Clinical testing of corticospinal tract function US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical testing of corticospinal tract function. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical testing of corticospinal tract function US Medical PG Question 1: You are seeing a patient in clinic who presents with complaints of weakness. Her physical exam is notable for right sided hyperreflexia, as well as the reflex finding shown in the image below. Where is the most likely location of this patient's lesion?
- A. Postcentral gyrus
- B. Neuromuscular junction
- C. Lateral geniculate nucleus
- D. Internal capsule (Correct Answer)
- E. Subthalamic nucleus
Clinical testing of corticospinal tract function Explanation: ***Internal capsule***
- The combination of **right-sided hyperreflexia** (an upper motor neuron sign) and a positive **Babinski sign** (as implied by a video demonstrating this reflex) points to an upper motor neuron lesion.
- The **internal capsule** contains descending motor pathways, and a lesion here would affect the contralateral side of the body, causing **weakness** and upper motor neuron signs.
*Postcentral gyrus*
- The **postcentral gyrus** is the primary somatosensory cortex and primarily deals with sensory processing, not motor output.
- A lesion here would typically cause **contralateral sensory deficits**, such as numbness or loss of proprioception, rather than motor weakness with hyperreflexia.
*Neuromuscular junction*
- Diseases of the **neuromuscular junction**, such as myasthenia gravis, cause **fatigable weakness** without hyperreflexia or other upper motor neuron signs.
- Reflexes are typically normal or decreased in these conditions.
*Lateral geniculate nucleus*
- The **lateral geniculate nucleus** is a thalamic relay center for visual information.
- Lesions here would result in **visual field deficits** (e.g., homonymous hemianopsia), not motor weakness or hyperreflexia.
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia and is involved in motor control, particularly in regulating movement initiation and stopping.
- Lesions here are classically associated with **hemiballismus**, which is characterized by wild, flinging movements, rather than weakness and hyperreflexia.
Clinical testing of corticospinal tract function US Medical PG Question 2: A 62-year-old woman is brought to the physician because of 6 months of progressive weakness in her arms and legs. During this time, she has also had difficulty swallowing and holding her head up. Examination shows pooling of oral secretions. Muscle strength and tone are decreased in the upper extremities. Deep tendon reflexes are 1+ in the right upper and lower extremities, 3+ in the left upper extremity, and 4+ in the left lower extremity. Sensation to light touch, pinprick, and vibration are intact. Which of the following is the most likely diagnosis?
- A. Guillain-Barré syndrome
- B. Amyotrophic lateral sclerosis (Correct Answer)
- C. Spinal muscular atrophy
- D. Myasthenia gravis
- E. Syringomyelia
Clinical testing of corticospinal tract function Explanation: ***Amyotrophic lateral sclerosis***
- The patient presents with a combination of **upper motor neuron (UMN)** signs (hyperreflexia at 3+ and 4+, possibly stiffness contributing to difficulty holding head up) and **lower motor neuron (LMN)** signs (progressive weakness, decreased muscle tone, pooling of oral secretions due to bulbar involvement). This coexistence is pathognomonic for **ALS**.
- The **progressive nature** of the weakness in arms and legs, encompassing both UMN and LMN features without sensory deficits, is characteristic of ALS.
*Guillain-Barré syndrome*
- Typically presents with **acute or subacute onset (days to weeks)** of ascending weakness, often post-infectious, and characteristically causes **areflexia** or severely diminished deep tendon reflexes.
- This patient's symptoms have been progressive over **6 months**, and she exhibits significantly **increased reflexes** in some limbs, which is inconsistent with GBS.
*Spinal muscular atrophy*
- This is a group of **autosomal recessive disorders** that primarily affect **lower motor neurons**, leading to progressive muscle weakness and atrophy, usually presenting in infancy or childhood.
- The patient's age of presentation (62 years old) and the presence of **upper motor neuron signs** (hyperreflexia) rule out SMA.
*Myasthenia gravis*
- Presents with **fluctuating muscle weakness** that worsens with activity and improves with rest, often affecting ocular, bulbar, and limb muscles. It does not typically cause hyperreflexia or sustained upper motor neuron signs.
