Brainstem lesions and clinical correlations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Brainstem lesions and clinical correlations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Brainstem lesions and clinical correlations US Medical PG Question 1: A 59-year-old woman with a past medical history of atrial fibrillation currently on warfarin presents to the emergency department for acute onset dizziness. She was watching TV in the living room when she suddenly felt the room spin around her as she was getting up to go to the bathroom. She denies any fever, weight loss, chest pain, palpitations, shortness of breath, lightheadedness, or pain but reports difficulty walking and hiccups. A physical examination is significant for rotary nystagmus and decreased pin prick sensation on the left side of her body. A magnetic resonance image (MRI) of the head is obtained and shows ischemic changes of the right lateral medulla. What other symptoms would you expect to find in this patient?
- A. Left-sided tongue deviation
- B. Language impairment
- C. Paralysis of the right lower limb
- D. Right-sided facial paralysis
- E. Decreased gag reflex (Correct Answer)
Brainstem lesions and clinical correlations Explanation: ***Decreased gag reflex***
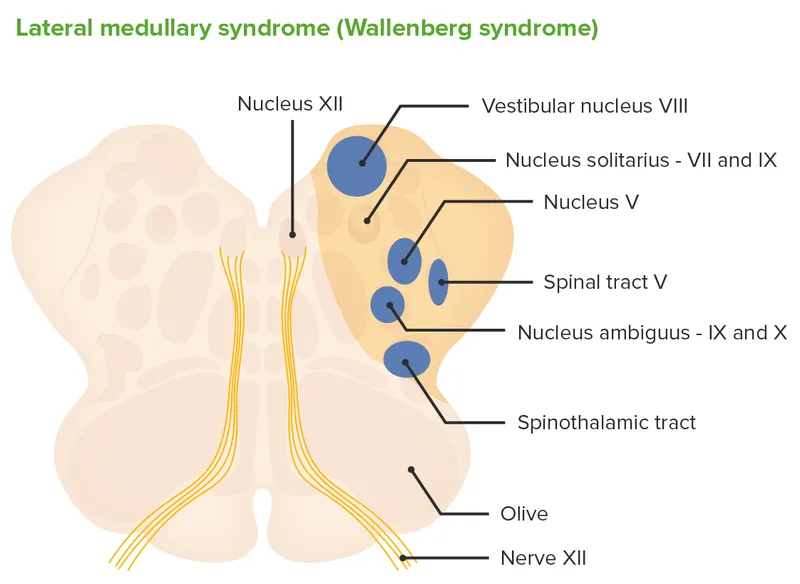
- Ischemia of the **right lateral medulla** specifically impacts the **nucleus ambiguus**, which innervates the muscles of the soft palate, pharynx, and larynx, leading to a **decreased gag reflex** and dysphagia.
- The presented symptoms of **dizziness**, **rotary nystagmus**, and **hiccups** are indicative of a lateral medullary (Wallenberg) syndrome, often presenting with **dysphagia** and a decreased gag reflex due to involvement of **cranial nerves IX and X**.
*Left-sided tongue deviation*
- Tongue deviation is associated with **hypoglossal nerve (CN XII) palsy**, which would typically involve an lesion in the **medial medulla** or a more distal nerve lesion.
- The patient's symptoms are consistent with a **lateral medullary syndrome**, where CN XII is usually spared.
*Language impairment*
- **Language impairment (aphasia)** is a cortical symptom, typically associated with lesions in the **dominant cerebral hemisphere** (Broca's or Wernicke's areas), not the brainstem.
- While brainstem strokes can cause communication difficulties, true aphasia is not characteristic of a **lateral medullary infarct**.
*Paralysis of the right lower limb*
- **Motor pathways (corticospinal tracts)** for the limbs decussate in the **pyramids of the medulla**, and a lesion in the lateral medulla typically does not involve these tracts enough to cause significant contralateral limb paralysis.
- Lateral medullary syndrome is characterized by **ipsilateral hemiataxia** and **contralateral sensory loss**, not typically contralateral motor paralysis of the limbs.
*Right-sided facial paralysis*
- **Facial paralysis** is caused by lesions affecting the **facial nerve (CN VII)** nucleus or its peripheral course, which is located more rostrally in the pons, not typically affected in a **lateral medullary infarct**.
