Visceral afferent pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Visceral afferent pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Visceral afferent pathways US Medical PG Question 1: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Visceral afferent pathways Explanation: ***Pressure***
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Visceral afferent pathways US Medical PG Question 2: Which receptor type mediates the slow phase of synaptic transmission in autonomic ganglia?
- A. Muscarinic (M3)
- B. Muscarinic (M2)
- C. Muscarinic (M1) (Correct Answer)
- D. Nicotinic (N2)
Visceral afferent pathways Explanation: ***Muscarinic (M1)***
- **M1 receptors** are **Gq-protein coupled receptors** that activate phospholipase C, leading to increased intracellular calcium and diacylglycerol, which mediates the slow excitatory postsynaptic potential in autonomic ganglia.
- This activation results in a **slow depolarization** that prolongs the excitability of ganglionic neurons after the initial fast synaptic transmission.
*Muscarinic (M3)*
- **M3 receptors** are primarily found on **smooth muscle**, glands, and endothelium, mediating contraction, secretion, and vasodilation, respectively.
- While also **Gq-protein coupled**, their role in autonomic ganglia is not the main mediator of the slow phase of synaptic transmission.
*Muscarinic (M2)*
- **M2 receptors** are **Gi-protein coupled receptors** mainly found in the heart, mediating decreased heart rate and contractility.
- In autonomic ganglia, M2 receptors could have a modulatory role, but they are not responsible for the slow excitatory phase of synaptic transmission.
*Nicotinic (N2)*
- **Nicotinic N2 receptors** (also known as **NN or neuronal nicotinic receptors**) mediate the **fast excitatory postsynaptic potential** (EPSP) in autonomic ganglia by opening ion channels.
- This leads to rapid depolarization and action potential generation, which is distinct from the **slower, prolonged phase** of transmission.
Visceral afferent pathways US Medical PG Question 3: A 52-year-old man presents to his primary care physician for generalized pain. The patient states that he feels like his muscles and bones are in constant pain. This has persisted for the past several weeks, and his symptoms have not improved with use of ibuprofen or acetaminophen. The patient has a past medical history of alcohol abuse, repeat episodes of pancreatitis, constipation, and anxiety. He has a 22 pack-year smoking history. His temperature is 99.5°F (37.5°C), blood pressure is 140/95 mmHg, pulse is 70/min, respirations are 15/min, and oxygen saturation is 99% on room air. On physical exam, you note generalized tenderness/pain of the patient's extremities. Abdominal exam reveals normoactive bowel sounds and is non-tender. Dermatologic exam is unremarkable. Laboratory values are ordered as seen below.
Hemoglobin: 12 g/dL
Hematocrit: 36%
Leukocyte count: 7,500/mm^3 with normal differential
Platelet count: 147,000/mm^3
Serum:
Na+: 138 mEq/L
Cl-: 100 mEq/L
K+: 4.2 mEq/L
HCO3-: 24 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.0 mg/dL
Ca2+: 10.2 mg/dL
Alkaline phosphatase: 252 U/L
Lipase: 30 U/L
AST: 12 U/L
ALT: 10 U/L
Which of the following is associated with this patient's condition?
- A. Hypercalcemia
- B. Adenocarcinoma of the gallbladder
- C. Obstructive jaundice
- D. Bence Jones proteins
- E. Alcoholic bone disease (Correct Answer)
Visceral afferent pathways Explanation: ***Alcoholic bone disease***
- Chronic **alcohol abuse** is a major risk factor for **metabolic bone disease**, including osteoporosis and osteomalacia, which can lead to generalized bone pain.
- The patient's history of alcohol abuse, elevated **alkaline phosphatase (252 U/L)**, and generalized bone pain suggest bone disease related to chronic alcoholism.
- While "alcoholic bone disease" is not a formal diagnosis, chronic alcohol use impairs bone formation, decreases calcium absorption, and can cause vitamin D deficiency, leading to osteomalacia with elevated alkaline phosphatase.
