Reticular formation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Reticular formation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Reticular formation US Medical PG Question 1: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Reticular formation Explanation: ***Pressure***
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Reticular formation US Medical PG Question 2: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Reticular formation Explanation: ***Muscarinic (M1)***
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Reticular formation US Medical PG Question 3: A 54-year-old man is brought to the emergency department 30 minutes after being hit by a car while crossing the street. He had a left-sided tonic-clonic seizure and one episode of vomiting while being transported to the hospital. On arrival, he is not oriented to person, place, or time. Physical examination shows flaccid paralysis of all extremities. A CT scan of the head is shown. This patient's symptoms are most likely the result of a hemorrhage in which of the following structures?
- A. Between the dura mater and the arachnoid mater
- B. Into the cerebral parenchyma
- C. Between the skull and the dura mater
- D. Between the arachnoid mater and the pia mater (Correct Answer)
- E. Into the ventricular system
Reticular formation Explanation: ***Between the arachnoid mater and the pia mater (Correct)***
- The CT scan demonstrates diffuse high-density (white) material within the sulci and basal cisterns, indicative of a **subarachnoid hemorrhage**. This space is located between the arachnoid mater and the pia mater.
- The patient's presentation with altered mental status, seizures, vomiting, and flaccid paralysis following trauma is consistent with the severe neurological impact of a **traumatic subarachnoid hemorrhage**.
*Between the dura mater and the arachnoid mater (Incorrect)*
- Hemorrhage in this location is known as a **subdural hematoma**, which typically appears as a crescent-shaped collection of blood.
- While possible in trauma, the CT image shows blood primarily filling the sulci, not a subdural collection.
*Into the cerebral parenchyma (Incorrect)*
- This would be an **intraparenchymal hemorrhage**, appearing as a focal area of high density within the brain tissue itself.
- Although there might be some associated parenchymal injury in severe trauma, the predominant pattern seen on the CT is diffuse blood in the subarachnoid space.
*Between the skull and the dura mater (Incorrect)*
- This describes an **epidural hematoma**, often characterized by a lenticular (lens-shaped) collection of blood due to its confinement by dural attachments.
- The CT image does not show a lenticular collection of blood in this space.
*Into the ventricular system (Incorrect)*
- **Intraventricular hemorrhage** would show blood filling the cerebral ventricles.
- While subarachnoid hemorrhage can sometimes extend into the ventricles, the primary finding on this CT is diffuse blood in the subarachnoid space, not isolated ventricular blood.
Reticular formation US Medical PG Question 4: A 20-year-old college student presents to the emergency room complaining of insomnia for the past 48 hours. He explains that although his body feels tired, he is "full of energy and focus" after taking a certain drug an hour ago. He now wants to sleep because he is having hallucinations. His vital signs are T 100.0 F, HR 110 bpm, and BP of 150/120 mmHg. The patient states that he was recently diagnosed with "inattentiveness." Which of the following is the mechanism of action of the most likely drug causing the intoxication?
- A. Blocks NMDA receptors
- B. Activates mu opioid receptors
- C. Displaces norepinephrine from secretory vesicles leading to norepinephrine depletion
- D. Binds to cannabinoid receptors
- E. Increases presynaptic dopamine and norepinephrine release from vesicles (Correct Answer)
Reticular formation Explanation: ***Increases presynaptic dopamine and norepinephrine releases from vesicles***
- The patient's presentation with **insomnia**, feeling "full of energy and focus," **hallucinations**, tachycardia (HR 110 bpm), and hypertension (BP 150/120 mmHg) after taking a drug, especially in the context of a recent diagnosis of "inattentiveness," strongly suggests **amphetamine intoxication**. Amphetamines are commonly prescribed for **ADHD**, and their mechanism involves increasing the release of **dopamine** and **norepinephrine** from presynaptic vesicles.
- This increased release of **catecholamines** leads to the stimulant effects observed, including heightened energy, improved focus, and the adverse effects of agitation, psychosis (hallucinations), and sympathetic overdrive.
*Blocks NMDA receptors*
- Drugs that block **NMDA receptors**, such as **phencyclidine (PCP)** or **ketamine**, can cause dissociative and hallucinatory effects.
- However, the patient's primary complaint of feeling "full of energy and focus" in the context of "inattentiveness" points more towards a classical stimulant rather than a dissociative anesthetic.
