Ascending sensory pathways in brainstem US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ascending sensory pathways in brainstem. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ascending sensory pathways in brainstem US Medical PG Question 1: A 45-year-old patient presents with difficulty speaking and swallowing following a stroke. MRI reveals an infarct in the medulla. Which of the following cranial nerve nuclei is most likely affected?
- A. Vestibulocochlear nucleus
- B. Trigeminal nerve nucleus
- C. Facial nerve nucleus
- D. Nucleus ambiguus (Correct Answer)
Ascending sensory pathways in brainstem Explanation: ***Nucleus ambiguus***
- The **nucleus ambiguus** is located in the **medulla** and contains motor neurons that innervate muscles involved in **speaking** and **swallowing**, specifically those of the pharynx, larynx, and soft palate via cranial nerves IX, X, and XI [1].
- An infarct in the medulla causing difficulty speaking and swallowing strongly implicates damage to this nucleus, leading to **dysarthria** and **dysphagia** [1].
*Vestibulocochlear nucleus*
- This nucleus is primarily involved in **hearing** and **balance**, which would manifest as dizziness, hearing loss, or nystagmus, not directly difficulty speaking and swallowing.
- While located in the brainstem, damage to this nucleus typically does not cause the specific symptoms of dysarthria and dysphagia described.
*Trigeminal nerve nucleus*
- The trigeminal nerve is responsible for sensory innervation of the face, and motor innervation for **mastication** (chewing).
- Damage would primarily affect facial sensation or jaw movement, not the act of deglutition or phonation.
*Facial nerve nucleus*
- This nucleus, located in the **pons**, controls the muscles of **facial expression** and taste for the anterior two-thirds of the tongue.
- Damage would lead to facial weakness or paralysis, not the profound difficulty with speaking and swallowing affecting pharyngeal and laryngeal function.
Ascending sensory pathways in brainstem US Medical PG Question 2: A patient with a known spinal cord ependymoma presents to his neurologist for a check up. He complains that he has had difficulty walking, which he attributes to left leg weakness. On exam, he is noted to have 1/5 strength in his left lower extremity, as well as decreased vibration and position sensation in the left lower extremity and decreased pain and temperature sensation in the right lower extremity. Which of the following spinal cord lesions is most consistent with his presentation?
- A. Anterior cord syndrome
- B. Posterior cord syndrome
- C. Syringomyelia
- D. Right-sided Brown-Sequard (hemisection)
- E. Left-sided Brown-Sequard (hemisection) (Correct Answer)
Ascending sensory pathways in brainstem Explanation: ***Left-sided Brown-Sequard (hemisection)***
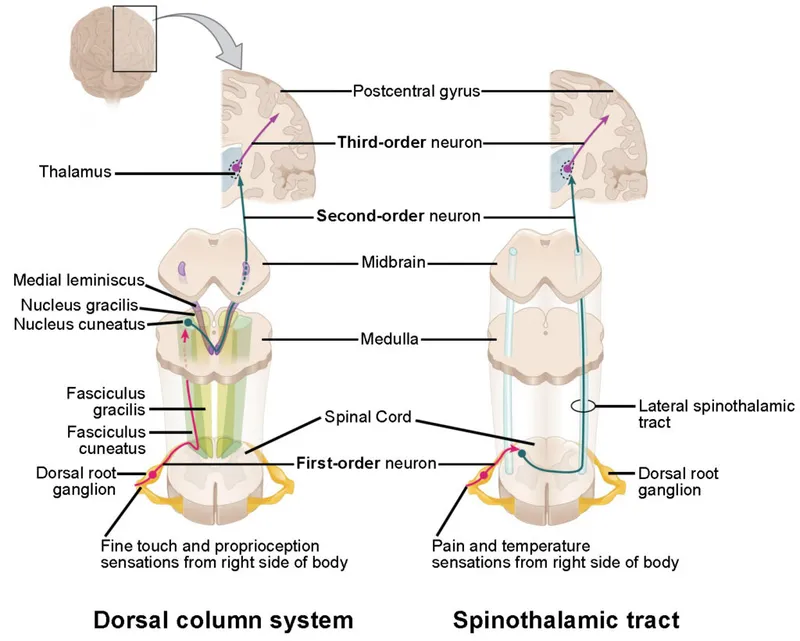
- This syndrome is characterized by **ipsilateral loss of motor function (weakness)** and **proprioception/vibration sensation** below the lesion, along with **contralateral loss of pain and temperature sensation**.
