Vital centers in brainstem US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vital centers in brainstem. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vital centers in brainstem US Medical PG Question 1: An otherwise healthy 58-year-old man comes to the physician because of a 1-year history of episodic coughing whenever he cleans his left ear. There is no history of hearing loss, tinnitus, or vertigo. Stimulating his left ear canal with a cotton swab triggers a bout of coughing. The physician informs him that these symptoms are caused by hypersensitivity of a cranial nerve. A peripheral lesion of this nerve is most likely to manifest with which of the following findings on physical examination?
- A. Ipsilateral sensorineural hearing loss
- B. Ipsilateral deviation of the tongue
- C. Inability to raise ipsilateral eyebrow
- D. Decreased secretion from ipsilateral sublingual gland
- E. Ipsilateral vocal cord palsy (Correct Answer)
Vital centers in brainstem Explanation: ***Ipsilateral vocal cord palsy***
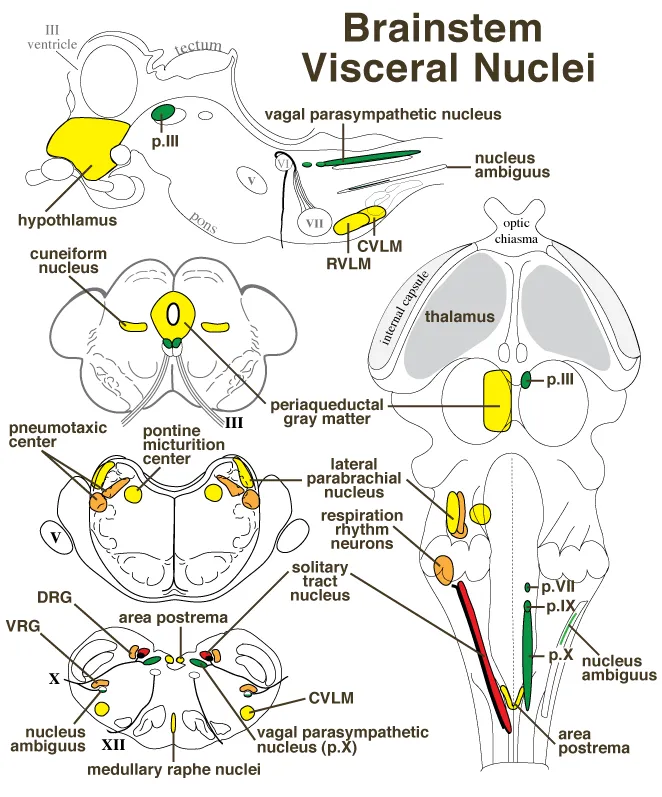
- The sensation in the external auditory canal that triggers a cough reflex is mediated by the **auricular branch of the vagus nerve (CN X)**, also known as Arnold's nerve.
- A peripheral lesion of the vagus nerve would most likely affect its motor functions, including the innervation of the **larynx**, leading to **ipsilateral vocal cord palsy** and hoarseness.
*Ipsilateral sensorineural hearing loss*
- Hearing loss is primarily associated with pathology of the **vestibulocochlear nerve (CN VIII)**, not the vagus nerve.
- The patient's presentation does not describe any auditory symptoms.
*Ipsilateral deviation of the tongue*
- Tongue deviation is a sign of compromise of the **hypoglossal nerve (CN XII)**, which controls the intrinsic and extrinsic muscles of the tongue.
- This is not a function of the vagus nerve.
*Inability to raise ipsilateral eyebrow*
- The ability to raise the eyebrow is controlled by the **facial nerve (CN VII)**, which innervates the muscles of facial expression.
- Vagus nerve lesions do not typically present with facial weakness.
*Decreased secretion from ipsilateral sublingual gland*
- Secretion from the sublingual gland is controlled by the **facial nerve (CN VII)** via the submandibular ganglion.
- While the vagus nerve has autonomic functions, it does not directly control sublingual gland secretion.
Vital centers in brainstem US Medical PG Question 2: Which of the following physiologic changes decreases pulmonary vascular resistance (PVR)?