*Activates mu opioid receptors*
- Activating **mu opioid receptors** (e.g., by heroin, morphine, fentanyl) typically causes central nervous system **depression**, respiratory depression, miosis, and euphoria, not the stimulant and hyperactive state described.
- The patient's symptoms of increased energy, focus, and elevated vital signs are the opposite of opioid effects.
*Displaces norepinephrine from secretory vesicles leading to norepinephrine depletion*
- This mechanism is characteristic of drugs like **reserpine**, which deplete catecholamines and lead to sedative or antihypertensive effects, not the stimulant and sympathomimetic presentation described.
- Such a mechanism would cause a **decrease** in sympathetic activity, contrary to the patient's elevated heart rate and blood pressure.
*Binds to cannabinoid receptors*
- Binding to **cannabinoid receptors** (e.g., by marijuana)
typically leads to effects such as euphoria, altered perception, impaired memory, and sometimes anxiety or paranoia.
- While hallucinations can occur, the prominent "full of energy and focus" and significant sympathetic activation (tachycardia, hypertension) are not typical of cannabinoid intoxication.
Reticular formation US Medical PG Question 5: An 18-year-old man presents to his primary care physician with a complaint of excessive daytime sleepiness. He denies any substance abuse or major changes in his sleep schedule. He reports frequently dozing off during his regular daily activities. On further review of systems, he endorses falling asleep frequently with the uncomfortable sensation that there is someone in the room, even though he is alone. He also describes that from time to time, he has transient episodes of slurred speech when experiencing heartfelt laughter. Vital signs are stable, and his physical exam is unremarkable. This patient is likely deficient in a neurotransmitter produced in which part of the brain?
- A. Hippocampus
- B. Midbrain
- C. Pons nucleus
- D. Hypothalamus (Correct Answer)
- E. Thalamus
Reticular formation Explanation: ***Hypothalamus***
- The patient's symptoms of excessive daytime sleepiness, cataplexy (falling asleep with strong emotions like laughter), and hypnagogic hallucinations (sensing someone in the room upon falling asleep) are classic for **narcolepsy**.
- Narcolepsy type 1 is characterized by a significant loss of **orexin (hypocretin)** neurons, a neuropeptide primarily produced in the **lateral hypothalamus** (specifically the lateral and perifornical areas), which plays a crucial role in maintaining wakefulness.
*Hippocampus*
- The **hippocampus** is primarily involved in **memory formation** and spatial navigation.
- Deficiencies in neurotransmitters produced or acting in the hippocampus are typically associated with memory disorders, not narcolepsy.
*Midbrain*
- The **midbrain** contains nuclei involved in dopamine, serotonin, and norepinephrine pathways, which are critical for mood, reward, and sleep-wake regulation.
- While these neurotransmitters influence the sleep-wake cycle, the primary deficiency in narcolepsy type 1 is specifically orexin, which originates from the hypothalamus, not the midbrain.
*Pons nucleus*
- The **pons** is essential for regulating sleep stages, particularly **REM sleep**, and contains nuclei involved in breathing and motor control.
- While it contributes to sleep architecture, the core pathology of narcolepsy type 1, the loss of orexin-producing neurons, is located higher in the brain, in the hypothalamus.
*Thalamus*
- The **thalamus** acts as a crucial relay station for sensory and motor signals to the cerebral cortex and is involved in regulating consciousness and alertness.
- While it is involved in arousal regulation, it is not the primary site of orexin production, nor is a neurotransmitter deficiency directly from the thalamus the primary cause of narcolepsy.