- Lateral medullary syndrome often presents with an **ipsilateral Horner's syndrome** and **ipsilateral facial sensory loss** (due to trigeminal nucleus involvement), but not facial motor weakness.
Brainstem lesions and clinical correlations US Medical PG Question 2: A 25-year-old man presents to the emergency department with the sudden onset of neck pain and a severe spinning sensation for the last 6 hours. The symptoms initially began while he was lifting weights in the gym. He feels the room is spinning continuously, and he is unable to open his eyes or maintain his balance. The dizziness and pain are associated with nausea and vomiting. Past medical history is unremarkable. His blood pressure is 124/88 mm Hg, the heart rate is 84/min, the temperature is 37.0°C (98.6°F), the respiratory rate is 12/min, and the BMI is 21.6 kg/m2. On physical examination, he is awake and oriented to person, place, and time. Higher mental functions are intact. There are several horizontal beats of involuntary oscillatory eye movements on the left lateral gaze. He has difficulty performing repetitive pronation and supination movements on the left side. Electrocardiogram reveals normal sinus rhythm. Which of the following additional clinical features would you expect to be present?
- A. Sensory aphasia
- B. Past-pointing (Correct Answer)
- C. Expressive aphasia
- D. Hemiplegia
- E. Bitemporal hemianopsia
Brainstem lesions and clinical correlations Explanation: ***Past-pointing***
- The patient's symptoms (sudden onset of neck pain, severe spinning sensation, inability to maintain balance, horizontal nystagmus, and dysdiadochokinesia on the left) strongly suggest a posterior circulation stroke, likely involving the **cerebellum** or brainstem.
- **Past-pointing**, a form of dysmetria, is a classic sign of cerebellar dysfunction, characterized by the inability to accurately touch a target due to issues with movement coordination and range.
*Sensory aphasia*
- **Sensory aphasia** (Wernicke's aphasia) is characterized by impaired comprehension and is typically associated with damage to the **left superior temporal gyrus** (Wernicke's area) in the dominant hemisphere.
- The patient's higher mental functions are intact, making sensory aphasia an unlikely finding.
*Expressive aphasia*
- **Expressive aphasia** (Broca's aphasia) involves difficulty in speech production while comprehension remains relatively intact; it is usually linked to damage in the **left inferior frontal gyrus** (Broca's area).
- Given the intact higher mental functions and the presentation of **posterior circulation symptoms**, expressive aphasia is not expected.
*Hemiplegia*
- **Hemiplegia** (paralysis of one side of the body) points to damage in the **contralateral motor cortex** or descending motor pathways, often from an anterior circulation stroke.
- While vertebrobasilar stroke can sometimes cause motor deficits, the prominent symptoms here point to cerebellar and brainstem involvement rather than widespread motor cortex damage.
*Bitemporal hemianopsia*
- **Bitemporal hemianopsia** is a visual field defect characterized by loss of vision in the outer half of both visual fields, typically caused by compression of the **optic chiasm**, often by a pituitary tumor.
- This condition is not associated with the acute onset of vertigo, neck pain, and cerebellar signs seen in this patient's presentation.