- While the patient has difficulty swallowing and pooling oral secretions, the **progressive, sustained weakness** and varied deep tendon reflexes (hypo to hyper) are not typical of myasthenia gravis without specific triggers like exertion.
*Syringomyelia*
- Characterized by a **syrinx (cyst) within the spinal cord**, leading to sensory deficits (often **"cape-like" loss of pain and temperature sensation**) and weakness/atrophy due to LMN damage, usually affecting the upper extremities.
- This patient's **intact sensation** and the presence of widespread UMN signs (hyperreflexia in lower limb) make syringomyelia an unlikely diagnosis.
Clinical testing of corticospinal tract function US Medical PG Question 3: A 34-year-old man presents to the neurology clinic for an appointment after having been referred by his family physician. Four months earlier, he presented with worsening upper limb weakness. His primary complaint at that time was that he was unable to play badminton because of increasing difficulty in moving his shoulders and arms. The weakness later progressed, and he now has spontaneous twitching of his leg and thigh muscles throughout the day. He also feels increasingly fatigued. On physical examination, there is significant atrophy of his arm and thigh muscles. Cranial nerves testing is unremarkable. The pupillary light and accommodation reflexes are both normal. Swallowing, speech, and eye movements are all normal. His cousin had similar symptoms at the age of 19 years old. Which of the following is most likely to also be seen in this patient?
- A. Spastic paralysis (Correct Answer)
- B. Positive Romberg sign
- C. Bowel incontinence
- D. Cape-like sensory loss
- E. Paresthesia
Clinical testing of corticospinal tract function Explanation: ***Spastic paralysis***
- The combination of **progressive muscle weakness**, **atrophy**, and **spontaneous muscle twitching (fasciculations)**, with normal cranial nerves except for muscle weakness, points towards a diagnosis of **Amyotrophic Lateral Sclerosis (ALS)**.
- In ALS, there is degeneration of both **upper motor neurons** (leading to spasticity and hyperreflexia) and **lower motor neurons** (leading to weakness, atrophy, and fasciculations), so **spastic paralysis** (due to upper motor neuron involvement) would be expected.
*Positive Romberg sign*
- A **positive Romberg sign** indicates dysfunction in **proprioception** (dorsal columns) or **cerebellar function**, neither of which is characteristic of ALS in its early to mid-stages.
- ALS primarily affects motor neurons, and sensory pathways are typically spared, meaning proprioceptive deficits are not a common feature.
*Bowel incontinence*
- **Bowel and bladder control** are generally preserved in ALS, as the **sphincter muscles** are often spared until very late stages, distinguishing it from conditions like spinal cord injury.
- Incontinence would suggest damage to the **autonomic nervous system** or specific spinal cord segments not primarily affected in ALS.
*Cape-like sensory loss*
- **Cape-like sensory loss** (loss of pain and temperature sensation in a shawl-like distribution over the shoulders and upper trunk) is characteristic of **syringomyelia**, a condition involving a fluid-filled cyst within the spinal cord.
- This symptom pattern is due to damage to the **spinothalamic tracts** as they cross in the spinal cord, and it is not typically seen in ALS, which spares sensory pathways.
*Paresthesia*
- **Paresthesias** (e.g., tingling, numbness) indicate **sensory nerve involvement** or **dorsal column dysfunction**.
- ALS is predominantly a **motor neuron disease**, and sensory symptoms like paresthesia are generally absent or minor, serving as a key differentiating factor from sensory neuropathies.
Clinical testing of corticospinal tract function US Medical PG Question 4: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Clinical testing of corticospinal tract function Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Clinical testing of corticospinal tract function US Medical PG Question 5: A 5-year-old boy who recently emigrated from Nigeria is brought to the emergency department because of a 2-day history of lower leg weakness, swallowing difficulty, and drooling of saliva. He has not yet received any childhood vaccinations. Two days after admission, the patient develops shortness of breath. Pulse oximetry shows an oxygen saturation of 64%. Despite resuscitative efforts, the patient dies of respiratory failure. At autopsy, examination of the spinal cord shows destruction of the anterior horn cells. Neurological examination of this patient would have most likely shown which of the following findings?
