Descending motor pathways in brainstem US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Descending motor pathways in brainstem. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Descending motor pathways in brainstem US Medical PG Question 1: You are seeing a patient in clinic who presents with complaints of weakness. Her physical exam is notable for right sided hyperreflexia, as well as the reflex finding shown in the image below. Where is the most likely location of this patient's lesion?
- A. Postcentral gyrus
- B. Neuromuscular junction
- C. Lateral geniculate nucleus
- D. Internal capsule (Correct Answer)
- E. Subthalamic nucleus
Descending motor pathways in brainstem Explanation: ***Internal capsule***
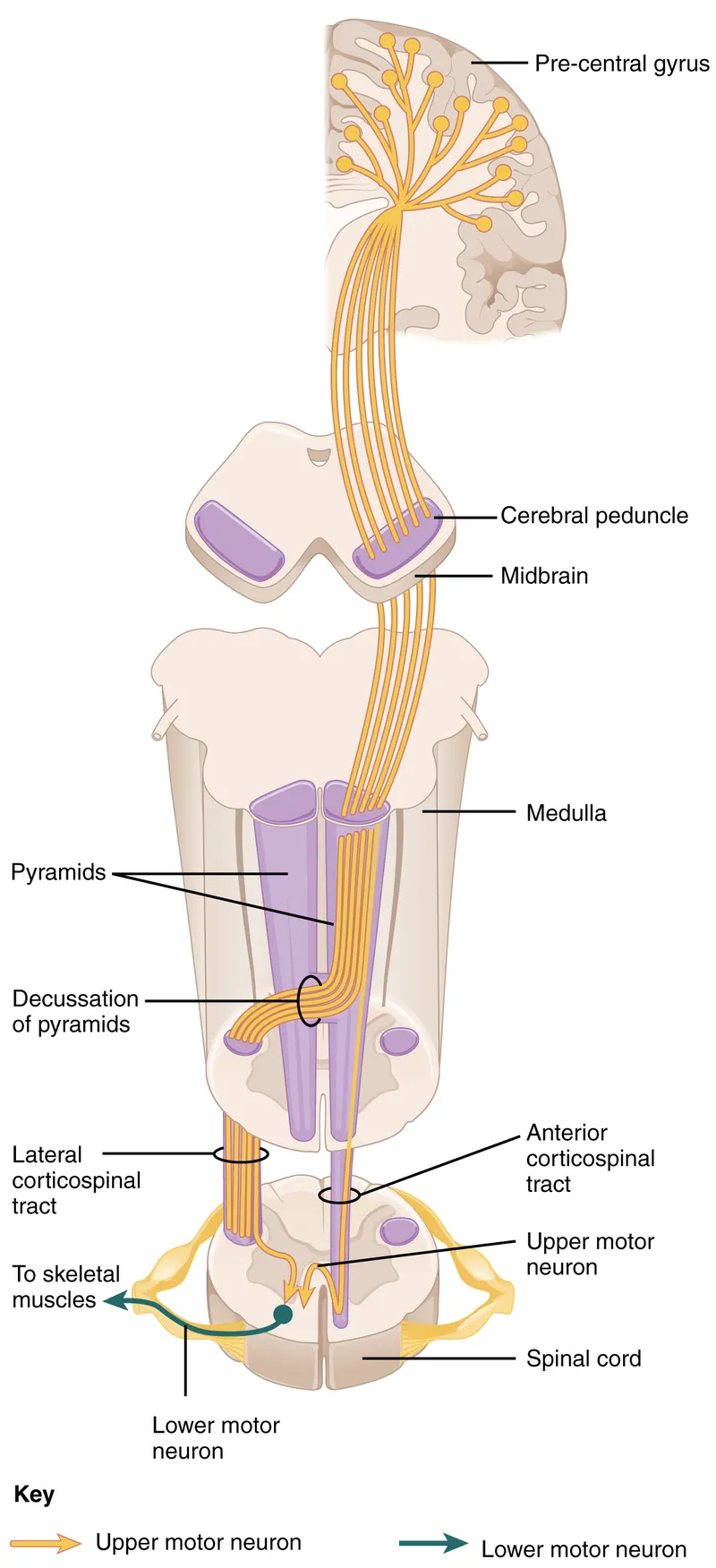
- The combination of **right-sided hyperreflexia** (an upper motor neuron sign) and a positive **Babinski sign** (as implied by a video demonstrating this reflex) points to an upper motor neuron lesion.
