Alternative motor pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alternative motor pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alternative motor pathways US Medical PG Question 1: A 55-year-old woman presents to the physician with repeated episodes of dizziness for the last 3 months, which are triggered by rising from a supine position and by lying down. The episodes are sudden and usually last for less than 30 seconds. During the episode, she feels as if she is suddenly thrown into a rolling spin. She has no symptoms in the period between episodes. The patient denies having headaches, vomiting, deafness, ear discharge or ear pain. There is no history of a known medical disorder or prolonged consumption of a specific drug. The vital signs are within normal limits. On physical examination, when the physician asks the woman to turn her head 45° to the right, and then to rapidly move from the sitting to the supine position, self-limited rotatory nystagmus is observed following her return to the sitting position. The rest of the neurological examination is normal. Which of the following is the treatment of choice for the condition of this patient?
- A. Oral prednisolone for 2 weeks and follow-up
- B. Singular neurectomy
- C. Posterior canal occlusion
- D. Canalith repositioning (Correct Answer)
- E. Oral meclizine for 6 weeks and follow-up
Alternative motor pathways Explanation: ***Canalith repositioning***
- The patient's symptoms (short-lasting, positional dizziness, rolling spin sensation, absence of other neurological symptoms, and positive **Dix-Hallpike maneuver** with **rotatory nystagmus**) are characteristic of **Benign Paroxysmal Positional Vertigo (BPPV)**.
- **Canalith repositioning maneuvers** (e.g., Epley maneuver) are the treatment of choice as they aim to move dislodged otoconia out of the semicircular canals.
*Oral prednisolone for 2 weeks and follow-up*
- **Prednisolone** is a corticosteroid used for inflammatory conditions, but it is **not indicated for BPPV**, which is a mechanical problem.
- While corticosteroids might be used in other vestibular disorders like Meniere's disease or vestibular neuritis, they would not address the underlying cause of BPPV.
*Singular neurectomy*
- **Singular neurectomy** is a surgical procedure that involves cutting the singular nerve (posterior ampullary nerve).
- This is a highly invasive treatment reserved for **intractable BPPV** that has failed multiple conservative treatments, and it carries risks such as hearing loss.
*Posterior canal occlusion*
- **Posterior canal occlusion** is a surgical procedure that involves plugging the posterior semicircular canal.
- This is a surgical option for **severe, refractory BPPV** that has not responded to canalith repositioning maneuvers, and it is more invasive than repositioning.
*Oral meclizine for 6 weeks and follow-up*
- **Meclizine** is an antihistamine used to relieve symptoms of nausea, vomiting, and dizziness associated with vertigo.
- While it can help alleviate symptoms, it does **not treat the underlying cause of BPPV** and is typically used for symptomatic relief, not as a definitive treatment.
Alternative motor pathways US Medical PG Question 2: A 71-year-old man presents to his primary care physician because he is increasingly troubled by a tremor in his hands. He says that the tremor is worse when he is resting and gets better when he reaches for objects. His wife reports that he has been slowing in his movements and also has difficulty starting to walk. His steps have been short and unsteady even when he is able to initiate movement. Physical exam reveals rigidity in his muscles when tested for active range of motion. Histology in this patient would most likely reveal which of the following findings?
- A. Intracellular hyperphosphorylated tau
- B. Large intracellular vacuoles
- C. Amyloid beta plaques
- D. Perivascular inflammation
- E. Alpha-synuclein (Correct Answer)
Alternative motor pathways Explanation: ***Alpha-synuclein***
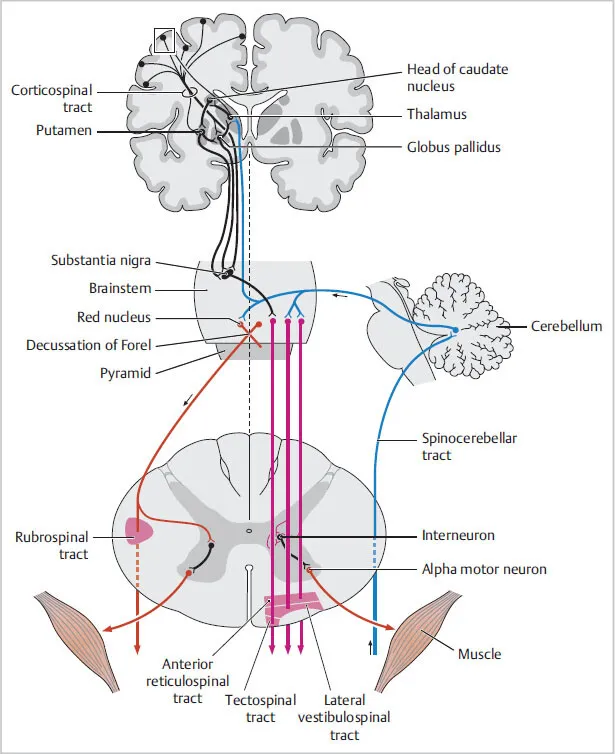
- The patient's symptoms of a **resting tremor** that improves with action, **bradykinesia** (slowed movements, difficulty initiating walking, short steps), and **rigidity** are classic for **Parkinson's disease**.