Brainstem lesions and clinical correlations US Medical PG Question 3: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Brainstem lesions and clinical correlations Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
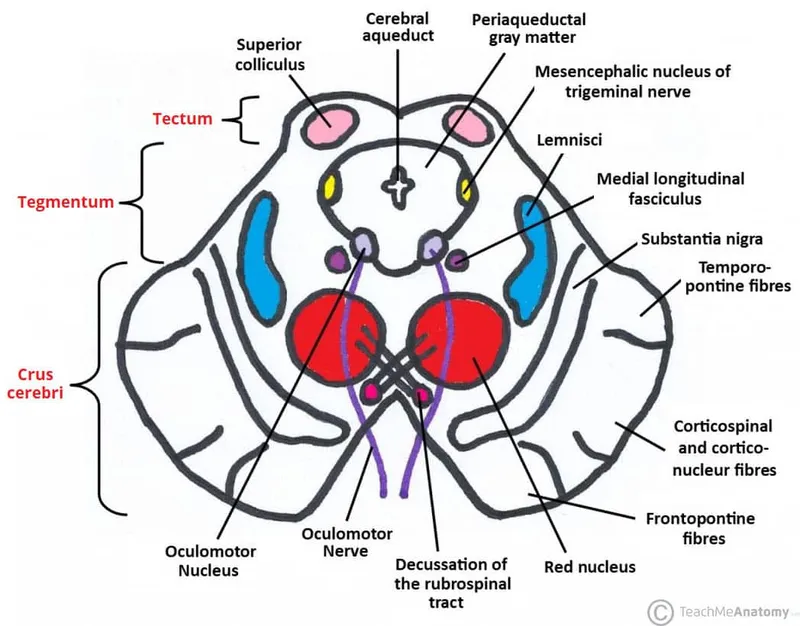
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Brainstem lesions and clinical correlations US Medical PG Question 4: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Brainstem lesions and clinical correlations Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Brainstem lesions and clinical correlations US Medical PG Question 5: A 57-year-old woman is brought to the emergency department by her husband with complaints of sudden-onset slurring for the past hour. She is also having difficulty holding things with her right hand. She denies fever, head trauma, diplopia, vertigo, walking difficulties, nausea, and vomiting. Past medical history is significant for type 2 diabetes mellitus, hypertension, and hypercholesterolemia for which she takes a baby aspirin, metformin, ramipril, and simvastatin. She has a 23-pack-year cigarette smoking history. Her blood pressure is 148/96 mm Hg, the heart rate is 84/min, and the temperature is 37.1°C (98.8°F). On physical examination, extraocular movements are intact. The patient is dysarthric, but her higher mental functions are intact. There is a right-sided facial weakness with preserved forehead wrinkling. Her gag reflex is weak. Muscle strength is mildly reduced in the right hand. She has difficulty performing skilled movements with her right hand, especially writing, and has difficulty touching far objects with her index finger. She is able to walk without difficulty. Pinprick and proprioception sensation is intact. A head CT scan is within normal limits. What is the most likely diagnosis?
- A. Locked in syndrome
- B. Pure motor syndrome
- C. Parinaud’s syndrome
- D. Dysarthria-clumsy hand syndrome (Correct Answer)
- E. Lateral medullary syndrome
Brainstem lesions and clinical correlations Explanation: ***Dysarthria-clumsy hand syndrome***
- This syndrome is characterized by **dysarthria**, **facial weakness**, and **clumsiness of the hand** (especially with fine motor movements), often affecting the contralateral side to the lesion.
- The patient's presentation with slurred speech (dysarthria), mild right-hand weakness, difficulty with skilled movements, and preserved forehead wrinkling (indicating an upper motor neuron lesion in the facial nerve distribution) is highly consistent and points to a **lacunar stroke** typically affecting the pons or internal capsule.
*Locked-in syndrome*
- This severe condition involves **complete paralysis** of nearly all voluntary muscles except for vertical eye movements and blinking, which is not described here.
- Patients are fully conscious but unable to communicate verbally or with body movements, a much more extensive deficit than presented.
*Pure motor syndrome*
- This syndrome primarily involves **weakness** without significant sensory, cerebellar, or cranial nerve involvement.
- While the patient has motor symptoms, the presence of **dysarthria** and **facial weakness** suggests more than just pure motor deficits of the limbs, differentiating it from pure motor hemiparesis.
*Parinaud’s syndrome*
- This syndrome, resulting from a lesion in the **dorsal midbrain**, presents with **vertical gaze palsy**, pupillary abnormalities, and lid retraction (Collier's sign).
- The patient's intact extraocular movements and lack of these specific eye signs rule out Parinaud's syndrome.
*Lateral medullary syndrome*
- Also known as **Wallenberg's syndrome**, it results from an infarct of the lateral medulla and is characterized by a constellation of symptoms including **vertigo**, nystagmus, ipsilateral facial numbness, contralateral body numbness, and ataxia.
- The patient explicitly denies vertigo and walking difficulties, and her sensory examination is intact, making lateral medullary syndrome unlikely.
Brainstem lesions and clinical correlations US Medical PG Question 6: A 75-year-old man is brought to the emergency room after being found unresponsive in his home. His medical history is unknown. On physical examination he does not demonstrate any spontaneous movement of his extremities and is unable to respond to voice or painful stimuli. You notice that he is able blink and move his eyes in the vertical plane. Based on these physical exam findings, you expect that magnetic resonance angiogram will most likely reveal an occlusion in which of the following vessels?