- The **internal capsule** contains descending motor pathways, and a lesion here would affect the contralateral side of the body, causing **weakness** and upper motor neuron signs.
*Postcentral gyrus*
- The **postcentral gyrus** is the primary somatosensory cortex and primarily deals with sensory processing, not motor output.
- A lesion here would typically cause **contralateral sensory deficits**, such as numbness or loss of proprioception, rather than motor weakness with hyperreflexia.
*Neuromuscular junction*
- Diseases of the **neuromuscular junction**, such as myasthenia gravis, cause **fatigable weakness** without hyperreflexia or other upper motor neuron signs.
- Reflexes are typically normal or decreased in these conditions.
*Lateral geniculate nucleus*
- The **lateral geniculate nucleus** is a thalamic relay center for visual information.
- Lesions here would result in **visual field deficits** (e.g., homonymous hemianopsia), not motor weakness or hyperreflexia.
*Subthalamic nucleus*
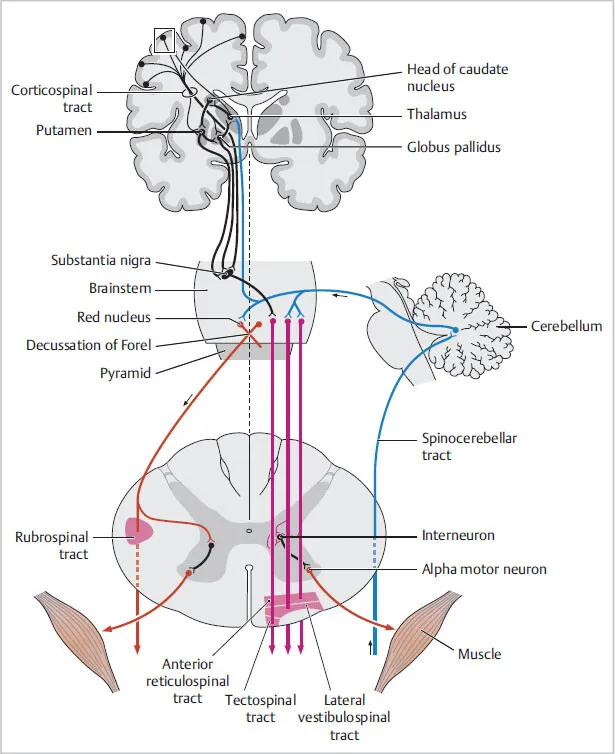
- The **subthalamic nucleus** is part of the basal ganglia and is involved in motor control, particularly in regulating movement initiation and stopping.
- Lesions here are classically associated with **hemiballismus**, which is characterized by wild, flinging movements, rather than weakness and hyperreflexia.
Descending motor pathways in brainstem US Medical PG Question 2: A 55-year-old woman presents to her family physician with a 1-week history of dizziness. She experiences spinning sensations whenever she lies down and these sensations increase when she turns her head to the right. These episodes are transient, intermittent, last for less than a minute, occur multiple times in a day, and are associated with nausea. Between the episodes, she is fine and is able to perform her routine activities. She denies fever, hearing disturbances, diplopia, tinnitus, and recent flu or viral illness. Past medical history is significant for diabetes mellitus type 2, hypertension, and hypercholesterolemia. She does not use tobacco or alcohol. Her blood pressure is 124/78 mm Hg, the heart rate is 79/min, and the respiratory rate is 13/min. During the examination, when she is asked to lie supine from a sitting position with her head rotated towards the right side at 45°, horizontal nystagmus is observed. What is the next best step in the management of this patient?
- A. Dix-Hallpike maneuver
- B. Epley maneuver (Correct Answer)
- C. MRI of the brain with gadolinium
- D. Broad-spectrum antibiotics
- E. High dose steroids
Descending motor pathways in brainstem Explanation: ***Epley maneuver***
- The patient's presentation with **transient, positional vertigo** triggered by head movements, associated with nausea, and demonstrating **horizontal nystagmus** on positional testing is diagnostic of **Benign Paroxysmal Positional Vertigo (BPPV)**.