- Histologically, Parkinson's disease is characterized by the presence of **Lewy bodies**, which are intracellular inclusions comprised primarily of aggregated **alpha-synuclein** protein, particularly in the substantia nigra.
*Intracellular hyperphosphorylated tau*
- **Hyperphosphorylated tau protein** forms **neurofibrillary tangles** and is characteristic of **Alzheimer's disease** and other tauopathies (e.g., frontotemporal dementia), which typically present with cognitive decline rather than primarily motor symptoms as seen here.
- While Parkinson's disease can have co-existing tau pathology, it is not the primary histological hallmark for the motor symptoms described.
*Large intracellular vacuoles*
- The presence of **large intracellular vacuoles** within neurons is characteristic of **spongiform encephalopathies** (e.g., Creutzfeldt-Jakob disease), which present with rapidly progressive dementia, myoclonus, and ataxia.
- This finding is not associated with the classic motor symptoms of Parkinson's disease.
*Amyloid beta plaques*
- **Amyloid beta plaques** (extracellular deposits of amyloid-beta protein) are a hallmark of **Alzheimer's disease**, which primarily manifests with progressive cognitive impairment and memory loss.
- These plaques are not the primary histological feature of Parkinson's disease.
*Perivascular inflammation*
- **Perivascular inflammation** is typically seen in **inflammatory or demyelinating diseases** of the central nervous system, such as **multiple sclerosis** or **encephalitis**.
- This finding is not characteristic of neurodegenerative disorders like Parkinson's disease, which are instead marked by protein aggregation and neuronal loss.
Alternative motor pathways US Medical PG Question 3: A 73-year-old man presents to your office accompanied by his wife. He has been experiencing a tremor in his right hand for the last several months that seems to be worsening. He does not have any other complaints and says he’s “fine.” His wife thinks that he has also had more difficulty walking. His history is significant for hypertension and an ischemic stroke of the right middle cerebral artery 2 years ago. His medications include hydrochlorothiazide and daily aspirin. On physical exam you note that the patient speaks with a soft voice and has decreased facial expressions. He has a resting tremor that is worse on the right side. He has increased resistance to passive movement when you flex and extend his relaxed wrist. He has 5/5 strength bilaterally. Neuronal degeneration in which of the following locations is most likely responsible for the progression of this disease?
- A. Vermis
- B. Substantia nigra pars compacta (Correct Answer)
- C. Frontotemporal lobe
- D. Caudate and putamen
- E. Subthalamic nucleus
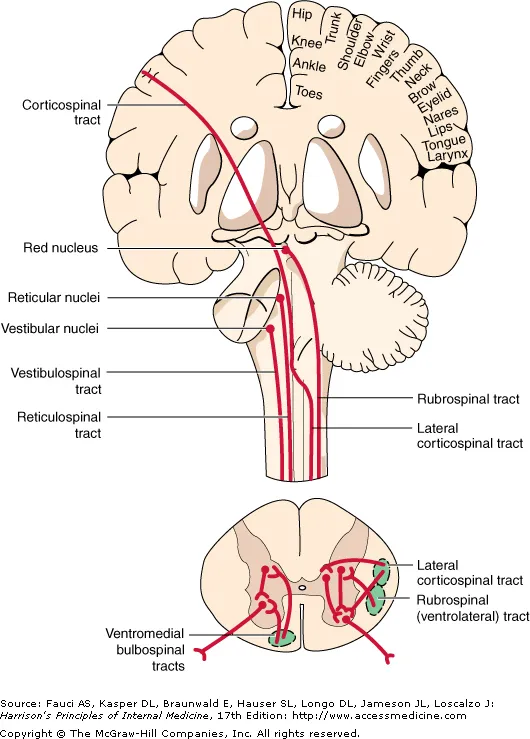
Alternative motor pathways Explanation: ***Substantia nigra pars compacta***
- The patient's symptoms, including **resting tremor**, **bradykinesia** (soft voice, decreased facial expressions, difficulty walking), and **rigidity** (increased resistance to passive movement), are classic signs of **Parkinson's disease**.
- Parkinson's disease is primarily caused by the degeneration of **dopaminergic neurons** in the **substantia nigra pars compacta**, leading to a lack of dopamine in the basal ganglia.
