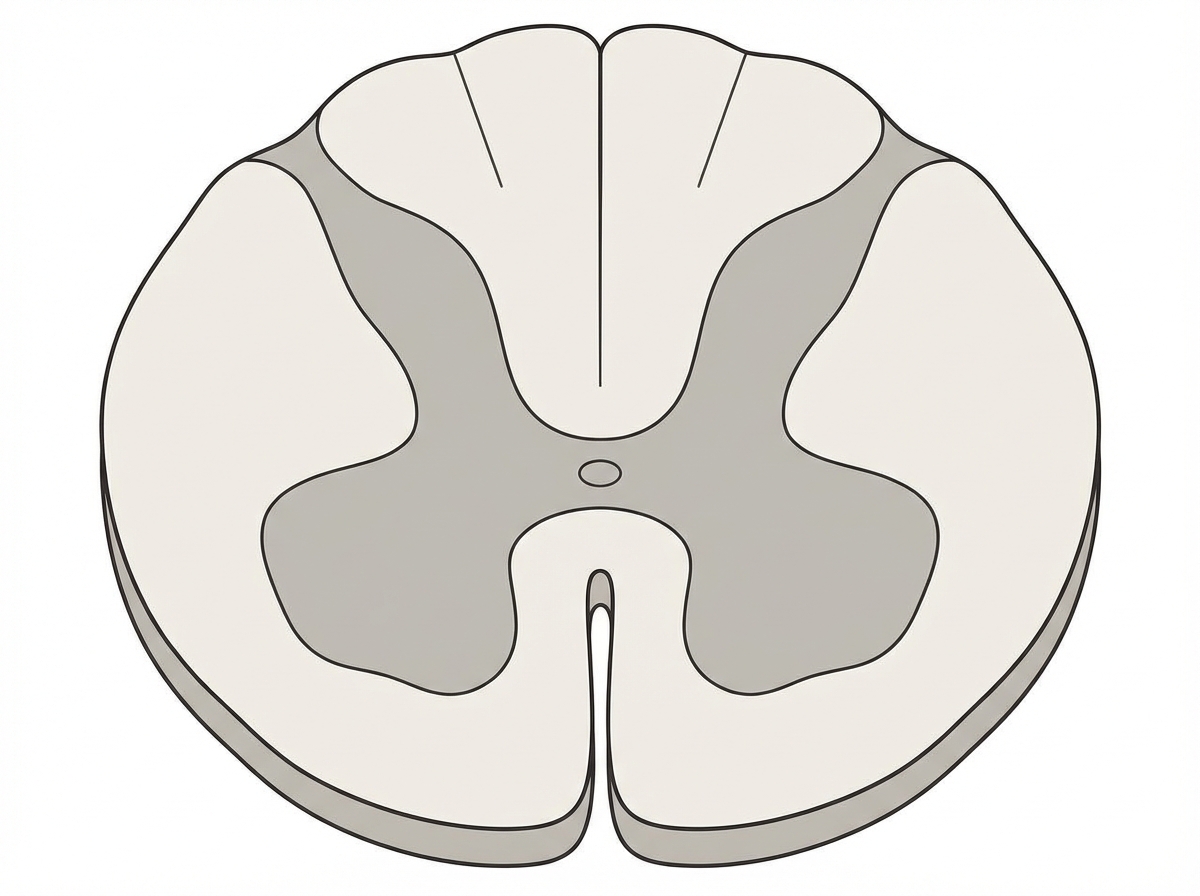
- The mid-thoracic spinal cord cross-section would show the characteristic butterfly-shaped gray matter with surrounding white matter tracts.
*C2*
- **C2** injury is a high cervical lesion that would result in:
- **Quadriplegia** (tetraplegia) affecting all four extremities
- Severe **respiratory compromise** requiring mechanical ventilation (phrenic nerve C3-C5)
- High mortality if untreated
- Cross-sectional anatomy at C2 shows enlarged gray matter for upper limb innervation.
*S2*
- **S2** injury is at the level of the conus medullaris/cauda equina and would cause:
- **Bowel and bladder dysfunction** (loss of parasympathetic control)
- **Saddle anesthesia** (loss of perineal sensation)
- Possible lower extremity weakness
- No significant autonomic instability
- Would not explain the clinical presentation in the upper body.