- A. Sensory loss
- B. Positive Babinski sign
- C. Hyporeflexia (Correct Answer)
- D. Myoclonus
- E. Pronator drift
Clinical testing of corticospinal tract function Explanation: ***Hyporeflexia***
- The destruction of **anterior horn cells** in the spinal cord is characteristic of **poliomyelitis**, a disease that primarily affects **lower motor neurons**.
- Lower motor neuron lesions lead to symptoms like **flaccid paralysis**, **weakness**, and **hyporeflexia** (diminished or absent reflexes).
*Sensory loss*
- Poliomyelitis specifically targets **motor neurons** and typically spares **sensory pathways**, meaning sensory function remains intact.
- Therefore, **sensory loss** is not a characteristic finding in poliomyelitis.
*Positive Babinski sign*
- A positive Babinski sign (**upgoing plantar reflex**) is indicative of an **upper motor neuron lesion** affecting the **corticospinal tract**.
- Since poliomyelitis involves lower motor neurons, a positive Babinski sign would not be expected.
*Myoclonus*
- **Myoclonus** refers to brief, involuntary twitching of a muscle or a group of muscles, often associated with disorders affecting the **cerebellum**, **brainstem**, or **cortex**.
- It is not a typical neurological finding in **poliomyelitis**, which primarily causes muscle weakness and paralysis.
*Pronator drift*
- **Pronator drift** is a sign of **upper motor neuron weakness** affecting the **contralateral corticospinal tract**, particularly in the arm.
- As **poliomyelitis** is a **lower motor neuron disease**, pronator drift would not be expected as a primary finding.
Clinical testing of corticospinal tract function US Medical PG Question 6: A 61-year-old man is brought to the emergency department by his son after collapsing to the ground while at home. His son immediately performed cardiopulmonary resuscitation and later the patient underwent successful defibrillation after being evaluated by the emergency medical technician. The patient has a medical history of hypertension, hyperlipidemia, and type II diabetes mellitus. He has smoked one-half pack of cigarettes for approximately 30 years. The patient was admitted to the cardiac intensive care unit, and after a few days developed acute onset right upper extremity weakness. His temperature is 99°F (37.2°C), blood pressure is 145/91 mmHg, pulse is 102/min and irregularly irregular, and respirations are 16/min. On physical examination, the patient is alert and orientated to person, place, and time. His language is fluent and he is able to name, repeat, and read. His strength is 5/5 throughout except in the right hand, wrist, and arm, which is 2/5. Based on this patient's clinical presentation, the affected neuronal fibers decussate at which level of the central nervous system?
- A. Caudal medulla (Correct Answer)
- B. Pons
- C. Spinal cord
- D. Primary motor cortex
- E. Thalamus
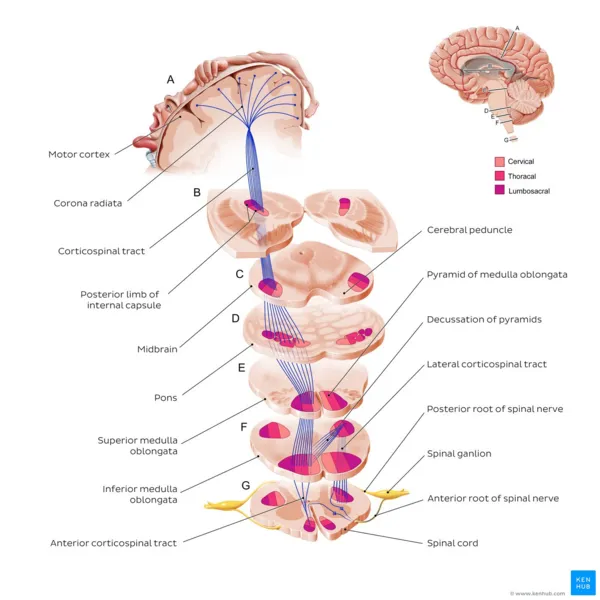
Clinical testing of corticospinal tract function Explanation: ***Caudal medulla***
- The patient's **acute right upper extremity weakness** following a cardiac event suggests a **stroke** affecting the left motor pathways.