*Vermis*
- The **vermis** is a part of the cerebellum primarily involved in coordinating **truncal movements** and maintaining **posture**.
- Damage to the vermis typically causes **ataxia**, truncal instability, and gait disturbances, which are not the primary features described here.
*Frontotemporal lobe*
- The **frontotemporal lobe** is associated with cognitive functions, personality, and language.
- Degeneration in this area is characteristic of **frontotemporal dementia**, presenting with prominent behavioral changes, language difficulties, or progressive memory loss, which are not the main symptoms in this patient.
*Caudate and putamen*
- The **caudate and putamen** are components of the **striatum**, which receives dopaminergic input from the substantia nigra.
- While the lack of dopamine in the striatum contributes to Parkinsonian symptoms, the primary neuronal degeneration occurs *before* this in the substantia nigra pars compacta, which *projects* to the striatum.
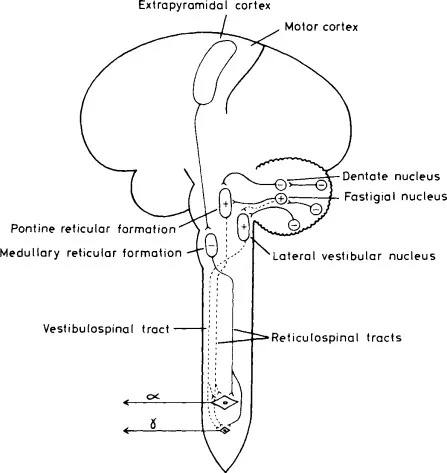
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia circuit, and its overactivity can contribute to motor symptoms in Parkinson's disease.
- **Deep brain stimulation (DBS)** targeting the subthalamic nucleus is a treatment for Parkinson's, but the primary site of neuronal degeneration in the disease itself is not the subthalamic nucleus.
Alternative motor pathways US Medical PG Question 4: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
Alternative motor pathways Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Alternative motor pathways US Medical PG Question 5: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Alternative motor pathways Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
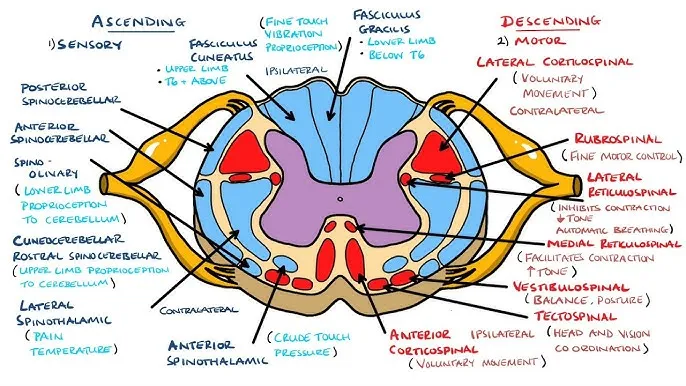
Alternative motor pathways US Medical PG Question 6: A 21-year-old man was involved in a motor vehicle accident and died. At autopsy, the patient demonstrated abnormally increased mobility at the neck. A section of cervical spinal cord at C6 was removed and processed into slides. Which of the following gross anatomic features is most likely true of this spinal cord level?
- A. Cuneate and gracilis fasciculi are present (Correct Answer)
- B. Least amount of white matter
- C. Prominent lateral horns
- D. Absence of gray matter enlargement
- E. Involvement with parasympathetic nervous system
Alternative motor pathways Explanation: **Cuneate and gracilis fasciculi are present**
- At the **C6 level** of the spinal cord, both the **fasciculus gracilis** (carrying information from the lower body) and the **fasciculus cuneatus** (carrying information from the upper body) are present in the dorsal column.
- The fasciculus cuneatus typically appears at **T6 and above**, making it visible at C6.
*Least amount of white matter*
- The cervical spinal cord, particularly at C6, contains a **significant amount of white matter** because it carries all ascending and descending tracts to and from the brain, including those for the upper and lower limbs.
- The **sacral segments** typically have the least amount of white matter due to fewer tracts remaining.
*Prominent lateral horns*
- **Lateral horns** are characteristic of the **thoracic and upper lumbar (T1-L2/L3)** spinal cord segments, where they house preganglionic sympathetic neurons.
- They are generally **absent or poorly developed** in the cervical spinal cord.
*Absence of gray matter enlargement*
- The **cervical enlargement** of the spinal cord, particularly pronounced from C4 to T1, contains an increased amount of gray matter to accommodate the innervation of the **upper limbs**.
- Therefore, the C6 level would show **significant gray matter enlargement**.
*Involvement with parasympathetic nervous system*
- The **parasympathetic nervous system** exits the spinal cord at the **sacral levels (S2-S4)** and as cranial nerves, not primarily from the cervical spinal cord through distinct horns.