*L4*
- **L4** injury affects the lumbar enlargement and would cause:
- **Lower extremity weakness** (quadriceps, tibialis anterior)
- **Diminished patellar reflex**
- Sensory loss in the medial leg and foot
- Bowel/bladder may be affected
- Cross-section shows prominent gray matter for lower limb innervation.
*S4*
- **S4** is the lowest sacral level and injury would cause:
- Very limited dysfunction: **anal sphincter weakness**
- **Loss of anocutaneous reflex**
- Minimal motor or sensory deficits elsewhere
- Would not cause systemic neurological compromise.
Origin and course of anterior corticospinal tract US Medical PG Question 2: A neurology resident sees a stroke patient on the wards. This 57-year-old man presented to the emergency department after sudden paralysis of his right side. He was started on tissue plasminogen activator within 4 hours, as his wife noticed the symptoms and immediately called 911. When the resident asks the patient how he is doing, he replies by saying that his apartment is on Main St. He does not seem to appropriately answer the questions being asked, but rather speaks off topic. He is able to repeat the word "fan." His consciousness is intact, and his muscle tone and reflexes are normal. Upon striking the lateral part of his sole, his big toe extends upward and the other toes fan out. Which of the following is the area most likely affected in his condition?
- A. Caudate nucleus
- B. Broca’s area
- C. Arcuate fasciculus
- D. Temporal lobe (Correct Answer)
- E. Cuneus gyrus
Origin and course of anterior corticospinal tract Explanation: ***Temporal lobe***
- The patient exhibits features of **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** ("apartment is on Main St." when asked how he is), poor comprehension, and the ability to repeat words. **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus**.
- **Sudden paralysis of the right side** indicates involvement of the left cerebral hemisphere (**contralateral motor cortex** lesion), while speech disturbances point to the dominant hemisphere, which is typically the **left temporal lobe**.
*Caudate nucleus*
- Lesions of the **caudate nucleus** are primarily associated with **movement disorders** (e.g., chorea) and **behavioral changes**, not typically with fluent aphasia as described.
- While it plays a role in cognitive functions, its direct involvement in the specific language deficits presented is less likely.
*Broca’s area*
- Damage to **Broca's area**, located in the **frontal lobe**, causes **Broca's aphasia**, characterized by **non-fluent, halting speech** with good comprehension and poor repetition.
- The patient's speech is **fluent**, though off-topic, which contrasts with the typical presentation of Broca's aphasia.
*Arcuate fasciculus*
- The **arcuate fasciculus** connects Broca's and Wernicke's areas, and damage to it typically causes **conduction aphasia**, characterized by **impaired repetition** despite fluent speech and good comprehension.
- While the patient has impaired comprehension, his ability to repeat "fan" makes conduction aphasia less likely than Wernicke's aphasia, where repetition can vary but comprehension is profoundly affected.
*Cuneus gyrus*
- The **cuneus gyrus** is located in the **occipital lobe** and is primarily involved in **visual processing**.
- Damage to this area would lead to **visual field deficits** (e.g., hemianopia) rather than the language and comprehension problems described.
Origin and course of anterior corticospinal tract US Medical PG Question 3: A 17-year-old boy is brought to the emergency department after being stabbed with a knife during an altercation. Physical examination shows a 4-cm stab wound on the right lateral border of the T1 spinous process. An MRI of the spinal cord shows damage to the area of the right lateral corticospinal tract at the level of T1. Further evaluation will most likely show which of the following findings?
- A. Absence of right-sided motor function below T1 (Correct Answer)
- B. Absence of left-sided proprioception below T1
- C. Presence of left-sided Babinski sign
- D. Absence of left-sided fine touch sensation below T1
- E. Absence of right-sided temperature sensation below T1
Origin and course of anterior corticospinal tract Explanation: ***Absence of right-sided motor function below T1***
- The **right lateral corticospinal tract** controls **voluntary motor function** on the **ipsilateral side** of the body.
- Damage to this tract at T1 would therefore lead to a loss of motor function on the right side below the level of the injury.
*Absence of left-sided proprioception below T1*
- **Proprioception** is carried by the **dorsal columns**, which ascend **ipsilaterally** before decussating in the brainstem.
- Damage to the right lateral corticospinal tract would not affect left-sided proprioception.
*Presence of left-sided Babinski sign*
- A **Babinski sign** (upgoing plantar reflex) indicates an **upper motor neuron lesion**.
- Since the corticospinal tract decussates in the **medulla** (before reaching the spinal cord), a lesion in the **right lateral corticospinal tract at T1** affects motor function on the **right side** of the body.