- The **pyramidal decussation**, where the vast majority of the **corticospinal tracts** cross to the contralateral side, occurs in the **caudal medulla**.
*Pons*
- While the corticospinal tracts pass through the pons, they generally do not decussate at this level.
- Lesions in the pons often present with **ipsilateral cranial nerve** deficits and **contralateral body weakness**.
*Spinal cord*
- Only a small percentage (about 10-15%) of the corticospinal fibers decussate in the spinal cord, and these form the **anterior corticospinal tract**, mainly supplying axial muscles.
- Significant contralateral upper extremity weakness implies a lesion higher up, before the spinal cord.
*Primary motor cortex*
- Lesions in the primary motor cortex would cause contralateral weakness, but the decussation itself occurs in the brainstem, not the cortex.
- The motor cortex is where the motor commands originate, not where they cross over.
*Thalamus*
- The thalamus is a major **sensory relay station** and also plays a role in motor control, but it is not the site of decussation for the corticospinal tracts.
- Thalamic lesions typically cause **sensory deficits** (e.g., contralateral hemianesthesia) and sometimes ataxia or dyskinesias.
Clinical testing of corticospinal tract function US Medical PG Question 7: A 54-year-old man is referred to a tertiary care hospital with a history of 5 months of progressive difficulty in walking and left leg numbness. He first noticed mild gait unsteadiness and later developed gradual right leg weakness. His left leg developed progressive numbness and tingling. His blood pressure is 138/88 mm Hg, the heart rate is 72/min, and the temperature is 36.7°C (98.2°F). On physical examination, he is alert and oriented to person, place, and time. Cranial nerves are intact. Muscle strength is 5/5 in both upper extremities and left lower extremity, but 3/5 in the right leg with increased tone. The plantar reflex is extensor on the right. Pinprick sensation is decreased on the left side below the umbilicus. Vibration and joint position senses are decreased in the right foot and leg. All sensations are normal in the upper extremities. Finger-to-nose and heel-to-shin testing are normal. This patient’s lesion is most likely located in which of the following parts of the nervous system?
- A. Right hemi-spinal cord (Correct Answer)
- B. Right frontal lobe
- C. Left frontal lobe
- D. Left hemi-spinal cord
- E. Right pons
Clinical testing of corticospinal tract function Explanation: ***Right hemi-spinal cord***
- The patient presents with **ipsilateral motor weakness** (right leg 3/5 with increased tone and extensor plantar reflex) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the right foot and leg) along with **contralateral spinothalamic loss** (decreased pinprick sensation on the left side below the umbilicus). This classic combination of symptoms is known as **Brown-Séquard syndrome**, which results from a lesion affecting one half of the spinal cord.
- The specific pattern of deficits—motor and proprioceptive loss on the same side as the lesion, and pain/temperature loss on the opposite side—localizes the lesion to the **right half of the spinal cord**.
*Right frontal lobe*
- A lesion in the right frontal lobe would typically cause **contralateral motor weakness** (left-sided) and potentially cognitive or behavioral changes, without the specific sensory dissociation seen in this patient.
- It would not explain the **ipsilateral proprioceptive loss** or the **contralateral pain/temperature loss** at different levels as observed in this case.
*Left frontal lobe*
- A lesion in the left frontal lobe would primarily result in **contralateral motor weakness** (right-sided), similar to the right leg weakness observed, but it would not explain the other sensory deficits, particularly the **contralateral pain/temperature loss** (right-sided in this scenario) and the **ipsilateral proprioceptive loss**.
- **Speech disturbances** (aphasia) are also common with left frontal lobe lesions, depending on the exact location, which are not mentioned here.
*Left hemi-spinal cord*
- A lesion in the left hemi-spinal cord would cause **ipsilateral motor weakness** (left leg weakness) and **ipsilateral dorsal column deficits** (decreased vibration and joint position senses in the left foot and leg), along with **contralateral spinothalamic loss** (decreased pinprick sensation on the right side).
- This pattern is the opposite of the patient's symptoms, which show right-sided weakness and proprioceptive loss, and left-sided pain/temperature loss.
