Cranial nerve nuclei US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cranial nerve nuclei. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cranial nerve nuclei US Medical PG Question 1: You are seeing a patient in clinic who presents with complaints of weakness. Her physical exam is notable for right sided hyperreflexia, as well as the reflex finding shown in the image below. Where is the most likely location of this patient's lesion?
- A. Postcentral gyrus
- B. Neuromuscular junction
- C. Lateral geniculate nucleus
- D. Internal capsule (Correct Answer)
- E. Subthalamic nucleus
Cranial nerve nuclei Explanation: ***Internal capsule***
- The combination of **right-sided hyperreflexia** (an upper motor neuron sign) and a positive **Babinski sign** (as implied by a video demonstrating this reflex) points to an upper motor neuron lesion.
- The **internal capsule** contains descending motor pathways, and a lesion here would affect the contralateral side of the body, causing **weakness** and upper motor neuron signs.
*Postcentral gyrus*
- The **postcentral gyrus** is the primary somatosensory cortex and primarily deals with sensory processing, not motor output.
- A lesion here would typically cause **contralateral sensory deficits**, such as numbness or loss of proprioception, rather than motor weakness with hyperreflexia.
*Neuromuscular junction*
- Diseases of the **neuromuscular junction**, such as myasthenia gravis, cause **fatigable weakness** without hyperreflexia or other upper motor neuron signs.
- Reflexes are typically normal or decreased in these conditions.
*Lateral geniculate nucleus*
- The **lateral geniculate nucleus** is a thalamic relay center for visual information.
- Lesions here would result in **visual field deficits** (e.g., homonymous hemianopsia), not motor weakness or hyperreflexia.
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia and is involved in motor control, particularly in regulating movement initiation and stopping.
- Lesions here are classically associated with **hemiballismus**, which is characterized by wild, flinging movements, rather than weakness and hyperreflexia.