- A. Basilar artery (Correct Answer)
- B. Anterior cerebral artery
- C. Anterior spinal artery
- D. Posterior cerebral artery
- E. Anterior inferior cerebellar artery
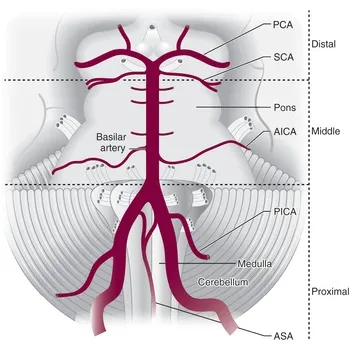
Brainstem lesions and clinical correlations Explanation: ***Basilar artery***
- The patient's presentation with **quadriplegia**, inability to respond to stimuli, and preserved **vertical eye movements** and blinking is characteristic of **locked-in syndrome**.
- **Locked-in syndrome** is most commonly caused by an **occlusion of the basilar artery**, leading to infarction of the ventral pons while sparing the tegmentum.
*Anterior cerebral artery*
- Occlusion of the **anterior cerebral artery** typically causes **contralateral leg weakness** and sensory loss, and sometimes **abulia** or urinary incontinence.
- It does not explain the widespread motor paralysis affecting all four limbs or the preservation of vertical eye movements in an otherwise unresponsive patient.
*Anterior spinal artery*
- Occlusion of the **anterior spinal artery** causes an **anterior spinal cord syndrome**, characterized by bilateral weakness and loss of pain/temperature sensation below the lesion, with preserved proprioception and vibration sense.
- This presentation does not include the characteristic signs of **brainstem dysfunction** seen in locked-in syndrome.
*Posterior cerebral artery*
- An occlusion in the **posterior cerebral artery** typically leads to **contralateral homonymous hemianopia**, and depending on the branch occluded, can also cause memory deficits or thalamic pain.
- It does not account for the extensive motor paralysis or the pattern of preserved vertical eye movements seen in locked-in syndrome.
*Anterior inferior cerebellar artery*
- Occlusion of the **anterior inferior cerebellar artery (AICA)** typically results in **lateral pontine syndrome**, which includes ipsilateral facial weakness, hearing loss, cerebellar ataxia, and contralateral loss of pain and temperature sensation.
- While it affects the pons, AICA occlusion does not typically cause the complete quadriplegia and preservation of vertical eye movements characteristic of locked-in syndrome.
Brainstem lesions and clinical correlations US Medical PG Question 7: A 32-year-old previously healthy female presents to her primary care physician with double vision. She first noted the double vision yesterday and saw no improvement this morning. She does not think it is worsening. She has not had any changes in her normal routine though she recalls one episode of right arm weakness 2 months ago. She did not seek treatment and the weakness subsided after several days. She does not have a history of head trauma. She denies headache, fever, chills, nausea, vomiting, paresthesias, extremity pain, or weakness. On exam she has right adduction palsy on leftward gaze. She has no focal weakness. Which of the following additional physical exam findings is associated with the lesion responsible for her ocular findings?
- A. Afferent pupillary defect in the left eye
- B. Horizontal nystagmus in the left eye on leftward gaze (Correct Answer)
- C. Ptosis on the right
- D. Left abduction palsy on leftward gaze
- E. Proptosis of the right eye
Brainstem lesions and clinical correlations Explanation: **Horizontal nystagmus in the left eye on leftward gaze**
- The patient presents with **double vision** and **right adduction palsy on leftward gaze**, indicative of an **internuclear ophthalmoplegia (INO)**, highly suggestive of **multiple sclerosis (MS)** in a young adult with a history of transient neurological symptoms (right arm weakness).
- In INO, the eye attempting to adduct (in this case, the right eye on leftward gaze) has impaired movement, while the contralateral abducting eye (left eye on leftward gaze) often exhibits **horizontal nystagmus**.
*Afferent pupillary defect in the left eye*
- An **afferent pupillary defect (APD)**, also known as a **Marcus Gunn pupil**, indicates a lesion to the **afferent visual pathway** (retina, optic nerve, or optic chiasm).
- While MS can cause optic neuritis leading to APD, it is not a direct consequence or associated finding of an INO itself.
*Ptosis on the right*
- **Ptosis** (drooping eyelid) is typically caused by dysfunction of the **oculomotor nerve (cranial nerve III)** or the **sympathetic pathway (Horner's syndrome)**.