- A. Inhaling the inspiratory reserve volume (IRV)
- B. Exhaling the entire vital capacity (VC)
- C. Exhaling the expiratory reserve volume (ERV)
- D. Breath holding maneuver at functional residual capacity (FRC)
- E. Inhaling the entire vital capacity (VC) (Correct Answer)
Vital centers in brainstem Explanation: ***Inhaling the entire vital capacity (VC)***
- As lung volume increases from FRC to TLC (which includes inhaling the entire VC), alveolar vessels are **stretched open**, and extra-alveolar vessels are **pulled open** by the increased radial traction, leading to a decrease in PVR.
- This **maximizes the cross-sectional area** of the pulmonary vascular bed, lowering resistance.
*Inhaling the inspiratory reserve volume (IRV)*
- While inhaling IRV increases lung volume, it's not the maximal inspiration of the entire VC where **PVR is typically at its lowest**.
- PVR continues to decrease as lung volume approaches total lung capacity (TLC).
*Exhaling the entire vital capacity (VC)*
- Exhaling the entire vital capacity leads to very low lung volumes, where PVR significantly **increases**.
- At low lung volumes, **alveolar vessels become compressed** and extra-alveolar vessels **narrow**, increasing resistance.
*Exhaling the expiratory reserve volume (ERV)*
- Exhaling the ERV results in a lung volume below FRC, which causes a **marked increase in PVR**.
- This is due to the **compression of alveolar vessels** and decreased radial traction on extra-alveolar vessels.
*Breath holding maneuver at functional residual capacity (FRC)*
- At FRC, the PVR is at an **intermediate level**, not its lowest.
- This is the point where the opposing forces affecting alveolar and extra-alveolar vessels are somewhat balanced, but not optimized for minimal resistance.
Vital centers in brainstem US Medical PG Question 3: A 66-year-old man is brought to the emergency department because of shortness of breath and confusion. His pulse is 98/min, and blood pressure is 109/73 mm Hg. He is oriented to person but not time or place. A graph of his breathing pattern and oxygen saturation is shown. Which of the following additional findings is most likely present in this patient?
- A. Rib fracture
- B. Fruity breath odor
- C. Ventricular gallop (Correct Answer)
- D. Miotic pupils
- E. Barrel chest
Vital centers in brainstem Explanation: ***Ventricular gallop***
- The patient's presentation with **shortness of breath**, **confusion**, and **oxygen desaturation** coupled with the breathing pattern shown (likely Cheyne-Stokes respiration from the image) strongly suggests **heart failure**. A **ventricular gallop (S3 heart sound)** is a classic finding in heart failure, indicating rapid ventricular filling into a stiff or dilated ventricle.
- The **confusional state** and **tachypnea (implied by oxygen desaturation)** are consistent with **hypoxia** and **reduced cardiac output** often seen in decompensated heart failure, where an S3 gallop is frequently heard.
*Rib fracture*
- While a rib fracture can cause shortness of breath due to pain and reduced chest expansion, it would not typically lead to **confusion** or a specific cyclical breathing pattern like Cheyne-Stokes, nor would it directly cause a ventricular gallop.
- The patient's vital signs and mental status point towards a more systemic issue rather than isolated chest trauma.
*Fruity breath odor*
- A **fruity breath odor** is a hallmark of **diabetic ketoacidosis (DKA)**, caused by the exhalation of acetone. This condition would also present with confusion and tachypnea, but would typically involve hyperglycemia and metabolic acidosis.
- There is no information to suggest diabetes, and the presentation of a specific breathing pattern in correlation with cardiac findings makes heart failure more likely.
*Miotic pupils*
- **Miotic pupils (pinpoint pupils)** are strongly associated with **opioid overdose** or organophosphate poisoning. These conditions would cause respiratory depression, not necessarily the specific breathing pattern, and would not explain the other findings in this specific context.
- The patient's pulse and blood pressure are also not typical of severe opioid overdose, which often involves bradycardia and hypotension.
*Barrel chest*
- A **barrel chest** is a physical finding typically associated with **chronic obstructive pulmonary disease (COPD)** due to chronic air trapping. While COPD can cause shortness of breath and confusion (in acute exacerbations), it does not directly lead to a ventricular gallop.
- Although the patient's age makes COPD possible, the acute presentation with a specific breathing pattern and the likelihood of heart failure make a barrel chest a less specific or primary finding in this context.