*Right pons*
- A lesion in the pons would typically present with a **combination of cranial nerve deficits** (e.g., facial sensory or motor abnormalities, gaze palsies) **and long tract signs**, often affecting both sides of the body due to the compact nature of the brainstem.
- While it could cause long tract signs, the specific pattern of **dissociated ipsilateral and contralateral sensory/motor deficits** observed below the umbilical level is highly characteristic of a spinal cord lesion and less so of a pontine lesion.
Clinical testing of corticospinal tract function US Medical PG Question 8: A 27-year-old man presents to the emergency department with back pain. The patient states that he has back pain that has been steadily worsening over the past month. He states that his pain is worse in the morning but feels better after he finishes at work for the day. He rates his current pain as a 7/10 and says that he feels short of breath. His temperature is 99.5°F (37.5°C), blood pressure is 130/85 mmHg, pulse is 80/min, respirations are 14/min, and oxygen saturation is 99% on room air. On physical exam, you note a young man who does not appear to be in any distress. Cardiac exam is within normal limits. Pulmonary exam is notable only for a minor decrease in air movement bilaterally at the lung bases. Musculoskeletal exam reveals a decrease in mobility of the back in all four directions. Which of the following is the best initial step in management of this patient?
- A. MRI of the sacroiliac joint (Correct Answer)
- B. CT scan of the chest
- C. Pulmonary function tests
- D. Ultrasound
- E. Radiography of the lumbosacral spine
Clinical testing of corticospinal tract function Explanation: ***MRI of the sacroiliac joint***
- The patient's symptoms of **worsening back pain**, morning stiffness that improves with activity, and decreased back mobility are highly suggestive of **ankylosing spondylitis**.
- **MRI** is the most sensitive imaging modality for detecting early inflammatory changes in the **sacroiliac joints** and spine, which are characteristic of ankylosing spondylitis, even before radiographic changes are visible.
*CT scan of the chest*
- While the patient reports feeling **short of breath**, his vital signs and oxygen saturation are normal, and he does not appear in acute distress.
- A CT scan of the chest would be a more appropriate step if there were clearer signs of acute pulmonary pathology, such as significant hypoxemia, fever, or adventitious lung sounds, which are not present here.
*Pulmonary function tests*
- **Shortness of breath** could eventually be a complication of severe ankylosing spondylitis due to restricted chest wall expansion.
- However, PFTs are generally not the *initial* diagnostic step given the primary presentation of back pain and the need to confirm the underlying rheumatologic condition first.
*Ultrasound*
- **Ultrasound** is not a primary imaging modality for evaluating the sacroiliac joints or the spine in the context of suspected ankylosing spondylitis.
- It could be useful for assessing peripheral joint inflammation in other arthropathies, but not for axial involvement.
*Radiography of the lumbosacral spine*
- **X-rays of the lumbosacral spine** might show changes in advanced ankylosing spondylitis (e.g., squaring of vertebrae, syndesmophytes), but they are often normal in the early stages of the disease.
- **MRI** is superior for detecting early inflammatory changes and is often used to diagnose the condition before radiographic damage is evident.
Clinical testing of corticospinal tract function US Medical PG Question 9: A 23-year-old male presents with complaints of polydipsia and frequent, large-volume urination. Laboratory testing does not demonstrate any evidence of diabetes; however, a reduced urine osmolality of 120 mOsm/L is measured. Which of the following findings on a desmopressin test would be most consistent with a diagnosis of central diabetes insipidus?
- A. Reduction in urine osmolality to 60 mOsm/L following desmopressin administration
- B. No detectable change in urine osmolality following desmopressin administration
- C. Increase in urine osmolality to 400 mOsm/L following desmopressin administration (Correct Answer)
- D. Increase in urine osmolality to 130 mOsm/L following desmopressin administration
- E. Reduction in urine osmolality to 110 mOsm/L following desmopressin administration
Clinical testing of corticospinal tract function Explanation: ***Increase in urine osmolality to 400 mOsm/L following desmopressin administration***
- In **central diabetes insipidus**, the kidneys are still able to respond to **vasopressin** (ADH), but the body doesn't produce enough of it. Therefore, administering **desmopressin** (a synthetic ADH analog) will significantly increase **urine osmolality** as the kidneys resorb more water.