- The patient's left leg weakness, decreased vibration/position sensation in the left lower extremity, and decreased pain/temperature sensation in the right lower extremity perfectly match a **left-sided hemisection of the spinal cord**.
*Anterior cord syndrome*
- This syndrome results in **bilateral motor paralysis** and bilateral loss of **pain and temperature sensation** below the level of the lesion.
- However, **proprioception** and **vibration sense** are typically preserved, which contrasts with the patient's presentation of ipsilateral loss of these senses.
*Posterior cord syndrome*
- This rare syndrome primarily affects the **dorsal columns**, leading to bilateral loss of **vibration and proprioception** below the lesion.
- **Motor function** and **pain/temperature sensation** are largely preserved, which is inconsistent with the patient's significant motor weakness and contralateral pain/temperature loss.
*Syringomelia*
- This condition involves a fluid-filled cavity (syrinx) within the spinal cord, often causing a **cape-like distribution of pain and temperature loss** (crossing the midline) due to damage to the **decussating spinothalamic fibers**.
- While it can cause weakness, the distinct **ipsilateral proprioceptive loss** and **contralateral pain/temperature loss** seen in this patient are not typical for syringomyelia.
*Right-sided Brown-Sequard (hemisection)*
- A right-sided Brown-Sequard syndrome would present with **right-sided weakness** and **loss of proprioception/vibration sensation**, along with **left-sided loss of pain and temperature sensation**.
- This is the **opposite of the patient's presentation** of left-sided weakness and ipsilateral proprioceptive loss.
Ascending sensory pathways in brainstem US Medical PG Question 3: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Ascending sensory pathways in brainstem Explanation: ***Medulla***
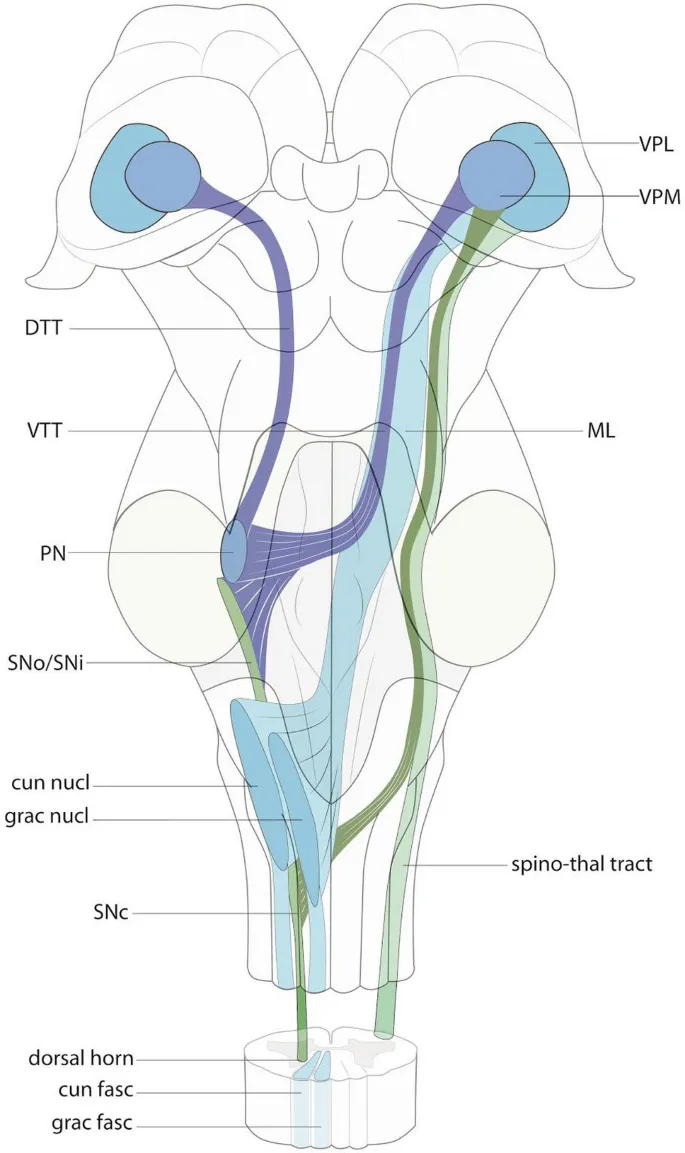
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Ascending sensory pathways in brainstem US Medical PG Question 4: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Ascending sensory pathways in brainstem Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Ascending sensory pathways in brainstem US Medical PG Question 5: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
Ascending sensory pathways in brainstem Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Ascending sensory pathways in brainstem US Medical PG Question 6: A 22-year-old man is brought to the emergency department after he was impaled by a metal rod during a work accident. The rod went into his back around the level of T9 but was removed before arrival. He has no past medical history and does not take any medications. On physical examination, he has significant muscle weakness in his entire left lower body. He also exhibits impaired vibration and proprioception in his left leg as well as loss of pain and temperature sensation in his right leg. Which of the following sections of the spinal cord was most likely damaged in this patient?