Vital centers in brainstem US Medical PG Question 4: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Vital centers in brainstem Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Vital centers in brainstem US Medical PG Question 5: A researcher is studying receptors that respond to epinephrine in the body and discovers a particular subset that is expressed in presynaptic adrenergic nerve terminals. She discovers that upon activation, these receptors will lead to decreased sympathetic nervous system activity. She then studies the intracellular second messenger changes that occur when this receptor is activated. She records these changes and begins searching for analogous receptor pathways. Which of the following receptors would cause the most similar set of intracellular second messenger changes?
- A. Muscarinic cholinoreceptors in the gastrointestinal tract
- B. Growth hormone receptors in the musculoskeletal system
- C. Vasopressin receptors in the kidney
- D. Dopamine receptors in the brain (Correct Answer)
- E. Aldosterone receptors in the kidney
Vital centers in brainstem Explanation: ***Dopamine receptors in the brain***
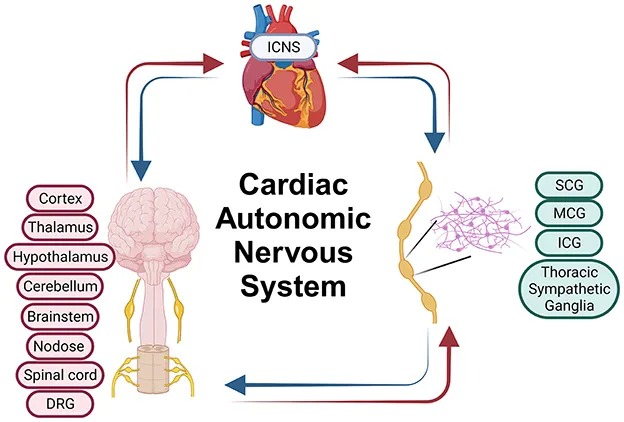
- The described presynaptic receptors for epinephrine that decrease sympathetic activity are **alpha-2 adrenergic receptors**, which are **G inhibitory protein (Gi)-coupled receptors**.
- Gi-coupled receptors **inhibit adenylyl cyclase**, leading to a **decrease in intracellular cAMP**, a signaling pathway shared by **D2 dopamine receptors**.
*Muscarinic cholinoreceptors in the gastrointestinal tract*
- Most muscarinic receptors (M1 and M3) in the GI tract are **Gq-coupled**, leading to an **increase in phospholipase C (PLC) activity**, ultimately increasing intracellular **IP3 and DAG** and promoting smooth muscle contraction.
- This mechanism is distinct from the **Gi-mediated inhibition of cAMP** described for the presynaptic adrenergic receptor.
*Growth hormone receptors in the musculoskeletal system*
- Growth hormone receptors are **tyrosine kinase-associated receptors** (specifically, they are linked to **JAK/STAT pathways**), not G protein-coupled receptors.
- Their intracellular signaling involves **protein phosphorylation cascades**, which are fundamentally different from second messenger changes involving cAMP.
*Vasopressin receptors in the kidney*
- Vasopressin (ADH) acts on **V2 receptors** in the kidney, which are **G stimulatory protein (Gs)-coupled receptors**.
- Activation of V2 receptors leads to an **increase in adenylyl cyclase activity** and thus an **increase in intracellular cAMP**, the opposite effect of the described Gi-coupled receptor.
*Aldosterone receptors in the kidney*
- Aldosterone receptors are **intracellular steroid hormone receptors** that directly bind to DNA and regulate gene transcription.
- They do not engage in rapid intracellular second messenger changes like G protein-coupled receptors, but rather alter **protein synthesis** over hours to days.
Vital centers in brainstem US Medical PG Question 6: A 55-year-old man presents with an unremitting cough and swelling of the lower limbs for the past 2 weeks. He says he has had a chronic cough for years, however, he feels it is getting worse. He reports a 30-pack-year smoking history. Physical examination reveals mild central cyanosis and expiratory wheezes throughout the chest. Oxygen therapy is ordered immediately but, soon after administering it, his respiratory rate starts to slow down and he becomes drowsy. Dysfunction of which of the following receptors most likely led to this patient’s current condition?