- A significant increase, such as from 120 mOsm/L to 400 mOsm/L, indicates that the underlying problem is a lack of ADH production, characteristic of **central diabetes insipidus**.
*Increase in urine osmolality to 130 mOsm/L following desmopressin administration*
- A minor increase from 120 mOsm/L to 130 mOsm/L following desmopressin administration would suggest that the kidneys are largely **unresponsive** to ADH, which is characteristic of **nephrogenic diabetes insipidus**.
- In central diabetes insipidus, a more substantial increase in **urine osmolality** is expected, as the kidney's ability to respond to ADH is intact.
*Reduction in urine osmolality to 60 mOsm/L following desmopressin administration*
- A reduction in **urine osmolality** after desmopressin administration would be an unexpected and contradictory finding.
- Desmopressin is meant to increase water reabsorption, leading to concentrated urine, not more dilute urine.
*Reduction in urine osmolality to 110 mOsm/L following desmopressin administration*
- Similar to the previous option, a reduction in **urine osmolality** following desmopressin administration is clinically inconsistent with the expected action of ADH.
- This result would not align with either central nor nephrogenic diabetes insipidus scenarios, where an increase or no change, respectively, would be anticipated.
*No detectable change in urine osmolality following desmopressin administration*
- If there is no detectable change or only a very small change in **urine osmolality** after desmopressin administration, it suggests that the kidneys are not responding to ADH.
- This would be consistent with **nephrogenic diabetes insipidus**, where the kidneys themselves are resistant to ADH, rather than central DI, where the problem is ADH deficiency.
Clinical testing of corticospinal tract function US Medical PG Question 10: A father brings his 3-year-old son to the pediatrician because he is concerned about his health. He states that throughout his son's life he has had recurrent infections despite proper treatment and hygiene. Upon reviewing the patient's chart, the pediatrician notices that the child has been infected multiple times with S. aureus, Aspergillus, and E. coli. Which of the following would confirm the most likely cause of this patient's symptoms?
- A. Increased IgM, Decreased IgG, IgA, and IgE
- B. Negative nitroblue-tetrazolium test (Correct Answer)
- C. Positive nitroblue-tetrazolium test
- D. Normal dihydrorhodamine (DHR) flow cytometry test
- E. Increased IgE and IgA, Decreased IgM
Clinical testing of corticospinal tract function Explanation: ***Negative nitroblue-tetrazolium test***
- A **negative nitroblue-tetrazolium (NBT) test** indicates an inability of phagocytes to produce a respiratory burst, which is characteristic of **Chronic Granulomatous Disease (CGD)**.
- CGD patients suffer from recurrent infections with catalase-positive organisms such as *Staphylococcus aureus*, *Aspergillus*, and *E. coli*, consistent with the patient's history.
*Increased IgM, Decreased IgG, IgA, and IgE*
- This pattern of immunoglobulin levels is characteristic of **X-linked hyper-IgM syndrome**, where there is a defect in CD40L on T cells.
- While it also causes recurrent infections, the typical pathogens differ from those stated in the question, often including *Pneumocystis jirovecii*.
*Positive nitroblue-tetrazolium test*
- A **positive NBT test** indicates that phagocytes are capable of producing a respiratory burst and forming superoxide, thus ruling out CGD.
- This result would be expected in a healthy individual or someone with an immunodeficiency not affecting the phagocytic oxidative burst.
*Normal dihydrorhodamine (DHR) flow cytometry test*
- A **normal DHR flow cytometry test** indicates that neutrophils can produce reactive oxygen species (ROS) effectively, meaning the respiratory burst is intact.
- This result would rule out CGD, as CGD patients have an abnormal (decreased) DHR test.
*Increased IgE and IgA, Decreased IgM*
- This specific pattern of immunoglobulin abnormalities is not typically associated with a single, well-defined primary immunodeficiency that would present with the described infections.
- **Hyper-IgE syndrome (Job's syndrome)**, for example, features very high IgE levels but usually a normal IgM.
More Clinical testing of corticospinal tract function US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.