- While MS can affect cranial nerves, ptosis is not a characteristic finding specifically associated with INO.
*Left abduction palsy on leftward gaze*
- A **left abduction palsy on leftward gaze** would mean the left eye is unable to fully abduct, indicating a problem with the **left abducens nerve (cranial nerve VI)** or its nucleus.
- In INO, it is the **adduction** of the ipsilateral eye that is impaired, and the contralateral eye typically **abducts normally** but with nystagmus.
*Proptosis of the right eye*
- **Proptosis** (exophthalmos) is the bulging of the eye from the orbit, usually caused by retro-orbital mass lesions (e.g., **thyroid eye disease**, orbital tumors) or inflammation.
- This finding is unrelated to the neurological lesion causing an INO.
Brainstem lesions and clinical correlations US Medical PG Question 8: A 57-year-old man was brought into the emergency department unconscious 2 days ago. His friends who were with him at that time say he collapsed on the street. Upon arrival to the ED, he had a generalized tonic seizure. At that time, he was intubated and is being treated with diazepam and phenytoin. A noncontrast head CT revealed hemorrhages within the pons and cerebellum with a mass effect and tonsillar herniation. Today, his blood pressure is 110/65 mm Hg, heart rate is 65/min, respiratory rate is 12/min (intubated, ventilator settings: tidal volume (TV) 600 ml, positive end-expiratory pressure (PEEP) 5 cm H2O, and FiO2 40%), and temperature is 37.0°C (98.6°F). On physical examination, the patient is in a comatose state. Pupils are 4 mm bilaterally and unresponsive to light. Cornea reflexes are absent. Gag reflex and cough reflex are also absent. Which of the following is the next best step in the management of this patient?
- A. Second opinion from a neurologist
- B. Withdraw ventilation support and mark time of death
- C. Electroencephalogram
- D. Repeat examination in several hours
- E. Apnea test (Correct Answer)
Brainstem lesions and clinical correlations Explanation: ***Apnea test***
- The patient exhibits classic signs of **brain death**, including a **coma**, fixed and dilated pupils, and absent brainstem reflexes (corneal, gag, cough). The next step is to perform an apnea test to confirm the absence of spontaneous respiratory drive.
- An apnea test confirms brain death by demonstrating the **absence of respiratory effort** despite a rising pCO2, provided that spinal cord reflexes are not mistaken for respiratory efforts.
*Second opinion from a neurologist*
- While consulting a neurologist is often helpful in complex neurological cases, the current clinical picture presents such clear signs of brain death that **further confirmatory testing** for brain death (like the apnea test) is more immediately indicated before seeking additional opinions on diagnosis.
- A second opinion would typically be sought to confirm the diagnosis or guide management, but establishing brain death requires a specific protocol which is incomplete without the apnea test.
*Withdraw ventilation support and mark time of death*
- It is **premature to withdraw ventilation** before brain death is unequivocally confirmed by all necessary clinical and confirmatory tests, including the apnea test.
- Withdrawing support without full confirmation could lead to ethical and legal issues, as the patient might still have residual brainstem function, however minimal.
*Electroencephalogram*
- An **EEG** can show absent electrical activity, supporting brain death, but it is **not a mandatory part of the core brain death criteria** in many protocols, especially when clinical signs are clear and an apnea test can be performed.
- The primary diagnostic criteria for brain death usually prioritize clinical examination and the apnea test for proving irreversible cessation of all brain functions.
*Repeat examination in several hours*
- Repeating the examination in several hours is typically done if there are **confounding factors** (e.g., severe hypothermia, drug intoxication) that might mimic brain death, or if the initial assessment is incomplete.
- In this case, there are no mentioned confounding factors, and the immediate priority is to complete the brain death protocol with an apnea test, given the current clear clinical picture.
Brainstem lesions and clinical correlations US Medical PG Question 9: A 26-year-old man is brought to the emergency department by ambulance after being involved in a motor vehicle collision. He does not open his eyes on command or respond to verbal cues. A CT scan of the head shows a hyperdense fluid collection in the right medial temporal lobe with medial displacement of the uncus and parahippocampal gyrus of the temporal lobe. Which of the following cranial nerves is most likely to be injured as a result of this patient's lesion?