- A. Pleural pain receptors
- B. Central chemoreceptors
- C. Airway stretch receptors
- D. Pulmonary stretch receptors
- E. Peripheral chemoreceptors (Correct Answer)
Vital centers in brainstem Explanation: ***Peripheral chemoreceptors***
- In patients with chronic obstructive pulmonary disease (COPD) like this patient, the **central chemoreceptors** become desensitized to chronically elevated CO2 levels. Their primary respiratory drive then shifts to the **peripheral chemoreceptors** (carotid and aortic bodies), which are sensitive to **hypoxia**.
- Administering high-flow oxygen **eliminates the hypoxic stimulus** sensed by these normally functioning peripheral chemoreceptors, removing the hypoxic drive to breathe and leading to **hypoventilation, CO2 retention, respiratory acidosis**, and drowsiness (CO2 narcosis).
*Pleural pain receptors*
- These receptors are primarily involved in sensing pain associated with **pleural inflammation** or injury, contributing to the sensation of pain with breathing.
- They do not play a role in regulating the primary ventilatory drive in response to blood gas changes.
*Central chemoreceptors*
- These receptors are located in the **medulla** and are primarily sensitive to changes in **arterial PCO2** and pH (via H+ ions in CSF).
- In chronic respiratory diseases with CO2 retention, they become **desensitized** to elevated CO2, shifting the main respiratory drive to the peripheral chemoreceptors' response to hypoxia.
*Airway stretch receptors*
- These receptors, including **slowly adapting stretch receptors** and **rapidly adapting irritant receptors**, are located in the airways and respond to lung inflation and irritants.
- They are involved in the Hering-Breuer reflex and cough reflex but are not the primary drivers of ventilation in response to hypoxemia.
*Pulmonary stretch receptors*
- These receptors are located in the **bronchial smooth muscle** and respond to lung distension, contributing to the **Hering-Breuer reflex** which inhibits inspiration to prevent overinflation.
- While important for lung mechanics, they do not directly sense blood gas levels to drive ventilation in the context of hypoxia or hypercapnia.
Vital centers in brainstem US Medical PG Question 7: A 65-year-old female with a past medical history of hypertension presents to her primary care doctor with a 3 month history of spasmodic facial pain. The pain is located in her right cheek and seems to be triggered when she smiles, chews, or brushes her teeth. The pain is sharp and excruciating, lasts for a few seconds, and occurs up to twenty times per day. She denies headaches, blurry vision, facial weakness, or changes in her memory. She feels rather debilitated and has modified much of her daily activities to avoid triggering the spasms. In the clinic, her physical exam is within normal limits. Her primary care doctor prescribes carbamazepine and asks her to follow up in a few weeks. Which cranial nerve is most likely involved in the patient's disease process?
- A. CN III
- B. CN V (Correct Answer)
- C. CN VI
- D. CN VII
- E. CN IV
Vital centers in brainstem Explanation: ***CN V***
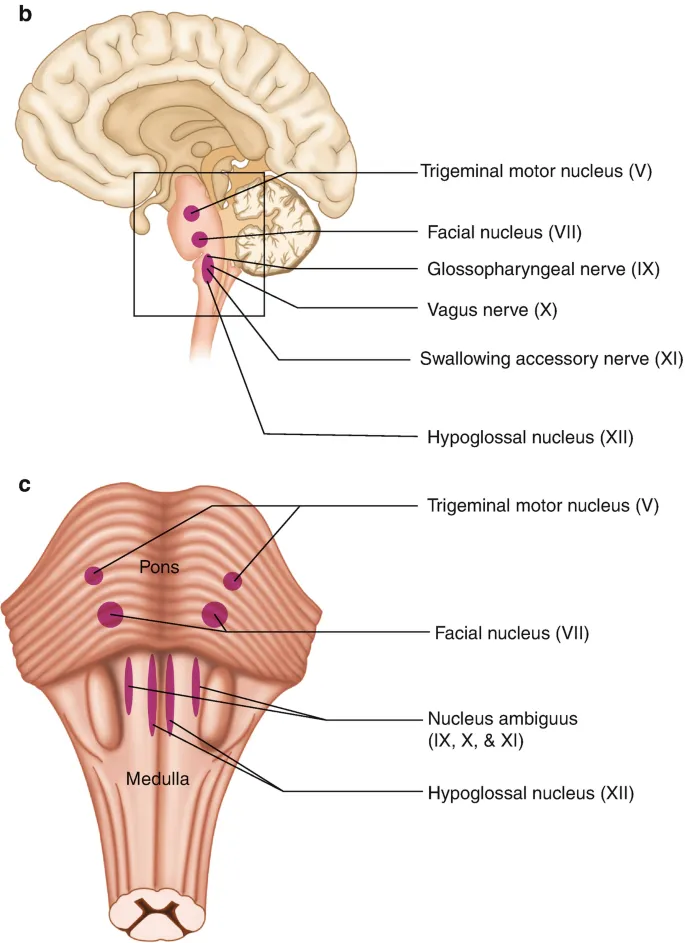
- The patient's presentation of **recurrent, sharp, excruciating, unilateral facial pain** triggered by movements like chewing, smiling, or brushing teeth is classic for **trigeminal neuralgia**.