- **Note**: This presentation is also consistent with **Paget's disease of bone** (isolated elevated alkaline phosphatase with bone pain), but given the options, the alcohol-bone disease association is the most relevant.
*Bence Jones proteins*
- These are **monoclonal light chains** found in the urine, highly suggestive of **multiple myeloma**.
- While multiple myeloma can present with bone pain and elevated alkaline phosphatase, it typically presents with **hypercalcemia**, **anemia**, and **renal dysfunction** (CRAB criteria: hyperCalcemia, Renal failure, Anemia, Bone lesions).
- This patient has **normal calcium** and **normal renal function**, making multiple myeloma less likely.
*Hypercalcemia*
- The patient's **calcium level is normal** (10.2 mg/dL; normal range 8.5-10.5 mg/dL), ruling out hypercalcemia.
- Hypercalcemia can cause bone pain, constipation, and neuropsychiatric symptoms, but is not present in this case.
*Adenocarcinoma of the gallbladder*
- This rare malignancy typically presents with **right upper quadrant pain**, **jaundice**, **weight loss**, and a palpable mass.
- The patient's **normal liver enzymes** (AST, ALT) and lack of biliary symptoms make this unlikely.
*Obstructive jaundice*
- Would present with **jaundice**, **dark urine**, **pale stools**, **pruritus**, and elevated conjugated bilirubin.
- While alkaline phosphatase can be elevated in cholestasis, the patient's **normal AST/ALT** and absence of jaundice make this unlikely.
Visceral afferent pathways US Medical PG Question 4: A 45-year-old man is brought to the emergency department by ambulance after a motor vehicle collision. He is not responsive to verbal commands and is unable to provide any history. His pulse is 108/min and regular. Physical examination shows ecchymoses over the neck and back. Neurological examination indicates damage to the spinal cord at the level shown in the illustration. This patient's injury is most likely located at which of the following levels of the spinal cord?
- A. C2
- B. S2
- C. L4
- D. T6 (Correct Answer)
- E. S4
Visceral afferent pathways Explanation: ***T6***
- The correct answer depends on identifying the spinal cord level shown in the illustration (cross-sectional anatomy).
- Injury at **T6** (mid-thoracic level) can present with:
- **Paraplegia** with loss of lower extremity function
- **Sensory level** at approximately the xiphoid process (T6 dermatome)
- Risk of **autonomic dysreflexia** if injury is complete (occurs with injuries at or above T6)
- Preserved upper extremity function and respiratory capacity
- The mid-thoracic spinal cord cross-section would show the characteristic butterfly-shaped gray matter with surrounding white matter tracts.
*C2*
- **C2** injury is a high cervical lesion that would result in:
- **Quadriplegia** (tetraplegia) affecting all four extremities
- Severe **respiratory compromise** requiring mechanical ventilation (phrenic nerve C3-C5)
- High mortality if untreated
- Cross-sectional anatomy at C2 shows enlarged gray matter for upper limb innervation.
*S2*
- **S2** injury is at the level of the conus medullaris/cauda equina and would cause:
- **Bowel and bladder dysfunction** (loss of parasympathetic control)
- **Saddle anesthesia** (loss of perineal sensation)
- Possible lower extremity weakness
- No significant autonomic instability
- Would not explain the clinical presentation in the upper body.
*L4*
- **L4** injury affects the lumbar enlargement and would cause:
- **Lower extremity weakness** (quadriceps, tibialis anterior)
- **Diminished patellar reflex**
- Sensory loss in the medial leg and foot
- Bowel/bladder may be affected
- Cross-section shows prominent gray matter for lower limb innervation.
*S4*
- **S4** is the lowest sacral level and injury would cause:
- Very limited dysfunction: **anal sphincter weakness**
- **Loss of anocutaneous reflex**
- Minimal motor or sensory deficits elsewhere
- Would not cause systemic neurological compromise.