Cranial nerve nuclei US Medical PG Question 2: During an examination of the cranial nerves, a patient shows inability to move their eye laterally past the midline. Which of the following structures in the cavernous sinus is most likely affected?
- A. Oculomotor nerve
- B. Trochlear nerve
- C. Ophthalmic nerve
- D. Abducens nerve (Correct Answer)
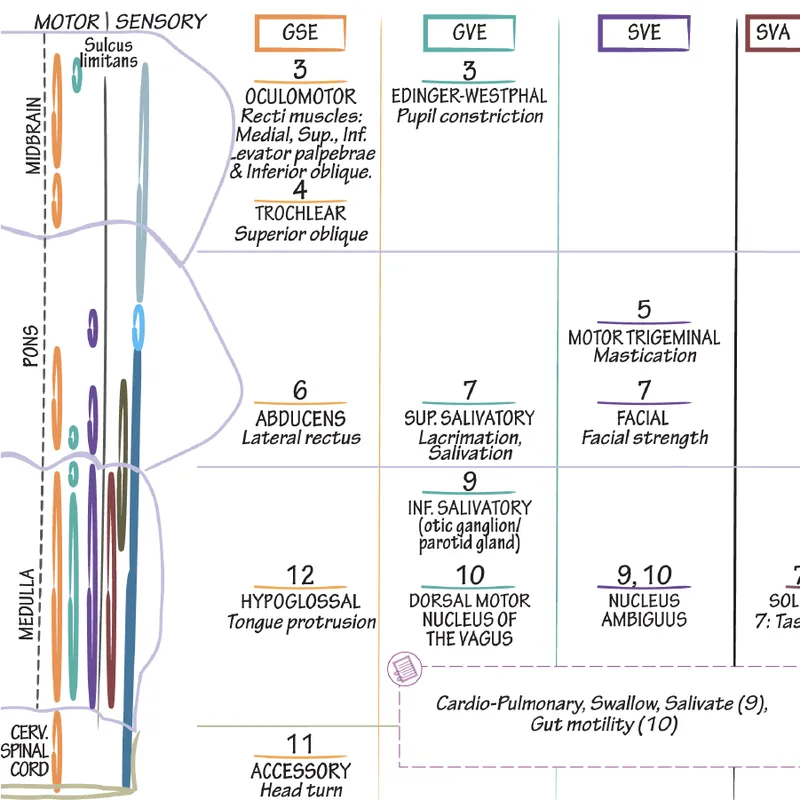
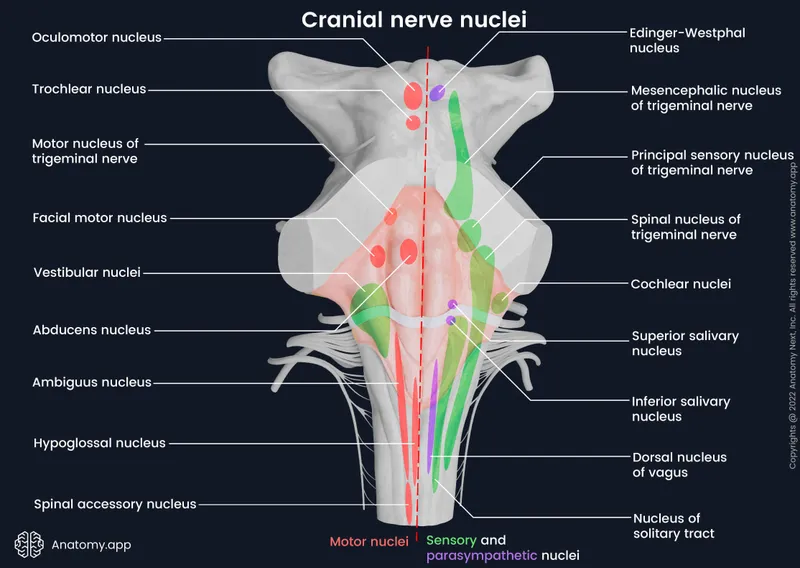
Cranial nerve nuclei Explanation: ***Abducens nerve***
- The **abducens nerve (CN VI)** innervates the **lateral rectus muscle**, responsible for **abduction** (lateral movement) of the eye [1].
- Inability to move the eye laterally past the midline indicates paralysis or weakness of the lateral rectus muscle, directly implicating the abducens nerve [1].
*Oculomotor nerve*
- The **oculomotor nerve (CN III)** controls most **extraocular muscles** (superior, inferior, medial rectus, inferior oblique) and the levator palpebrae superioris, as well as pupillary constriction [1], [2].
- Damage to this nerve would primarily affect **adduction**, elevation, depression, and eyelid opening, not isolated lateral gaze.
*Trochlear nerve*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which depresses and internally rotates the eye [1].
- A lesion here typically presents with **vertical diplopia**, particularly when reading or descending stairs, due to impaired eye depression and intorsion.
*Ophthalmic nerve*
- The **ophthalmic nerve (V1)** is one of the three divisions of the trigeminal nerve and is purely **sensory**.
- It provides sensation to the forehead, upper eyelid, cornea, and nose, and does not control any eye movements.
Cranial nerve nuclei US Medical PG Question 3: A researcher is studying the brains of patients who recently died from stroke-related causes. One specimen has a large thrombus in an area of the brain that is important in relaying many modalities of sensory information from the periphery to the sensory cortex. Which of the following embryologic structures gave rise to the part of the brain in question?