Reticular formation US Medical PG Question 6: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Reticular formation Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Reticular formation US Medical PG Question 7: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Reticular formation Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Reticular formation US Medical PG Question 8: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Reticular formation Explanation: ***Glossopharyngeal***
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
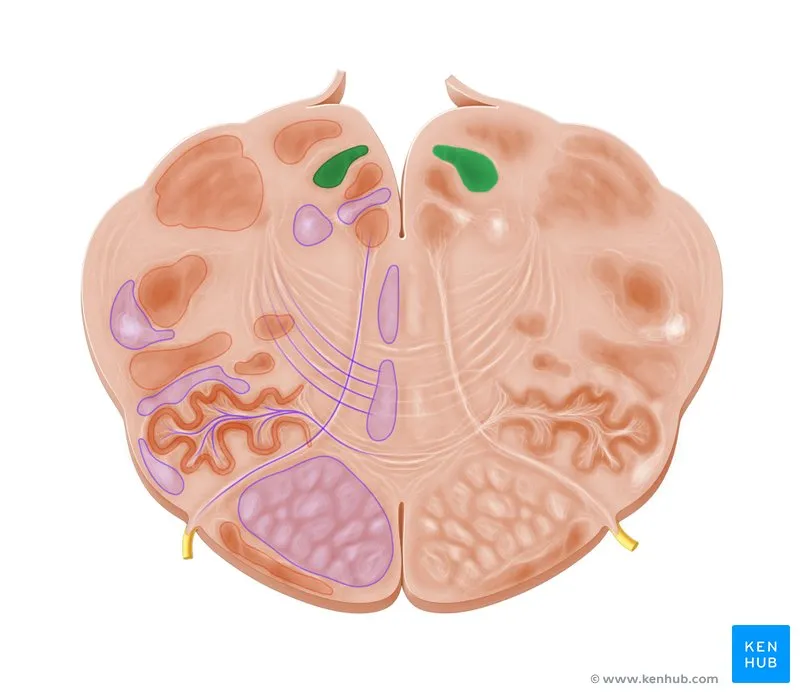
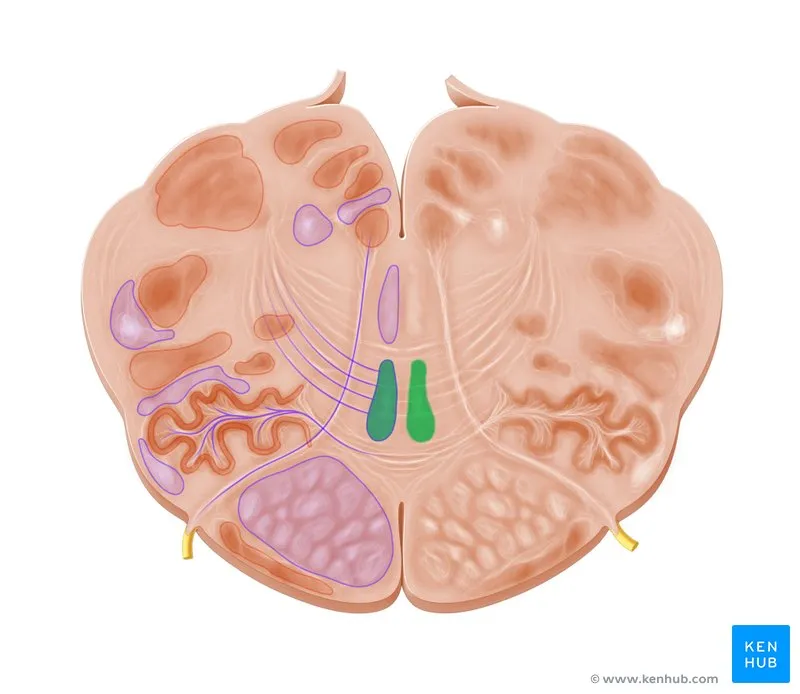
Reticular formation US Medical PG Question 9: Fibers from the marked structure terminate at which of the following?
- A. Red nucleus (Correct Answer)
- B. Subthalamus
- C. Inferior olivary nucleus
- D. Fastigial nucleus
Reticular formation Explanation: ***Red nucleus***
- The arrow points to the **superior cerebellar peduncle**, which contains efferent fibers from the **dentate nucleus** of the cerebellum.
- A major projection of the superior cerebellar peduncle is to the **contralateral red nucleus**, forming part of the **dentato-rubro-thalamic pathway**.
*Subthalamus*
- The subthalamus is part of the **diencephalon** and is involved in motor control as part of the **basal ganglia circuit**.
- It does not receive direct efferent projections from the cerebellum via the superior cerebellar peduncle.
*Inferior olivary nucleus*
- The inferior olivary nucleus is a major source of **climbing fibers** to the cerebellum, providing **afferent input** for motor learning and coordination.
- It does not receive direct efferent output from the cerebellum's deep nuclei via the superior cerebellar peduncle.
*Fastigial nucleus*
- The fastigial nucleus is one of the **deep cerebellar nuclei**, located medially.
- Its primary efferent projections are via the **inferior cerebellar peduncle** to the vestibular nuclei and reticular formation, not typically receiving fibers from the superior cerebellar peduncle.
Reticular formation US Medical PG Question 10: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Reticular formation Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
More Reticular formation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.