- Therefore, if a Babinski sign were present, it would be on the **right side**, not the left.
*Absence of left-sided fine touch sensation below T1*
- **Fine touch** sensation is transmitted by the **dorsal columns**, which ascend **ipsilaterally** and decussate in the brainstem.
- Damage to the right lateral corticospinal tract would not affect fine touch sensation on the left side.
*Absence of right-sided temperature sensation below T1*
- **Temperature sensation** is carried by the **spinothalamic tracts**, which decussate at the level of entry into the spinal cord.
- Therefore, a lesion of the right lateral corticospinal tract would not affect temperature sensation on the right side; ipsilateral temperature loss would be due to damage to the right spinothalamic tract, which is located more anterolaterally in the spinal cord.
Origin and course of anterior corticospinal tract US Medical PG Question 4: A 37-year-old man presents to his primary care provider complaining of bilateral arm numbness. He was involved in a motor vehicle accident 3 months ago. His past medical history is notable for obesity and psoriatic arthritis. He takes adalimumab. His temperature is 99.3°F (37.4°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. On exam, superficial skin ulcerations are found on his fingers bilaterally. His strength is 5/5 bilaterally in shoulder abduction, arm flexion, arm extension, wrist extension, finger abduction, and thumb flexion. He demonstrates loss of light touch and pinprick response in the distal tips of his 2nd and 5th fingertips and over the first dorsal web space. Vibratory sense is intact in the bilateral upper and lower extremities. Which of the following nervous system structures is most likely affected in this patient?
- A. Cuneate fasciculus
- B. Ventral horns
- C. Anterior corticospinal tract
- D. Spinocerebellar tract
- E. Ventral white commissure (Correct Answer)
Origin and course of anterior corticospinal tract Explanation: ***Ventral white commissure***
- The patient presents with **bilateral loss of pain (pinprick) and light touch sensation** in the upper extremity fingertips, while **vibratory sense is intact** and **motor strength is fully preserved (5/5)**. This dissociated sensory loss pattern is pathognomonic for a lesion affecting the **ventral white commissure**.
- The ventral white commissure contains **decussating fibers of the spinothalamic tract**, which carry pain and temperature sensation from the contralateral body. A lesion here (classically seen in **syringomyelia** affecting the cervical spinal cord) causes **bilateral loss of pain and temperature sensation** in a characteristic distribution while **sparing the dorsal columns** (vibratory sense and proprioception remain intact) and motor pathways.
- The **superficial skin ulcerations** on his fingers are explained by chronic loss of protective pain sensation, leading to unnoticed repetitive trauma. The motor vehicle accident 3 months ago may have precipitated or worsened an underlying syrinx.
- This is the classic **"cape-like" or suspended sensory loss** pattern, though it can present with focal dermatomal involvement as in this case.
*Cuneate fasciculus*
- The cuneate fasciculus is part of the **dorsal column-medial lemniscal pathway** that carries **vibratory sense, proprioception, and fine discriminative touch** from the upper extremities.
- A lesion here would cause **loss of vibratory sense** and proprioception, which are explicitly **intact** in this patient, making this option incorrect.
*Ventral horns*
- The ventral horns contain **lower motor neuron cell bodies** that innervate skeletal muscles.
- Damage would cause **motor deficits** including weakness (reduced strength), muscle atrophy, and fasciculations, none of which are present in this patient who has normal 5/5 strength throughout.
*Anterior corticospinal tract*
- This tract mediates **voluntary motor control**, primarily of axial and proximal muscles.
- Lesions would result in **motor weakness or spasticity**, not the isolated sensory deficits seen in this patient.
*Spinocerebellar tract*
- The spinocerebellar tracts carry **unconscious proprioceptive information** to the cerebellum for motor coordination.
- Damage would manifest as **ataxia, dysmetria, and incoordination**, which are not described in this patient's presentation.
Origin and course of anterior corticospinal tract US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Origin and course of anterior corticospinal tract Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Origin and course of anterior corticospinal tract US Medical PG Question 6: A 26-year-old woman presents to the obstetrics ward to deliver her baby. The obstetrician establishes a pudendal nerve block via intravaginal injection of lidocaine near the tip of the ischial spine. From which of the following nerve roots does the pudendal nerve originate?