- A. Metencephalon
- B. Diencephalon (Correct Answer)
- C. Mesencephalon
- D. Telencephalon
- E. Myelencephalon
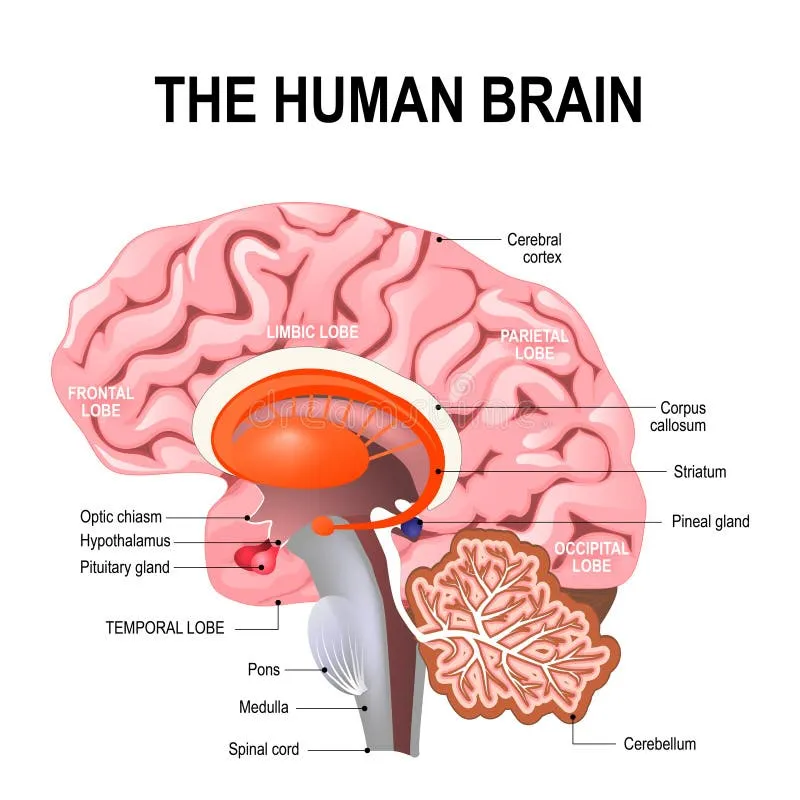
Cranial nerve nuclei Explanation: ***Diencephalon***
- The **thalamus**, a key relay center for sensory information to the cerebral cortex, develops from the diencephalon.
- A thrombus in this area would severely impair the transmission of **sensory modalities** from the periphery.
*Metencephalon*
- The metencephalon gives rise to the **pons** and the **cerebellum**.
- These structures are primarily involved in motor control, coordination, and respiratory regulation, not direct sensory relay to the cortex.
*Mesencephalon*
- The mesencephalon develops into the **midbrain**.
- The midbrain contains structures involved in visual and auditory reflexes, and motor control, but not the primary sensory relay described.
*Myelencephalon*
- The myelencephalon gives rise to the **medulla oblongata**.
- The medulla is crucial for vital autonomic functions (e.g., breathing, heart rate) and connects the brain to the spinal cord.
*Telencephalon*
- The telencephalon develops into the **cerebral hemispheres** (cerebral cortex, basal ganglia, hippocampus).
- While it processes sensory information, it is not the primary relay center from the periphery; that role belongs to the thalamus.
Cranial nerve nuclei US Medical PG Question 4: A 45-year-old patient presents with difficulty speaking and swallowing following a stroke. MRI reveals an infarct in the medulla. Which of the following cranial nerve nuclei is most likely affected?
- A. Vestibulocochlear nucleus
- B. Trigeminal nerve nucleus
- C. Facial nerve nucleus
- D. Nucleus ambiguus (Correct Answer)
Cranial nerve nuclei Explanation: ***Nucleus ambiguus***
- The **nucleus ambiguus** is located in the **medulla** and contains motor neurons that innervate muscles involved in **speaking** and **swallowing**, specifically those of the pharynx, larynx, and soft palate via cranial nerves IX, X, and XI [1].
- An infarct in the medulla causing difficulty speaking and swallowing strongly implicates damage to this nucleus, leading to **dysarthria** and **dysphagia** [1].
*Vestibulocochlear nucleus*
- This nucleus is primarily involved in **hearing** and **balance**, which would manifest as dizziness, hearing loss, or nystagmus, not directly difficulty speaking and swallowing.
- While located in the brainstem, damage to this nucleus typically does not cause the specific symptoms of dysarthria and dysphagia described.
*Trigeminal nerve nucleus*
- The trigeminal nerve is responsible for sensory innervation of the face, and motor innervation for **mastication** (chewing).