- Since the diagnostic positional maneuver has already been performed and BPPV is confirmed, the **next best step is canalith repositioning** using the **Epley maneuver**.
- The Epley maneuver is the **gold standard treatment** for posterior canal BPPV with **70-90% success rate** after a single treatment session, and it directly addresses the underlying pathophysiology by relocating displaced otoconia.
- This is recommended as **first-line treatment** by the American Academy of Otolaryngology-Head and Neck Surgery guidelines.
*Dix-Hallpike maneuver*
- The **Dix-Hallpike maneuver** is primarily a **diagnostic test** to confirm BPPV and identify the affected semicircular canal.
- The question stem describes that a positional maneuver has already been performed with nystagmus observed, effectively confirming the diagnosis.
- While repeating the diagnostic test might be considered, it is not the next management step once BPPV is confirmed.
*MRI of the brain with gadolinium*
- This investigation is generally reserved for patients with suspected **central causes of vertigo** or other neurological deficits.
- The patient's symptoms are highly suggestive of a peripheral vestibular disorder, and the absence of **ataxia, diplopia, dysarthria**, or other focal neurological signs makes a brain MRI unnecessary at this stage.
*Broad-spectrum antibiotics*
- Antibiotics are used to treat **bacterial infections**, such as bacterial labyrinthitis or meningitis, which can cause vertigo.
- The patient denies fever, recent infections, or other signs of infection, making antibiotic therapy inappropriate for this presentation.
*High dose steroids*
- Corticosteroids are sometimes used in conditions like **vestibular neuritis** or **Meniere's disease** to reduce inflammation.
- The patient's symptoms are not consistent with these conditions; the positional nature of her vertigo and lack of continuous symptoms point away from an inflammatory process.
- Vestibular suppressants (meclizine) may provide symptomatic relief but are **adjunctive** rather than definitive treatment for BPPV.
Descending motor pathways in brainstem US Medical PG Question 3: A 55-year-old woman presents to the physician with repeated episodes of dizziness for the last 3 months, which are triggered by rising from a supine position and by lying down. The episodes are sudden and usually last for less than 30 seconds. During the episode, she feels as if she is suddenly thrown into a rolling spin. She has no symptoms in the period between episodes. The patient denies having headaches, vomiting, deafness, ear discharge or ear pain. There is no history of a known medical disorder or prolonged consumption of a specific drug. The vital signs are within normal limits. On physical examination, when the physician asks the woman to turn her head 45° to the right, and then to rapidly move from the sitting to the supine position, self-limited rotatory nystagmus is observed following her return to the sitting position. The rest of the neurological examination is normal. Which of the following is the treatment of choice for the condition of this patient?
- A. Oral prednisolone for 2 weeks and follow-up
- B. Singular neurectomy
- C. Posterior canal occlusion
- D. Canalith repositioning (Correct Answer)
- E. Oral meclizine for 6 weeks and follow-up
Descending motor pathways in brainstem Explanation: ***Canalith repositioning***
- The patient's symptoms (short-lasting, positional dizziness, rolling spin sensation, absence of other neurological symptoms, and positive **Dix-Hallpike maneuver** with **rotatory nystagmus**) are characteristic of **Benign Paroxysmal Positional Vertigo (BPPV)**.
- **Canalith repositioning maneuvers** (e.g., Epley maneuver) are the treatment of choice as they aim to move dislodged otoconia out of the semicircular canals.
*Oral prednisolone for 2 weeks and follow-up*
- **Prednisolone** is a corticosteroid used for inflammatory conditions, but it is **not indicated for BPPV**, which is a mechanical problem.
- While corticosteroids might be used in other vestibular disorders like Meniere's disease or vestibular neuritis, they would not address the underlying cause of BPPV.
*Singular neurectomy*
- **Singular neurectomy** is a surgical procedure that involves cutting the singular nerve (posterior ampullary nerve).
- This is a highly invasive treatment reserved for **intractable BPPV** that has failed multiple conservative treatments, and it carries risks such as hearing loss.
*Posterior canal occlusion*
- **Posterior canal occlusion** is a surgical procedure that involves plugging the posterior semicircular canal.