- A. L4-L5
- B. S2-S4 (Correct Answer)
- C. L3-L4
- D. L5-S2
- E. L5-S1
Origin and course of anterior corticospinal tract Explanation: ***S2-S4***
- The **pudendal nerve** originates from the **sacral plexus**, specifically from the ventral rami of spinal nerves **S2, S3, and S4**.
- Its origin from these segments is crucial for its function in innervating structures of the **perineum**, **external genitalia**, and the **anal and urethral sphincters**, making it highly relevant for procedures like **pudendal nerve blocks** during childbirth.
*L4-L5*
- Nerve roots **L4-L5** contribute significantly to the **lumbar plexus** and subsequently to nerves like the **femoral nerve** and portions of the **sciatic nerve**.
- These roots are primarily involved in innervating the **lower limbs** (e.g., quadriceps, tibialis anterior) and are not the primary origin of the pudendal nerve.
*L3-L4*
- The **L3-L4** nerve roots are also part of the **lumbar plexus**, chiefly contributing to the **femoral nerve**.
- They are essential for motor innervation of the **anterior thigh muscles** and sensation in this area, distinct from the pudendal nerve's role in the perineum.
*L5-S2*
- While **S2** is part of the pudendal nerve's origin, the inclusion of **L5** and **S1** primarily characterizes the origin of the **sciatic nerve** (which is formed by L4-S3) and its branches, such as the common fibular and tibial nerves.
- These roots are primarily concerned with the **posterior thigh** and **leg innervation**, not the perineum, which differentiates it from the pudendal nerve.
*L5-S1*
- The nerve roots **L5-S1** are key components of the **lumbosacral plexus** and contribute significantly to the **sciatic nerve**, particularly its innervation of the **hamstrings** and certain lower leg muscles.
- This origin does not align with the known roots of the **pudendal nerve** which stems from S2-S4.
Origin and course of anterior corticospinal tract US Medical PG Question 7: A 61-year-old man is brought to the emergency department by his son after collapsing to the ground while at home. His son immediately performed cardiopulmonary resuscitation and later the patient underwent successful defibrillation after being evaluated by the emergency medical technician. The patient has a medical history of hypertension, hyperlipidemia, and type II diabetes mellitus. He has smoked one-half pack of cigarettes for approximately 30 years. The patient was admitted to the cardiac intensive care unit, and after a few days developed acute onset right upper extremity weakness. His temperature is 99°F (37.2°C), blood pressure is 145/91 mmHg, pulse is 102/min and irregularly irregular, and respirations are 16/min. On physical examination, the patient is alert and orientated to person, place, and time. His language is fluent and he is able to name, repeat, and read. His strength is 5/5 throughout except in the right hand, wrist, and arm, which is 2/5. Based on this patient's clinical presentation, the affected neuronal fibers decussate at which level of the central nervous system?
- A. Caudal medulla (Correct Answer)
- B. Pons
- C. Spinal cord
- D. Primary motor cortex
- E. Thalamus
Origin and course of anterior corticospinal tract Explanation: ***Caudal medulla***
- The patient's **acute right upper extremity weakness** following a cardiac event suggests a **stroke** affecting the left motor pathways.
- The **pyramidal decussation**, where the vast majority of the **corticospinal tracts** cross to the contralateral side, occurs in the **caudal medulla**.
*Pons*
- While the corticospinal tracts pass through the pons, they generally do not decussate at this level.
- Lesions in the pons often present with **ipsilateral cranial nerve** deficits and **contralateral body weakness**.
*Spinal cord*
- Only a small percentage (about 10-15%) of the corticospinal fibers decussate in the spinal cord, and these form the **anterior corticospinal tract**, mainly supplying axial muscles.
- Significant contralateral upper extremity weakness implies a lesion higher up, before the spinal cord.
*Primary motor cortex*
- Lesions in the primary motor cortex would cause contralateral weakness, but the decussation itself occurs in the brainstem, not the cortex.
- The motor cortex is where the motor commands originate, not where they cross over.
*Thalamus*
- The thalamus is a major **sensory relay station** and also plays a role in motor control, but it is not the site of decussation for the corticospinal tracts.
- Thalamic lesions typically cause **sensory deficits** (e.g., contralateral hemianesthesia) and sometimes ataxia or dyskinesias.