- Damage would primarily affect facial sensation or jaw movement, not the act of deglutition or phonation.
*Facial nerve nucleus*
- This nucleus, located in the **pons**, controls the muscles of **facial expression** and taste for the anterior two-thirds of the tongue.
- Damage would lead to facial weakness or paralysis, not the profound difficulty with speaking and swallowing affecting pharyngeal and laryngeal function.
Cranial nerve nuclei US Medical PG Question 5: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Cranial nerve nuclei Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Cranial nerve nuclei US Medical PG Question 6: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Cranial nerve nuclei Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Cranial nerve nuclei US Medical PG Question 7: A 72-year-old man comes to his primary care provider because of double vision and headache. He says these symptoms developed suddenly last night and have not improved. He has had type 2 diabetes mellitus for 32 years and essential hypertension for 19 years for which he takes metformin and lisinopril. His last recorded A1c was 9.4%. He has smoked 10 to 15 cigarettes a day for the past 35 years. Family history is significant for chronic kidney disease in his mother. Vital signs reveal a temperature of 36.9 °C (98.42°F), blood pressure of 137/82 mm Hg, and pulse of 72/min. On examination, there is ptosis of the right eye and it is deviated down and out. Visual acuity is not affected in either eye. Which of the following cranial nerves is most likely impaired in this patient?
- A. Facial nerve
- B. Optic nerve
- C. Oculomotor nerve (Correct Answer)
- D. Abducens nerve
- E. Trochlear nerve
Cranial nerve nuclei Explanation: ***Oculomotor nerve***
- The patient's presentation of **ptosis** (due to paralysis of the **levator palpebrae superioris** muscle) and the eye being **deviated down and out** (due to paralysis of most extraocular muscles except the superior oblique and lateral rectus) are classic signs of **oculomotor nerve (CN III) palsy**.
- Given the patient's history of **poorly controlled diabetes** and **hypertension**, microvascular ischemia is a common cause of CN III palsy that typically spares the pupil due to its superficial location.
*Facial nerve*
- Dysfunction of the **facial nerve (CN VII)** primarily affects **facial muscle movements**, leading to symptoms like facial drooping, inability to close the eye, or difficulty with smiling.
- It does not cause double vision, ptosis, or specific eye deviation patterns.
*Optic nerve*
- The **optic nerve (CN II)** is responsible for **vision (visual acuity)** and transmits visual information from the retina to the brain.
- Impairment would lead to vision loss or specific visual field defects, but not double vision, ptosis, or oculomotor abnormalities as described.
*Abducens nerve*
- The **abducens nerve (CN VI)** innervates the **lateral rectus muscle**, which is responsible for **abducting the eye** (moving it outward).
- A lesion would cause the eye to be **adducted at rest** and lead to **horizontal double vision**, especially when looking towards the affected side, which is different from "down and out" deviation.
*Trochlear nerve*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which is responsible for **intorsion, depression, and abduction of the eye**.
- Palsy typically causes **vertical double vision** that is worse when looking down and is often compensated by a head tilt away from the affected side, not ptosis or a "down and out" position.
Cranial nerve nuclei US Medical PG Question 8: A 47-year-old man presents to you with gradual loss of voice and difficulty swallowing for the past couple of months. The difficulty of swallowing is for both solid and liquid foods. His past medical history is insignificant except for occasional mild headaches. Physical exam also reveals loss of taste sensation on the posterior third of his tongue and palate, weakness in shrugging his shoulders, an absent gag reflex, and deviation of the uvula away from the midline. MRI scanning was suggested which revealed a meningioma that was compressing some cranial nerves leaving the skull. Which of the following openings in the skull transmit the affected cranial nerves?
- A. Jugular foramen (Correct Answer)
- B. Foramen rotundum
- C. Foramen spinosum
- D. Foramen ovale
- E. Foramen lacerum
Cranial nerve nuclei Explanation: ***Jugular foramen***
- The symptoms described—loss of voice, difficulty swallowing, loss of taste on the posterior third of the tongue, absent gag reflex, and uvula deviation—point to impairment of **cranial nerves IX (glossopharyngeal), X (vagus), XI (accessory)**, which all exit the skull via the **jugular foramen**.