- A. Vagus
- B. Facial
- C. Oculomotor (Correct Answer)
- D. Abducens
- E. Trigeminal
Brainstem lesions and clinical correlations Explanation: ***Oculomotor***
- The description of **medial displacement of the uncus and parahippocampal gyrus** (uncus herniation) compresses the **oculomotor nerve (CN III)** as it passes between the posterior cerebral and superior cerebellar arteries.
- Compression of the oculomotor nerve leads to a **dilated pupil** (due to parasympathetic fiber involvement) and **down-and-out deviation of the eye** (due to paralysis of extraocular muscles it innervates).
*Vagus*
- The vagus nerve (CN X) is deep within the skull and brainstem, far from the temporal lobe, and is not directly affected by uncal herniation.
- Injury to the vagus nerve typically presents with dysphagia, hoarseness, or cardiac arrhythmias, symptoms not indicated here.
*Facial*
- The facial nerve (CN VII) exits the brainstem at the pontomedullary junction and is located more superiorly and laterally than the structures involved in uncal herniation.
- Damage to the facial nerve causes facial muscle weakness or paralysis, which is not the primary concern with uncal herniation.
*Abducens*
- The abducens nerve (CN VI) is a long, slender nerve that can be affected by **generalized increases in intracranial pressure**, but is less commonly directly compressed by an uncal herniation itself.
- Injury to the abducens nerve causes **lateral rectus muscle paralysis**, leading to medial deviation of the eye, whereas uncal herniation typically affects the oculomotor nerve.
*Trigeminal*
- The trigeminal nerve (CN V) exits the pons and is located superior to the tentorial notch and medial temporal lobe, making it unlikely to be directly compressed by uncal herniation.
- Injury to the trigeminal nerve causes sensory loss in the face or weakness of the muscles of mastication, which are not consistent with the described lesion.
Brainstem lesions and clinical correlations US Medical PG Question 10: An 8-year-old boy is brought to the physician by his mother because of a 3-week history of irritability and frequent bed wetting. She also reports that he has been unable to look upward without tilting his head back for the past 2 months. He is at the 50th percentile for height and weight. His vital signs are within normal limits. Ophthalmological examination shows dilated pupils that are not reactive to light and bilateral optic disc swelling. Pubic hair development is Tanner stage 2. The most likely cause of this patient's condition is a tumor in which of the following locations?
- A. Fourth ventricle
- B. Sella turcica
- C. Cerebellar vermis
- D. Cerebral falx
- E. Dorsal midbrain (Correct Answer)
Brainstem lesions and clinical correlations Explanation: ***Dorsal midbrain***
- The inability to look upward (**Parinaud's syndrome**), dilated pupils with poor light reflex, and **optic disc swelling** (indicating increased intracranial pressure) are classic signs of a mass lesion compressing the **dorsal midbrain**, specifically the **tectal plate**.
- **Irritability and bedwetting** are nonspecific symptoms, but in this context, they could be related to **hydrocephalus** due to **aqueductal compression** by the tumor.
*Fourth ventricle*
- Tumors of the fourth ventricle typically present with symptoms related to **hydrocephalus** (headache, nausea, vomiting, papilledema) and **ataxia** due to cerebellar involvement, but not specifically with **Parinaud's syndrome**.
- **Truncal ataxia** and **gait instability** are common with posterior fossa tumors affecting the cerebellum.
*Sella turcica*
- Tumors in the sella turcica primarily affect the **pituitary gland** and **optic chiasm**, leading to **endocrine dysfunction** (e.g., growth retardation, precocious puberty, hypogonadism) and **bitemporal hemianopsia**.
- **Parinaud's syndrome** and **dilated, unreactive pupils** are not typical presentations for sellar tumors.
*Cerebral falx*
- Tumors associated with the cerebral falx (e.g., meningiomas) are often located **supratentorially** and can cause focal neurological deficits like **seizures** or **hemiparesis**, depending on their location and size.
- They do not typically cause the specific eye movement disorders or pupillary abnormalities seen in this patient.
*Cerebellar vermis*
- Cerebellar vermis tumors often lead to **truncal ataxia**, **gait disturbance**, and **hydrocephalus** due to compression of the aqueduct or fourth ventricle outflow.
- While they can cause increased intracranial pressure, they do not directly cause **Parinaud's syndrome** or isolated deficits of upward gaze.
More Brainstem lesions and clinical correlations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.