- **Trigeminal neuralgia** specifically affects the **trigeminal nerve (CN V)**, which has sensory branches covering the face, and is often treated with **carbamazepine**.
*CN III*
- The **oculomotor nerve (CN III)** is primarily involved in **eye movement** and **pupillary constriction**.
- Damage to CN III typically causes **diplopia, ptosis,** and **pupil dilation**, which are not present in this patient's symptoms.
*CN VI*
- The **abducens nerve (CN VI)** controls the **lateral rectus muscle**, responsible for **abducting the eye** (moving it outward).
- Dysfunction typically results in **diplopia** and an inability to move the eye laterally, not facial pain.
*CN VII*
- The **facial nerve (CN VII)** controls **facial expressions**, taste sensation from the anterior two-thirds of the tongue, and lacrimation/salivation.
- While it innervates facial muscles, its involvement typically presents as **facial weakness** or **paralysis** (e.g., Bell's palsy), not sharp, spasmodic pain.
*CN IV*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which is involved in rotating and depressing the eye.
- Lesions usually lead to **vertical diplopia**, particularly when looking down and inward, which is unrelated to the described facial pain.
Vital centers in brainstem US Medical PG Question 8: A 22-year-old man presents with a history of lightheadedness, weakness, and palpitations when he assumes an upright position from a supine position. He is otherwise a healthy man without a history of alcohol or other substance abuse. His supine and standing blood pressures (measured at 3-minute intervals) were 124/82 mm Hg and 102/72 mm Hg, respectively. He was advised to perform a Valsalva maneuver while monitoring blood pressure and heart rate to assess the integrity of his baroreflex control. Which of the following statements is correct?
- A. During early phase II, there is an increase in blood pressure and a decrease in heart rate
- B. Phases III and IV are mediated by baroreceptor reflexes that require intact efferent parasympathetic responses
- C. During phase I, the blood pressure decreases due to increased intrathoracic pressure
- D. During late phase II, there is an increase in both blood pressure and heart rate (Correct Answer)
- E. The Valsalva ratio is defined as the maximum phase II tachycardia divided by the minimum phase IV bradycardia
Vital centers in brainstem Explanation: ***During late phase II, there is an increase in both blood pressure and heart rate***
- In **late phase II** of the Valsalva maneuver, the sustained intrathoracic pressure reduces venous return, leading to a compensatory **increase in heart rate** and **peripheral vasoconstriction** via baroreflex stimulation, which aims to normalize cardiac output and blood pressure.
- While cardiac output remains low, the increased peripheral resistance causes the **blood pressure to rise** back towards baseline, or even slightly above, as the body struggles to maintain perfusion.
*The Valsalva ratio is defined as the maximum phase II tachycardia divided by the minimum phase IV bradycardia*
- The **Valsalva ratio** is defined as the maximum R-R interval during phase IV (bradycardia) divided by the minimum R-R interval during phase II (tachycardia) of the maneuver.
- This ratio primarily assesses **parasympathetic function** and is used to evaluate autonomic neuropathy.
- The option incorrectly reverses the physiological responses: phase II is characterized by **tachycardia** (not bradycardia) and phase IV by **bradycardia** (not tachycardia).
*During early phase II, there is an increase in blood pressure and a decrease in heart rate*
- In **early phase II**, the sustained intrathoracic pressure significantly **reduces venous return** and subsequently **cardiac output**, which leads to a noticeable **drop in blood pressure**.