- The **vagus nerve** (CN X) is responsible for voice and swallowing (via innervation of the pharynx and larynx), the **glossopharyngeal nerve** (CN IX) for taste from the posterior third of the tongue and the gag reflex, and the **accessory nerve** (CN XI) for shoulder shrugging (trapezius and sternocleidomastoid muscles).
- Note: Loss of taste on the palate may involve CN VII (facial nerve) fibers, but the dominant clinical picture with absent gag reflex, uvula deviation, dysphagia, and dysphonia clearly indicates jugular foramen pathology.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, a branch of the trigeminal nerve.
- Damage to V2 would primarily cause sensory deficits in the midface and upper teeth, which are not described in this patient.
*Foramen spinosum*
- The **foramen spinosum** transmits the **middle meningeal artery** and the **meningeal branch of the mandibular nerve (V3)**.
- Injury here would not explain the constellation of symptoms related to voice, swallowing, taste, or shoulder movement.
*Foramen ovale*
- The **foramen ovale** transmits the **mandibular nerve (V3)**, the **accessory meningeal artery**, and occasionally the superficial petrosal nerve.
- Damage to V3 would result in sensory loss to the lower face and motor deficits in the muscles of mastication, which are not reported.
*Foramen lacerum*
- The **foramen lacerum** is filled with cartilage in vivo and does not typically transmit major neurovascular structures directly through its aperture.
- The **internal carotid artery** passes superior to it, and some small nerves may traverse its vicinity, but not the specific cranial nerves indicated by the patient's symptoms.
Cranial nerve nuclei US Medical PG Question 9: A 32-year-old man presents to the emergency department with a severe headache. He says that the pain has been getting progressively worse over the last 24 hours and is located primarily in his left forehead and eye. The headaches have woken him up from sleep and it is not relieved by over-the-counter medications. He has been recovering from a sinus infection that started 1 week ago. His past medical history is significant for type 1 diabetes and he has a 10 pack-year history of smoking. Imaging shows thrombosis of a sinus above the sella turcica. Which of the following findings would most likely also be seen in this patient?
- A. Anosmia
- B. Mandibular pain
- C. Vertigo
- D. Ophthalmoplegia (Correct Answer)
- E. Vision loss
Cranial nerve nuclei Explanation: ***Ophthalmoplegia***
- **Cavernous sinus thrombosis** (thrombosis of a sinus above the sella turcica) most commonly causes palsy of cranial nerves III, IV, and VI, which pass through the cavernous sinus, leading to **ophthalmoplegia**
- The patient's severe headache, particularly in the eye and forehead, progressive worsening, and history of recent sinus infection are all classic features of cavernous sinus thrombosis
- The cavernous sinus contains CN III (oculomotor), CN IV (trochlear), CN VI (abducens), and branches of CN V (V1 and V2), making ophthalmoplegia the most characteristic finding
*Anosmia*
- While a sinus infection can lead to temporary **anosmia** (loss of smell), it is not a direct consequence of cavernous sinus thrombosis
- The **olfactory nerve (CN I)** is located in the roof of the nasal cavity and passes through the cribriform plate, not through the cavernous sinus
- Anosmia would be related to the preceding sinus infection itself, not the cavernous sinus thrombosis
*Mandibular pain*
- **Mandibular pain** would typically be associated with issues affecting the mandibular division of the trigeminal nerve **(CN V3)**, which does not pass through the cavernous sinus
- Although CN V1 (ophthalmic) and CN V2 (maxillary) do pass through the cavernous sinus and could cause facial pain, the predominant pain pattern in cavernous sinus thrombosis is orbital and frontal, not mandibular
- V3 exits the skull via foramen ovale and bypasses the cavernous sinus entirely
*Vertigo*
- **Vertigo** is a sensation of spinning or dizziness typically associated with vestibular dysfunction (inner ear or CN VIII/brainstem pathology)