- A. Posterior cord
- B. Anterior cord
- C. Left hemicord (Correct Answer)
- D. Central cord
- E. Right hemicord
Ascending sensory pathways in brainstem Explanation: ***Left hemicord***
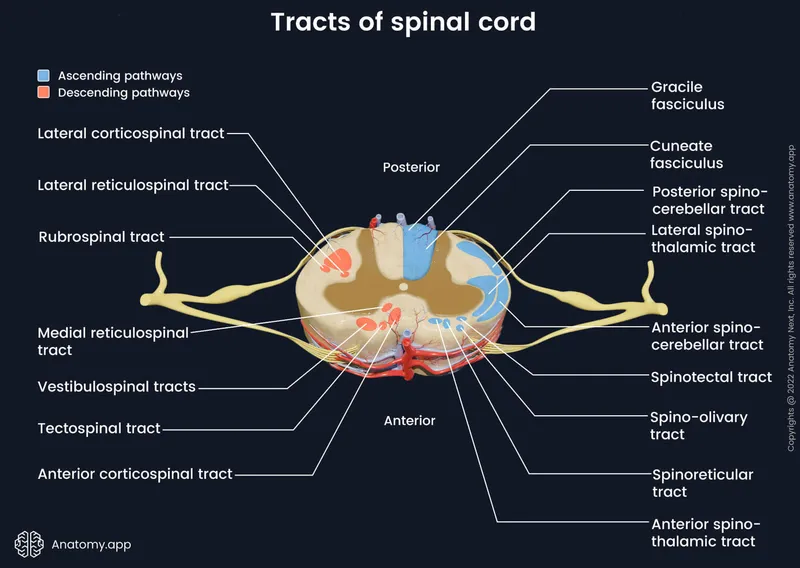
- The combination of **ipsilateral motor weakness** and **loss of vibration/proprioception** (damage to the **corticospinal tract** and **dorsal column**) along with **contralateral loss of pain/temperature** (damage to the **spinothalamic tract**) is the classic presentation of **Brown-Séquard syndrome**, which results from a lesion affecting one side (hemicord) of the spinal cord.
- The injury at **T9** is consistent with lower body symptoms, as tracts for the legs would be affected at this level.
*Posterior cord*
- Damage to the **posterior cord** primarily affects the **dorsal columns**, leading to **ipsilateral loss of vibration and proprioception**.
- It would not explain the **ipsilateral motor weakness** or the **contralateral loss of pain and temperature sensation**.
*Anterior cord*
- **Anterior cord syndrome** typically presents with **bilateral loss of motor function** (due to damage to the corticospinal tracts) and **bilateral loss of pain and temperature sensation** (due to damage to the spinothalamic tracts).
- **Vibration and proprioception** are usually preserved because the dorsal columns are spared.
*Central cord*
- **Central cord syndrome** most commonly results from hyperextension injuries, particularly in the cervical spine, affecting the central gray matter.
- It typically causes greater **weakness in the upper extremities** than the lower extremities and a variable sensory loss, often in a **"cape-like" distribution**.
*Right hemicord*
- A **right hemicord** lesion would cause **right-sided motor weakness** and **loss of vibration/proprioception**, along with **left-sided loss of pain/temperature sensation**.
- The patient's symptoms are on the **left side for motor/proprioception** and the **right side for pain/temperature**, indicating a left hemicord lesion.