- This drop in blood pressure activates the baroreflex, causing a compensatory **increase in heart rate**, not a decrease.
*Phases III and IV are mediated by baroreceptor reflexes that require intact efferent parasympathetic responses*
- **Phase III** is primarily a mechanical event where release of intrathoracic pressure causes an immediate drop in blood pressure as the aorta re-expands; this does not specifically require parasympathetic responses.
- **Phase IV** involves baroreceptor-mediated **parasympathetic activation** causing reflex bradycardia as blood pressure overshoots baseline due to increased venous return combined with persistent vasoconstriction.
- The statement is imprecise as it applies primarily to phase IV, not phase III.
*During phase I, the blood pressure decreases due to increased intrathoracic pressure*
- **Phase I** begins with the onset of straining and **increased intrathoracic pressure**, which briefly **compresses the aorta** and large arteries, causing a **transient increase in blood pressure**.
- This initial rise in pressure is due to mechanical compression, not a decrease.
Vital centers in brainstem US Medical PG Question 9: A 28-year-old woman is brought to the emergency department 1 hour after being involved in a motor vehicle collision. She was riding a bike when she lost control and hit a car on the opposite side of the road. On arrival, she is unconscious. She has a history of intravenous heroin use. Her pulse is 56/min, respirations are 8/min and irregular, and blood pressure is 196/102 mm Hg. Examination shows a 2-cm laceration over the left cheek and a 3-cm laceration over the left chest. There are multiple abrasions over her face and chest. She opens her eyes and flexes her extremities to painful stimuli. The pupils are dilated and react sluggishly to light. There are decreased breath sounds over the left lung. The trachea is central. There is no jugular venous distention. Cardiac examination shows no abnormalities. The abdomen is soft and nontender. The left knee and right ankle are swollen; range of motion is limited. Two large-bore peripheral intravenous catheters are inserted. She is intubated and mechanical ventilation is initiated. A focused assessment with sonography in trauma is negative. An occlusive dressing is applied over the left chest wound. She is scheduled for a noncontrast CT scan of the brain. Which of the following is the underlying cause of this patient's hypertension?
- A. Elevated sympathetic response
- B. Increased intrathoracic pressure
- C. Reduced parasympathetic response
- D. Posttraumatic vasospasm
- E. Brainstem compression (Correct Answer)
Vital centers in brainstem Explanation: ***Brainstem compression***
- The patient's presentation with **hypertension**, **bradycardia**, and **irregular respirations** (Cushing's triad) in the setting of severe head trauma is highly indicative of **increased intracranial pressure (ICP)** leading to brainstem compression.
- Brainstem compression, often due to a mass effect from hemorrhage or edema, impairs the brainstem's ability to regulate vital functions, resulting in this classic triad.
*Elevated sympathetic response*
- While trauma typically triggers an **elevated sympathetic response** leading to tachycardia and hypertension, the presence of **bradycardia** in this patient makes a purely sympathetic surge less likely to be the underlying cause of her hypertension.
- The elevated blood pressure combined with a low heart rate points away from an unopposed sympathetic activation.
*Increased intrathoracic pressure*
- An increase in intrathoracic pressure, as seen in conditions like **tension pneumothorax**, can impair venous return and cardiac output, typically leading to **hypotension**, not hypertension.
- Although the patient has decreased breath sounds on the left, an occlusive dressing was applied, and a FAST exam was negative for significant fluid, making this less likely the cause of hypertension.
*Reduced parasympathetic response*
- A reduced parasympathetic response would generally lead to **tachycardia** rather than bradycardia, as the vagal tone would be diminished.
- The observed bradycardia, therefore, contradicts a primary issue of reduced parasympathetic activity.
*Posttraumatic vasospasm*
- **Posttraumatic vasospasm** can occur after severe brain injury, but it typically does not directly manifest as immediate, severe hypertension accompanied by bradycardia and respiratory irregularities (Cushing's triad).
- Vasospasm usually contributes to cerebral ischemia and can develop hours to days after the initial injury, not typically as the acute cause of these profound vital sign changes.
Vital centers in brainstem US Medical PG Question 10: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Vital centers in brainstem Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
More Vital centers in brainstem US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.