Origin and course of anterior corticospinal tract US Medical PG Question 8: A 54-year-old man is referred to a tertiary care hospital with a history of 5 months of progressive difficulty in walking and left leg numbness. He first noticed mild gait unsteadiness and later developed gradual right leg weakness. His left leg developed progressive numbness and tingling. His blood pressure is 138/88 mm Hg, the heart rate is 72/min, and the temperature is 36.7°C (98.2°F). On physical examination, he is alert and oriented to person, place, and time. Cranial nerves are intact. Muscle strength is 5/5 in both upper extremities and left lower extremity, but 3/5 in the right leg with increased tone. The plantar reflex is extensor on the right. Pinprick sensation is decreased on the left side below the umbilicus. Vibration and joint position senses are decreased in the right foot and leg. All sensations are normal in the upper extremities. Finger-to-nose and heel-to-shin testing are normal. This patient’s lesion is most likely located in which of the following parts of the nervous system?
- A. Right hemi-spinal cord (Correct Answer)
- B. Right frontal lobe
- C. Left frontal lobe
- D. Left hemi-spinal cord
- E. Right pons
Origin and course of anterior corticospinal tract Explanation: ***Right hemi-spinal cord***
- The patient presents with **ipsilateral motor weakness** (right leg 3/5 with increased tone and extensor plantar reflex) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the right foot and leg) along with **contralateral spinothalamic loss** (decreased pinprick sensation on the left side below the umbilicus). This classic combination of symptoms is known as **Brown-Séquard syndrome**, which results from a lesion affecting one half of the spinal cord.
- The specific pattern of deficits—motor and proprioceptive loss on the same side as the lesion, and pain/temperature loss on the opposite side—localizes the lesion to the **right half of the spinal cord**.
*Right frontal lobe*
- A lesion in the right frontal lobe would typically cause **contralateral motor weakness** (left-sided) and potentially cognitive or behavioral changes, without the specific sensory dissociation seen in this patient.
- It would not explain the **ipsilateral proprioceptive loss** or the **contralateral pain/temperature loss** at different levels as observed in this case.
*Left frontal lobe*
- A lesion in the left frontal lobe would primarily result in **contralateral motor weakness** (right-sided), similar to the right leg weakness observed, but it would not explain the other sensory deficits, particularly the **contralateral pain/temperature loss** (right-sided in this scenario) and the **ipsilateral proprioceptive loss**.
- **Speech disturbances** (aphasia) are also common with left frontal lobe lesions, depending on the exact location, which are not mentioned here.
*Left hemi-spinal cord*
- A lesion in the left hemi-spinal cord would cause **ipsilateral motor weakness** (left leg weakness) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the left foot and leg), along with **contralateral spinothalamic loss** (decreased pinprick sensation on the right side).
- This pattern is the opposite of the patient's symptoms, which show right-sided weakness and proprioceptive loss, and left-sided pain/temperature loss.
*Right pons*
- A lesion in the pons would typically present with a **combination of cranial nerve deficits** (e.g., facial sensory or motor abnormalities, gaze palsies) **and long tract signs**, often affecting both sides of the body due to the compact nature of the brainstem.
- While it could cause long tract signs, the specific pattern of **dissociated ipsilateral and contralateral sensory/motor deficits** observed below the umbilical level is highly characteristic of a spinal cord lesion and less so of a pontine lesion.
Origin and course of anterior corticospinal tract US Medical PG Question 9: A 75-year-old man comes to his primary care physician because he has been having diarrhea and difficulty breathing. The diarrhea has been intermittent with frequent watery stools that occur along with abdominal cramps. Furthermore, the skin on his face and upper chest feels hot and changes color in episodes lasting from a few minutes to hours. Finally, the patient complains of loss of appetite and says that he has unexpectedly lost 20 pounds over the last two months. Based on clinical suspicion, magnetic resonance imaging is obtained showing a small mass in this patient's lungs. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. It also arises in the GI tract (Correct Answer)
- B. Stains positive for vimentin
- C. Has keratin pearls and intercellular bridges
- D. Most common lung cancer in non-smokers and females
- E. Contains psammoma bodies
Origin and course of anterior corticospinal tract Explanation: ***Correct: It also arises in the GI tract***
- The patient's symptoms (diarrhea, flushing, difficulty breathing, weight loss) are highly suggestive of **carcinoid syndrome**, often caused by a **neuroendocrine tumor (NET)** in the lung or gastrointestinal tract that metastasizes to the liver.
- While a lung mass is identified here, **carcinoid tumors** (a type of NET) most commonly originate in the **gastrointestinal tract** (especially the appendix, small intestine, and rectum), making this option strongly associated with the likely cause.