- The cervical spinal cord is primarily associated with **somatic motor and sensory pathways** for the neck, shoulders, and upper limbs, and receives some sympathetic input, but is not where parasympathetic outflow predominantly originates.
Alternative motor pathways US Medical PG Question 7: A 27-year-old man presents to a physician for evaluation of 3 months of increased vertigo. He says that occasionally he will experience several seconds of intense vertigo that makes him lose his balance. He came in for evaluation because this symptom is affecting his ability to drive to work. He has also been occasionally experiencing tinnitus. Physical exam reveals rotatory nystagmus that is delayed in onset and stops with visual fixation. The nerve that is most likely causing these symptoms exits the skull at which of the following locations?
- A. Internal auditory meatus (Correct Answer)
- B. Cribriform plate
- C. Foramen ovale
- D. Jugular foramen
- E. Foramen rotundum
Alternative motor pathways Explanation: ***Internal auditory meatus***
- The symptoms described, particularly **vertigo** and **tinnitus**, are indicative of an issue with the **vestibulocochlear nerve (CN VIII)**.
- The **vestibulocochlear nerve** exits the skull through the **internal auditory meatus**, which is also the pathway for the **facial nerve (CN VII)**.
*Cribriform plate*
- The **cribriform plate** is associated with the passage of the **olfactory nerves (CN I)**, which are responsible for the sense of smell.
- Damage to this area would typically cause **anosmia**, not vertigo or tinnitus.
*Foramen ovale*
- The **foramen ovale** is the exit point for the **mandibular nerve (V3)**, a branch of the trigeminal nerve.
- Dysfunction here would lead to problems with **mastication** or altered sensation in the lower face, not vertigo.
*Jugular foramen*
- The **jugular foramen** transmits several cranial nerves: the **glossopharyngeal (CN IX)**, **vagus (CN X)**, and **accessory (CN XI)** nerves.
- Issues in this region would manifest as difficulties with **swallowing**, **speech**, or **shoulder/neck movement**, not balance or hearing.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, another branch of the trigeminal nerve.
- Damage to this nerve would primarily affect **sensation in the middle third of the face**, not balance or hearing.
Alternative motor pathways US Medical PG Question 8: A 27-year-old man is brought to the emergency department because of a knife wound to his back. His pulse is 110/min, respirations are 14/min, and blood pressure is 125/78 mm Hg. Examination shows a 5-cm deep stab wound at the level of T9. He withdraws the right foot to pain but is unable to sense vibration or whether his right toe is flexed or extended. Sensation in the left leg is normal. Motor strength is 5/5 in all extremities. Rectal tone is normal. Which of the following spinal column structures was most likely affected?
- A. Central spinal cord grey matter
- B. Lateral corticospinal tract
- C. Dorsal root (Correct Answer)
- D. Artery of Adamkiewicz
- E. Posterior spinal artery
Alternative motor pathways Explanation: ***Dorsal root***
- The patient's inability to sense **vibration** or **proprioception** (flexed/extended toe) on the right side, with intact motor strength, strongly implicates damage to the **dorsal columns** or the **dorsal root** carrying these afferent fibers.
- The dorsal root transmits **sensory** (afferent) information from the periphery to the spinal cord, and injury would selectively impair these specific sensory modalities without affecting motor function.
*Central spinal cord grey matter*
- Damage to the central gray matter, as seen in conditions like **syringomyelia**, typically affects the **spinothalamic tracts** first, leading to a "cape-like" distribution of bilateral loss of **pain** and **temperature sensation**.
- It would not primarily cause isolated **proprioceptive** or **vibration** loss with preserved motor function.
*Lateral corticospinal tract*
- Injury to the **lateral corticospinal tract** results in **motor deficits**, specifically **weakness** or paralysis, usually on the same side or contralateral depending on the location of the lesion (above or below decussation).
- The patient exhibits normal motor strength (5/5), indicating this tract is likely intact.
*Artery of Adamkiewicz*
- Occlusion or injury to the **Artery of Adamkiewicz** typically causes **anterior spinal artery syndrome**, affecting the **anterior two-thirds of the spinal cord**.
- This leads to bilateral loss of **motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts), with preservation of dorsal column functions (vibration, proprioception).
*Posterior spinal artery*
- The **posterior spinal arteries** supply the **dorsal columns**, and their occlusion would lead to bilateral loss of **vibration** and **proprioception**.
- However, the patient's symptoms are **unilateral** on the right side, suggesting a more localized injury to the dorsal root or dorsal column on that side rather than a bilateral vascular event.
Alternative motor pathways US Medical PG Question 9: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Alternative motor pathways Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
Alternative motor pathways US Medical PG Question 10: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Alternative motor pathways Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
More Alternative motor pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.