Visceral afferent pathways US Medical PG Question 5: A 26-year-old woman presents to her gynecologist with complaints of pain with her menses and during intercourse. She also complains of chest pain that occurs whenever she has her menstrual period. The patient has a past medical history of bipolar disorder and borderline personality disorder. Her current medications include lithium and haloperidol. Review of systems is notable only for pain when she has a bowel movement relieved by defecation. Her temperature is 98.2°F (36.8°C), blood pressure is 114/74 mmHg, pulse is 70/min, respirations are 14/min, and oxygen saturation is 98% on room air. Pelvic exam is notable for a tender adnexal mass. The patient's uterus is soft, boggy, and tender. Which of the following is the most appropriate method of confirming the diagnosis in this patient?
- A. Endometrial biopsy
- B. MRI
- C. Transvaginal ultrasound
- D. Laparoscopy (Correct Answer)
- E. Clinical diagnosis
Visceral afferent pathways Explanation: ***Laparoscopy***
- **Laparoscopy** with biopsy is considered the **gold standard** for diagnosing endometriosis, allowing direct visualization of endometrial implants and histopathological confirmation.
- The patient's symptoms (dysmenorrhea, dyspareunia, chest pain with menses, and rectal pain with defecation) are highly suggestive of **endometriosis**, and pelvic exam findings (tender adnexal mass, boggy uterus) further support this, making definitive visual and histological confirmation crucial.
*Endometrial biopsy*
- An **endometrial biopsy** samples the uterine lining and is primarily used to diagnose endometrial pathologies, such as hyperplasia or carcinoma, not ectopic endometrial tissue.
- It would not detect or confirm the presence of **endometrial implants** outside the uterus, which is characteristic of endometriosis.
*MRI*
- **MRI** can identify larger endometriomas and deep infiltrating endometriosis but is generally **less sensitive** than laparoscopy for detecting small or superficial endometrial implants.
- While useful for surgical planning, it is not the **definitive diagnostic method** for all forms of endometriosis.
*Transvaginal ultrasound*
- A **transvaginal ultrasound** is a good initial imaging modality, effective for identifying **endometriomas** (cysts) and sometimes adenomyosis, but it cannot definitively diagnose peritoneal endometriosis.
- It offers **limited specificity** for small or diffuse endometrial implants, and the absence of findings does not rule out the disease.
*Clinical diagnosis*
- While the patient's symptoms are highly suggestive, relying solely on a **clinical diagnosis** of endometriosis can be inaccurate, as other conditions can mimic these symptoms.
- A definitive diagnosis is often necessary for **appropriate treatment planning** and ruling out other pathologies, especially given the presence of an adnexal mass.
Visceral afferent pathways US Medical PG Question 6: A 42-year-old woman presents to the emergency department complaining of abdominal pain, nausea, and vomiting for the last 4 hours. She says that symptoms onset right after she had 2 generous portions of pizza. She notes that she had prior similar episodes which resolved spontaneously within an hour. However, the pain today has persisted for 5 hours and is much more severe. She says the pain is located in the right upper quadrant of her abdomen and radiates to her upper back. She describes the pain as dull and cramping. She has had hypertension for the past 10 years, managed medically. Her vital signs are a blood pressure of 148/96 mm Hg, a pulse of 108/min, a respiratory rate of 18/min, and a temperature of 37.7°C (99.9°F). Her BMI is 28 kg/m2. On physical examination, the patient appears uncomfortable and is clutching her abdomen in pain. Abdominal exam reveals severe tenderness to palpation in the right upper quadrant with guarding. A positive Murphy’s sign is present. Her serum chemistry levels, including amylase, lipase, bilirubin, and liver function tests and urinalysis are normal. Urine hCG level is < 0.5 IU/L. Abdominal ultrasound reveals a large stone lodged in the neck of the gallbladder. Which of the following is the most likely pathway for referred pain in this patient?