- Carcinoid syndrome typically occurs when liver metastases allow serotonin and other vasoactive substances to bypass hepatic metabolism and enter systemic circulation.
*Incorrect: Stains positive for vimentin*
- **Vimentin** is an intermediate filament typically found in **mesenchymal cells** and is often positive in sarcomas, lymphomas, and melanomas.
- Neuroendocrine tumors, including carcinoid, typically stain positive for **chromogranin** and **synaptophysin**, not vimentin.
*Incorrect: Has keratin pearls and intercellular bridges*
- **Keratin pearls** and **intercellular bridges** are characteristic histological features of **squamous cell carcinoma**, which is a type of non-small cell lung cancer.
- While the patient has a lung mass, his symptoms of carcinoid syndrome point away from squamous cell carcinoma and towards a neuroendocrine tumor.
*Incorrect: Most common lung cancer in non-smokers and females*
- **Adenocarcinoma** is the most common type of lung cancer, particularly prevalent in non-smokers and females.
- However, adenocarcinoma does not typically cause carcinoid syndrome, which is a key clinical presentation in this case.
*Incorrect: Contains psammoma bodies*
- **Psammoma bodies** are concentric, laminated calcified structures seen in certain tumors, such as papillary thyroid carcinoma, meningioma, and serous papillary ovarian cancer.
- They are not characteristic features of neuroendocrine tumors or carcinoid tumors.
Origin and course of anterior corticospinal tract US Medical PG Question 10: A 70-year-old man is admitted with fever, chills, and rigor which have lasted for 4 days. He also complains of associated recent-onset fatigue. Past medical history is insignificant. He drinks a can of beer every night. His temperature is 39.0°C (102.2°F), pulse is 120/min, blood pressure is 122/80 mm Hg, and respirations are 14/min. Physical examination reveals splinter hemorrhages in the fingernails, and a 2/6 apical pansystolic murmur is heard which was not present during his last visit a month ago. A transoesophageal echocardiogram shows evidence of vegetations over the mitral valve. Blood cultures are taken from 3 different sites, which reveal the growth of Streptococcus gallolyticus. The patient is started on the appropriate antibiotic therapy which results in rapid clinical improvement. Which of the following would be the best next step in management in this patient after he is discharged?
- A. Refer for an outpatient upper GI endoscopy
- B. Repeat the transesophageal echocardiography
- C. Prepare and schedule valve replacement surgery
- D. Perform a transthoracic echocardiogram
- E. Refer for an outpatient colonoscopy (Correct Answer)
Origin and course of anterior corticospinal tract Explanation: ***Refer for an outpatient colonoscopy***
- *Streptococcus gallolyticus* (formerly *Streptococcus bovis* biotype I and II) is strongly associated with **colorectal carcinoma** and other **gastrointestinal pathologies**.
- Given the patient's age and the presence of *S. gallolyticus* endocarditis, a **colonoscopy** is essential to screen for underlying colorectal malignancy.
*Refer for an outpatient upper GI endoscopy*
- While *S. gallolyticus* can be linked to gastrointestinal issues, its association is predominantly with **colonic lesions**, not typically upper GI lesions.
- An upper GI endoscopy would be less targeted and therefore not the *best next step* compared to colonoscopy in this specific scenario.
*Prepare and schedule valve replacement surgery*
- The patient has shown **rapid clinical improvement** with antibiotic therapy, suggesting that the infection is responding well to treatment.
- Valve replacement surgery is typically reserved for cases with **severe heart failure**, large vegetations with embolic risk, or failure of medical therapy, none of which are described here.
*Perform a transthoracic echocardiogram*
- A **transesophageal echocardiogram (TEE)** has already confirmed vegetations on the mitral valve, which is a more sensitive and specific test for endocarditis than a transthoracic echocardiogram (TTE).
- Repeating a less sensitive imaging study would not add significant diagnostic value at this stage, especially given the clinical improvement.
*Repeat the transesophageal echocardiography*
- The initial TEE confirmed the diagnosis and the presence of vegetations; repeating it immediately post-treatment completion is usually performed to ensure clearance, but the **most urgent next step** is to address the underlying cause of the *S. gallolyticus* infection.
- While follow-up imaging is important, evaluating for **colorectal malignancy** takes precedence due to the strong association with this specific organism.
More Origin and course of anterior corticospinal tract US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.