- This is a surgical option for **severe, refractory BPPV** that has not responded to canalith repositioning maneuvers, and it is more invasive than repositioning.
*Oral meclizine for 6 weeks and follow-up*
- **Meclizine** is an antihistamine used to relieve symptoms of nausea, vomiting, and dizziness associated with vertigo.
- While it can help alleviate symptoms, it does **not treat the underlying cause of BPPV** and is typically used for symptomatic relief, not as a definitive treatment.
Descending motor pathways in brainstem US Medical PG Question 4: A 78-year-old woman is accompanied by her family for a routine visit to her primary care provider. The family states that 5 months prior, the patient had a stroke and is currently undergoing physical therapy. Today, her temperature is 98.2°F (36.8°C), blood pressure is 112/72 mmHg, pulse is 64/min, and respirations are 12/min. On exam, she is alert and oriented with no deficits in speech. Additionally, her strength and sensation are symmetric and preserved bilaterally. However, on further neurologic testing, she appears to have some difficulty with balance and a propensity to fall to her right side. Which of the following deficits does the patient also likely have?
- A. Hemiballismus
- B. Hemispatial neglect
- C. Intention tremor
- D. Contralateral eye deviation
- E. Truncal ataxia (Correct Answer)
Descending motor pathways in brainstem Explanation: ***Truncal ataxia***
- This patient's symptoms of **difficulty with balance** and a **propensity to fall to her right side** are highly suggestive of truncal ataxia.
- While she had a stroke, her preserved speech, symmetric strength and sensation, and alertness rule out typical hemiparesis or aphasia, pointing towards a **cerebellar lesion** affecting balance and coordination.
*Hemiballismus*
- This condition involves **flailing, high-amplitude, involuntary movements** typically affecting one side of the body.
- The patient's description of balance issues and falling, without mention of such specific movements, makes hemiballismus less likely.
*Hemispatial neglect*
- Characterized by the **inability to attend to one side of the environment**, usually the left side following a right parietal stroke.
- The patient's presentation does not describe an indifference to one side of her visual or personal space.
*Intention tremor*
- An **intention tremor** is a tremor that worsens during purposeful movement towards a target.
- While it can be associated with cerebellar dysfunction, the primary deficit described is imbalance and falling to one side, not specifically a tremor.
*Contralateral eye deviation*
- This typically occurs in acute stroke scenarios as part of a **gaze preference**, where the eyes deviate towards the side of the lesion (or away from the hemiparesis).
- The patient is 5 months post-stroke and is alert with no acute focal deficits, making acute eye deviation unlikely as a chronic presenting symptom here.
Descending motor pathways in brainstem US Medical PG Question 5: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Descending motor pathways in brainstem Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Descending motor pathways in brainstem US Medical PG Question 6: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
Descending motor pathways in brainstem Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
Descending motor pathways in brainstem US Medical PG Question 7: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Descending motor pathways in brainstem Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Descending motor pathways in brainstem US Medical PG Question 8: A 37-year-old man presents to his primary care provider complaining of bilateral arm numbness. He was involved in a motor vehicle accident 3 months ago. His past medical history is notable for obesity and psoriatic arthritis. He takes adalimumab. His temperature is 99.3°F (37.4°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. On exam, superficial skin ulcerations are found on his fingers bilaterally. His strength is 5/5 bilaterally in shoulder abduction, arm flexion, arm extension, wrist extension, finger abduction, and thumb flexion. He demonstrates loss of light touch and pinprick response in the distal tips of his 2nd and 5th fingertips and over the first dorsal web space. Vibratory sense is intact in the bilateral upper and lower extremities. Which of the following nervous system structures is most likely affected in this patient?
- A. Cuneate fasciculus
- B. Ventral horns
- C. Anterior corticospinal tract
- D. Spinocerebellar tract
- E. Ventral white commissure (Correct Answer)
Descending motor pathways in brainstem Explanation: ***Ventral white commissure***
- The patient presents with **bilateral loss of pain (pinprick) and light touch sensation** in the upper extremity fingertips, while **vibratory sense is intact** and **motor strength is fully preserved (5/5)**. This dissociated sensory loss pattern is pathognomonic for a lesion affecting the **ventral white commissure**.