- A. Right thoraco-abdominal intercostal nerves
- B. The phrenic nerve
- C. Greater splanchnic nerves to the spinal cord (Correct Answer)
- D. Left greater splanchnic nerve
- E. The pain endings of the visceral peritoneum
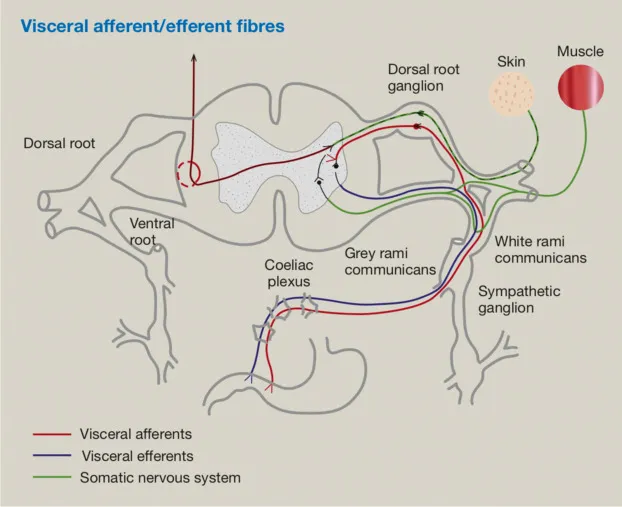
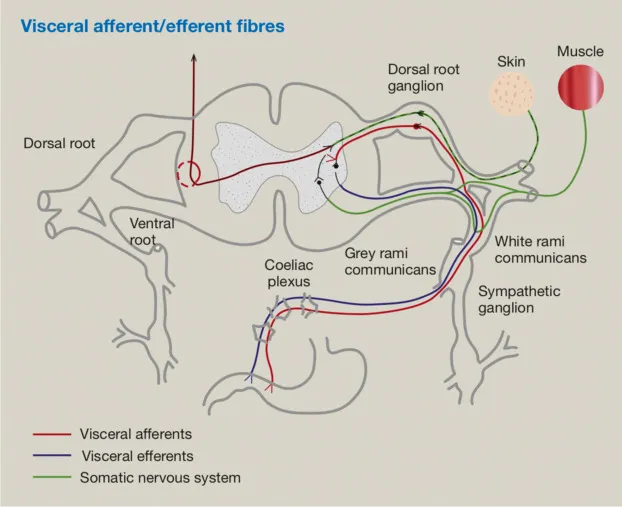
Visceral afferent pathways Explanation: ***Greater splanchnic nerves to the spinal cord***
- The **greater splanchnic nerves** (T5-T9) carry **visceral afferent fibers** from the gallbladder, transmitting pain to the spinal cord segments corresponding to the upper back (T5-T9).
- This explains the **dull, cramping right upper quadrant pain** that **radiates to the upper back**, characteristic of visceral pain from the gallbladder.
*Right thoraco-abdominal intercostal nerves*
- These nerves primarily innervate the **parietal peritoneum** and abdominal wall, responsible for sharp, localized somatic pain.
- While they could be involved in localized pain, they don't typically account for the **referred dull, cramping pain to the back** originating from a visceral organ like the gallbladder.
*The phrenic nerve*
- The **phrenic nerve** innervates the diaphragm and carries pain from the **diaphragmatic pleura and peritoneum**, often resulting in referred pain to the shoulder tip.
- Gallbladder pain can sometimes irritate the diaphragm, but the primary referral to the **upper back** is more characteristic of splanchnic nerve involvement.
*Left greater splanchnic nerve*
- The **left greater splanchnic nerve** primarily innervates organs on the left side of the upper abdomen, such as the stomach and spleen.
- Since the gallbladder is on the **right side**, its afferent pain signals travel via the right greater splanchnic nerves.
*The pain endings of the visceral peritoneum*
- The **visceral peritoneum** itself is generally insensitive to pain from cutting or burning; it senses stretch and inflammation.
- However, the pain signals from the stretched or inflamed gallbladder are transmitted via **visceral afferent fibers within the splanchnic nerves**, not directly by the visceral peritoneum's own pain endings.