- It is not a common or direct symptom of **cavernous sinus thrombosis**, which primarily affects structures passing through or adjacent to the cavernous sinus
- CN VIII (vestibulocochlear nerve) does not pass through the cavernous sinus
*Vision loss*
- While severe complications such as **optic nerve compression** from orbital swelling or **retinal venous congestion** can occur, direct **vision loss** is not the most common or earliest finding in cavernous sinus thrombosis
- The **optic nerve (CN II)** does not pass through the cavernous sinus itself, though it runs nearby
- Ophthalmoplegia (extraocular movement dysfunction) is far more characteristic than visual acuity loss as an initial presentation
Cranial nerve nuclei US Medical PG Question 10: A 65-year-old woman presents to her physician with the complaint of ringing in her right ear. She says it started about 3 months ago with associated progressive difficulty in hearing on the same side. Past medical history is significant for a hysterectomy 5 years ago due to dysfunctional uterine bleeding. She is currently not taking any medications. She is a non-smoker and drinks socially. On otoscopic examination, a red-blue pulsatile mass is observed behind the right tympanic membrane. A noncontrast CT scan of the head shows significant bone destruction resulting in a larger jugular foramen highly suggestive of a tumor derived from neural crest cells. Which of the cranial nerves are most likely to be involved in this type of lesion?
- A. Cranial nerves I, II, V
- B. Cranial nerves III, IV, VI
- C. Cranial nerves IX, X (Correct Answer)
- D. Cranial nerves VII & VIII
- E. Cranial nerves X, XI, XII
Cranial nerve nuclei Explanation: ***Cranial nerves IX, X***
- The symptoms of **tinnitus** and **hearing loss**, along with a **pulsatile retrotympanic mass** and **jugular foramen bone destruction**, strongly suggest a **glomus jugulare tumor**. These tumors arise from **chemoreceptor cells (paraganglia)** derived from neural crest cells located in the jugular foramen.
- The **jugular foramen** transmits the **glossopharyngeal (IX), vagus (X)**, and **accessory (XI)** cranial nerves. However, **CN IX and X are the most commonly and earliest affected** by glomus jugulare tumors due to their anatomical position.
- **Clinical involvement** of CN IX and X leads to symptoms like **dysphagia**, **hoarseness**, **loss of gag reflex**, and **vagal nerve dysfunctions**. While CN XI also passes through the jugular foramen, its involvement is typically **later and less symptomatic** in the early stages of tumor growth.
*Cranial nerves I, II, V*
- **Cranial nerve I (olfactory)** and **II (optic)** are involved in smell and vision, respectively, and are not affected by lesions in the jugular foramen.
- **Cranial nerve V (trigeminal)** supplies sensation to the face and muscles of mastication; it exits through the superior orbital fissure and foramen rotundum/ovale, not the jugular foramen.
*Cranial nerves III, IV, VI*
- These nerves (**oculomotor, trochlear, abducens**) are responsible for eye movements and are located within the **cavernous sinus** and orbit.
- Involvement of these nerves is typically associated with lesions of the cavernous sinus or superior orbital fissure, not the jugular foramen.
*Cranial nerves VII & VIII*
- **Cranial nerve VII (facial)** and **VIII (vestibulocochlear)** pass through the **internal auditory canal**, not the jugular foramen.
- While acoustic neuromas (vestibular schwannomas) cause hearing loss and involve CN VIII, a **pulsatile mass** and **jugular foramen destruction** are not characteristic of this type of lesion.
*Cranial nerves X, XI, XII*
- While **cranial nerve X (vagus)** and **XI (accessory)** do pass through the jugular foramen, **cranial nerve XII (hypoglossal)** passes through the **hypoglossal canal**, which is a completely separate opening anterior and medial to the jugular foramen.
- This option is **anatomically incorrect** because CN XII is not associated with the jugular foramen. Furthermore, the **most clinically relevant** nerves affected early in glomus jugulare tumors are CN IX and X, making the first option more accurate for "most likely to be involved."
More Cranial nerve nuclei US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.