- The ventral white commissure contains **decussating fibers of the spinothalamic tract**, which carry pain and temperature sensation from the contralateral body. A lesion here (classically seen in **syringomyelia** affecting the cervical spinal cord) causes **bilateral loss of pain and temperature sensation** in a characteristic distribution while **sparing the dorsal columns** (vibratory sense and proprioception remain intact) and motor pathways.
- The **superficial skin ulcerations** on his fingers are explained by chronic loss of protective pain sensation, leading to unnoticed repetitive trauma. The motor vehicle accident 3 months ago may have precipitated or worsened an underlying syrinx.
- This is the classic **"cape-like" or suspended sensory loss** pattern, though it can present with focal dermatomal involvement as in this case.
*Cuneate fasciculus*
- The cuneate fasciculus is part of the **dorsal column-medial lemniscal pathway** that carries **vibratory sense, proprioception, and fine discriminative touch** from the upper extremities.
- A lesion here would cause **loss of vibratory sense** and proprioception, which are explicitly **intact** in this patient, making this option incorrect.
*Ventral horns*
- The ventral horns contain **lower motor neuron cell bodies** that innervate skeletal muscles.
- Damage would cause **motor deficits** including weakness (reduced strength), muscle atrophy, and fasciculations, none of which are present in this patient who has normal 5/5 strength throughout.
*Anterior corticospinal tract*
- This tract mediates **voluntary motor control**, primarily of axial and proximal muscles.
- Lesions would result in **motor weakness or spasticity**, not the isolated sensory deficits seen in this patient.
*Spinocerebellar tract*
- The spinocerebellar tracts carry **unconscious proprioceptive information** to the cerebellum for motor coordination.
- Damage would manifest as **ataxia, dysmetria, and incoordination**, which are not described in this patient's presentation.
Descending motor pathways in brainstem US Medical PG Question 9: A 22-year-old man is brought to the emergency department after he was impaled by a metal rod during a work accident. The rod went into his back around the level of T9 but was removed before arrival. He has no past medical history and does not take any medications. On physical examination, he has significant muscle weakness in his entire left lower body. He also exhibits impaired vibration and proprioception in his left leg as well as loss of pain and temperature sensation in his right leg. Which of the following sections of the spinal cord was most likely damaged in this patient?
- A. Posterior cord
- B. Anterior cord
- C. Left hemicord (Correct Answer)
- D. Central cord
- E. Right hemicord
Descending motor pathways in brainstem Explanation: ***Left hemicord***
- The combination of **ipsilateral motor weakness** and **loss of vibration/proprioception** (damage to the **corticospinal tract** and **dorsal column**) along with **contralateral loss of pain/temperature** (damage to the **spinothalamic tract**) is the classic presentation of **Brown-Séquard syndrome**, which results from a lesion affecting one side (hemicord) of the spinal cord.
- The injury at **T9** is consistent with lower body symptoms, as tracts for the legs would be affected at this level.
*Posterior cord*
- Damage to the **posterior cord** primarily affects the **dorsal columns**, leading to **ipsilateral loss of vibration and proprioception**.
- It would not explain the **ipsilateral motor weakness** or the **contralateral loss of pain and temperature sensation**.
*Anterior cord*
- **Anterior cord syndrome** typically presents with **bilateral loss of motor function** (due to damage to the corticospinal tracts) and **bilateral loss of pain and temperature sensation** (due to damage to the spinothalamic tracts).
- **Vibration and proprioception** are usually preserved because the dorsal columns are spared.
*Central cord*
- **Central cord syndrome** most commonly results from hyperextension injuries, particularly in the cervical spine, affecting the central gray matter.
- It typically causes greater **weakness in the upper extremities** than the lower extremities and a variable sensory loss, often in a **"cape-like" distribution**.
*Right hemicord*
- A **right hemicord** lesion would cause **right-sided motor weakness** and **loss of vibration/proprioception**, along with **left-sided loss of pain/temperature sensation**.
- The patient's symptoms are on the **left side for motor/proprioception** and the **right side for pain/temperature**, indicating a left hemicord lesion.
Descending motor pathways in brainstem US Medical PG Question 10: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Descending motor pathways in brainstem Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
More Descending motor pathways in brainstem US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.