Visceral afferent pathways US Medical PG Question 7: A 37-year-old man presents to his primary care provider complaining of bilateral arm numbness. He was involved in a motor vehicle accident 3 months ago. His past medical history is notable for obesity and psoriatic arthritis. He takes adalimumab. His temperature is 99.3°F (37.4°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. On exam, superficial skin ulcerations are found on his fingers bilaterally. His strength is 5/5 bilaterally in shoulder abduction, arm flexion, arm extension, wrist extension, finger abduction, and thumb flexion. He demonstrates loss of light touch and pinprick response in the distal tips of his 2nd and 5th fingertips and over the first dorsal web space. Vibratory sense is intact in the bilateral upper and lower extremities. Which of the following nervous system structures is most likely affected in this patient?
- A. Cuneate fasciculus
- B. Ventral horns
- C. Anterior corticospinal tract
- D. Spinocerebellar tract
- E. Ventral white commissure (Correct Answer)
Visceral afferent pathways Explanation: ***Ventral white commissure***
- The patient presents with **bilateral loss of pain (pinprick) and light touch sensation** in the upper extremity fingertips, while **vibratory sense is intact** and **motor strength is fully preserved (5/5)**. This dissociated sensory loss pattern is pathognomonic for a lesion affecting the **ventral white commissure**.
- The ventral white commissure contains **decussating fibers of the spinothalamic tract**, which carry pain and temperature sensation from the contralateral body. A lesion here (classically seen in **syringomyelia** affecting the cervical spinal cord) causes **bilateral loss of pain and temperature sensation** in a characteristic distribution while **sparing the dorsal columns** (vibratory sense and proprioception remain intact) and motor pathways.
- The **superficial skin ulcerations** on his fingers are explained by chronic loss of protective pain sensation, leading to unnoticed repetitive trauma. The motor vehicle accident 3 months ago may have precipitated or worsened an underlying syrinx.
- This is the classic **"cape-like" or suspended sensory loss** pattern, though it can present with focal dermatomal involvement as in this case.
*Cuneate fasciculus*
- The cuneate fasciculus is part of the **dorsal column-medial lemniscal pathway** that carries **vibratory sense, proprioception, and fine discriminative touch** from the upper extremities.
- A lesion here would cause **loss of vibratory sense** and proprioception, which are explicitly **intact** in this patient, making this option incorrect.
*Ventral horns*
- The ventral horns contain **lower motor neuron cell bodies** that innervate skeletal muscles.
- Damage would cause **motor deficits** including weakness (reduced strength), muscle atrophy, and fasciculations, none of which are present in this patient who has normal 5/5 strength throughout.
*Anterior corticospinal tract*
- This tract mediates **voluntary motor control**, primarily of axial and proximal muscles.
- Lesions would result in **motor weakness or spasticity**, not the isolated sensory deficits seen in this patient.
*Spinocerebellar tract*
- The spinocerebellar tracts carry **unconscious proprioceptive information** to the cerebellum for motor coordination.
- Damage would manifest as **ataxia, dysmetria, and incoordination**, which are not described in this patient's presentation.
Visceral afferent pathways US Medical PG Question 8: One day after undergoing surgery for a traumatic right pelvic fracture, a 73-year-old man has pain over his buttocks and scrotum and urinary incontinence. Physical examination shows right-sided perineal hypesthesia and absence of anal sphincter contraction when the skin around the anus is touched. This patient is most likely to have which of the following additional neurological deficits?