Ascending sensory pathways in brainstem US Medical PG Question 7: A 61-year-old man is found dead in his home after his neighbors became concerned when they did not see him for several days. The man was described as a "recluse" who lived alone and mostly kept to himself. Medical records reveal that he had not seen a physician in over a decade. He had a known history of vascular disease including hypertension, hyperlipidemia, and diabetes mellitus. He did not take any medications for these conditions. An autopsy is performed to identify the cause of death. Although it is determined that the patient suffered from a massive cerebrovascular accident as the cause of death, an incidental finding of a tumor arising from the spinal cord meninges is noted. The tumor significantly compresses the left anterolateral lower thoracic spinal cord. The right side of the spinal cord and the posterior spinal cord appear normal. Which of the following would most likely be impaired due to this lesion?
- A. Pain sensation from the right side of the body (Correct Answer)
- B. Proprioceptive sensation from the left side of the body
- C. Temperature sensation from the left side of the body
- D. Pressure sensation from the left side of the body
- E. Vibratory sensation from the right side of the body
Ascending sensory pathways in brainstem Explanation: ***Pain sensation from the right side of the body***
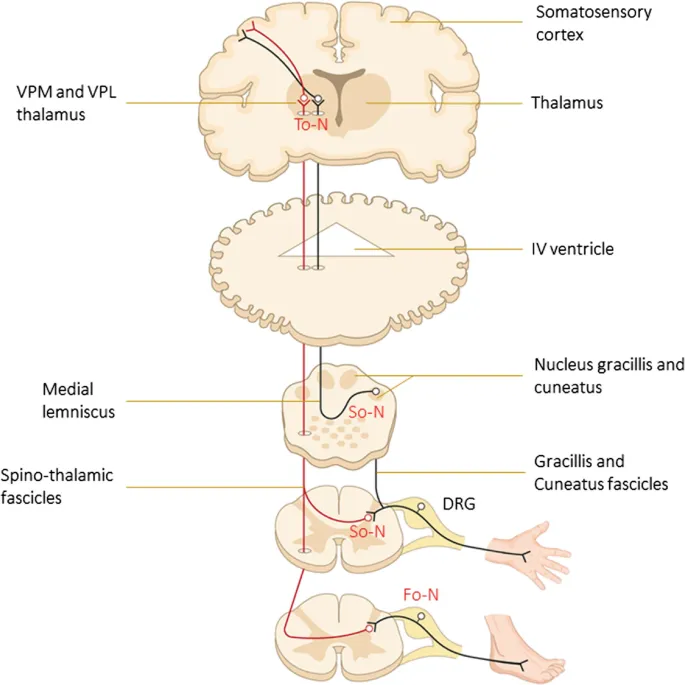
- Compression of the **left anterolateral lower thoracic spinal cord** would affect the **spinothalamic tract** on that side. The spinothalamic tract carries **pain and temperature** sensations from the **contralateral** side of the body.
- Since the fibers decussate (cross over) at the level of the spinal cord entry, a lesion on the left side of the cord would impair pain sensation from the right side of the body.
*Proprioceptive sensation from the left side of the body*
- Proprioception is carried by the **dorsal columns**, which are located in the posterior part of the spinal cord and decussate in the brainstem.
- The lesion is described as affecting the **anterolateral** left spinal cord, and the posterior cord is noted as normal, making this unlikely.
*Temperature sensation from the left side of the body*
- Temperature sensation is carried by the **spinothalamic tract**, similar to pain.
- This tract decussates at the level of entry into the spinal cord, so a lesion on the left anterolateral cord would impair temperature sensation from the **contralateral (right)** side, not the ipsilateral (left) side.
*Pressure sensation from the left side of the body*
- **Crude touch and pressure** are partially carried by the **spinothalamic tract** and partially by the **dorsal columns**.
- Impairment of pressure sensation on the left side would primarily indicate damage to the ipsilateral dorsal column pathway or significant bilateral spinothalamic involvement, neither of which is consistent with an isolated left anterolateral lesion affecting ipsilateral sensation.
*Vibratory sensation from the right side of the body*
- Vibratory sensation is carried by the **dorsal columns**, which are in the posterior spinal cord and decussate in the medulla oblongata.
- The lesion is in the **anterolateral** left spinal cord, and the posterior cord is noted as normal, making this an unlikely finding.
Ascending sensory pathways in brainstem US Medical PG Question 8: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Ascending sensory pathways in brainstem Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
Ascending sensory pathways in brainstem US Medical PG Question 9: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Ascending sensory pathways in brainstem Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
Ascending sensory pathways in brainstem US Medical PG Question 10: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Ascending sensory pathways in brainstem Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
More Ascending sensory pathways in brainstem US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.