- A. Impaired hip flexion
- B. Paralysis of hip adductors
- C. Absent cremasteric reflex
- D. Impaired psychogenic erection
- E. Absent reflex erection (Correct Answer)
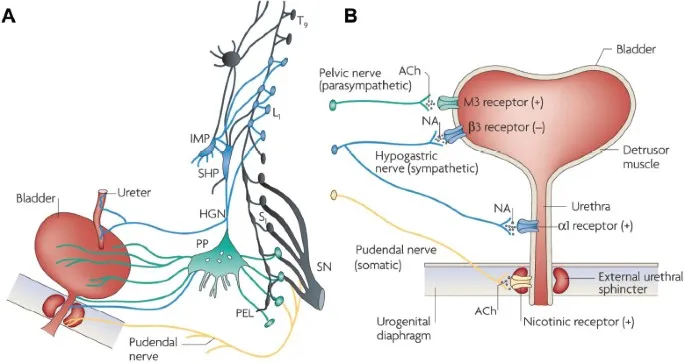
Visceral afferent pathways Explanation: ***Absent reflex erection***
- The patient's symptoms (buttock/scrotal pain, perineal hypesthesia, urinary incontinence, absent anal sphincter contraction) suggest **damage to the sacral plexus and pudendal nerve**, consistent with a **cauda equina syndrome**.
- **Reflex erections** are primarily mediated by the **sacral parasympathetic outflow (S2-S4)**, which are likely compromised given the other sacral nerve deficits.
*Impaired hip flexion*
- **Hip flexion** is primarily controlled by the **L1-L3 nerve roots** (e.g., iliopsoas muscle), and while a severe pelvic fracture could cause widespread nerve damage, the current symptoms localize more strongly to the sacral region.
- The described symptoms are more indicative of **sacral nerve involvement** rather than higher lumbar segments that govern hip flexion.
*Paralysis of hip adductors*
- **Hip adduction** is mainly innervated by the **obturator nerve (L2-L4)**.
- The patient's symptoms point to **S2-S4 nerve dysfunction** (perineal sensation, anal sphincter, bladder), which are distinct from the obturator nerve's primary innervations.
*Absent cremasteric reflex*
- The **cremasteric reflex** is mediated by the **genitofemoral nerve (L1-L2)**.
- The symptoms presented are more consistent with **sacral nerve damage**, specifically S2-S4, rather than the higher lumbar segments responsible for the cremasteric reflex.
*Impaired psychogenic erection*
- **Psychogenic erections** are initiated by **supraspinal input** descending through the thoracolumbar spinal cord (T10-L2) to activate sympathetic pathways.
- While sacral nerve damage can affect the final efferent pathway for all erections, the direct impairment of psychogenic initiation is linked to higher centers and **thoracolumbar sympathetic outflow**, not purely sacral damage.
Visceral afferent pathways US Medical PG Question 9: A 48-year-old man with retroperitoneal sarcoma requires extensive resection including portions of the sympathetic chain from T10-L2 and the celiac/superior mesenteric ganglia. Preoperative evaluation is needed to predict postoperative autonomic consequences. The multidisciplinary team must evaluate which combination of deficits is most likely based on the precise anatomical structures being resected and the potential for compensation.
- A. Pan-sympathetic failure including cardiovascular collapse due to loss of all preganglionic outflow
- B. Minimal deficits due to complete bilateral compensation from contralateral sympathetic chain
- C. Complete loss of lower extremity sweating and thermoregulation with normal GI and genitourinary function due to enteric nervous system compensation
- D. Severe orthostatic hypotension, GI dysmotility, and ejaculatory dysfunction with preserved upper body sympathetic function (Correct Answer)
- E. Isolated loss of visceral pain sensation with completely preserved motor and secretory autonomic functions
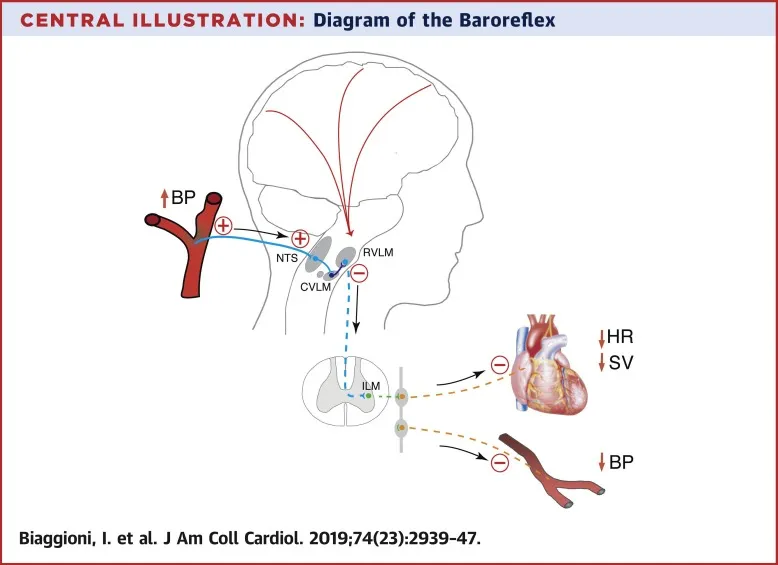
Visceral afferent pathways Explanation: ***Severe orthostatic hypotension, GI dysmotility, and ejaculatory dysfunction with preserved upper body sympathetic function***
- Resection of the **celiac and superior mesenteric ganglia** and the **sympathetic chain (T10-L2)** drastically reduces total peripheral resistance and venous return regulation, leading to **severe orthostatic hypotension**.
- Disrupting the **lumbar sympathetic chain (L1-L2)** interrupts the pathways for **emission**, while ganglionic resection causes **GI dysmotility** via loss of inhibitory sympathetic input.
*Complete loss of lower extremity sweating and thermoregulation with normal GI and genitourinary function due to enteric nervous system compensation*
- While **anhidrosis** occurs, the **enteric nervous system** cannot fully compensate for the loss of extrinsic sympathetic modulation, leading to significant GI dysfunction.
- Genitourinary function is significantly impacted as the **sympathetic input** required for the contraction of the internal urethral sphincter and seminal vesicles is removed.
*Isolated loss of visceral pain sensation with completely preserved motor and secretory autonomic functions*
- Although **visceral afferents** are interrupted, the resection of **preganglionic and postganglionic motor fibers** guarantees motor and secretory deficits.
- Sympathetic fibers are essential for the **vasoconstriction** and inhibitory signaling to the gut, which cannot remain "completely preserved" after such extensive resection.
*Pan-sympathetic failure including cardiovascular collapse due to loss of all preganglionic outflow*
- **Pan-sympathetic failure** is avoided because segments above **T10** (supplying the head, neck, and upper extremities) and the **adrenal medulla** (if T10-L2 is the primary resection) provide partial function.
- Cardiovascular collapse is unlikely because the **cardiac sympathetic nerves (T1-T4)** remain intact, maintaining heart rate and contractility.
*Minimal deficits due to complete bilateral compensation from contralateral sympathetic chain*
- Sympathetic innervation of the viscera is **bilateral**, but the **celiac and superior mesenteric ganglia** are midline structures; their resection leaves no contralateral alternative.
- Extensive **bilateral resection** of the chain segments at this level ensures profound deficits that cannot be compensated for by remaining neural pathways.
Visceral afferent pathways US Medical PG Question 10: A 62-year-old man with atrial fibrillation undergoes catheter ablation of the pulmonary vein ostia. Post-procedure, he develops gastroparesis, but his cardiologist notes preserved heart rate variability and normal baroreceptor responses. Surgical anatomy review suggests the ablation may have damaged autonomic structures. Evaluate the most likely anatomical explanation for isolated gastric dysmotility with preserved cardiovascular autonomic function.
- A. Injury to the celiac ganglion via retrograde thermal conduction
- B. Direct damage to the enteric nervous system myenteric plexus
- C. Thermal injury to epicardial vagal branches specifically innervating the stomach via the gastric plexus (Correct Answer)
- D. Damage to the stellate ganglion causing isolated sympathetic denervation of the stomach
- E. Disruption of the entire vagal trunk causing pan-autonomic dysfunction
Visceral afferent pathways Explanation: ***Thermal injury to epicardial vagal branches specifically innervating the stomach via the gastric plexus***
- The **vagus nerves** descend behind the heart and form the **esophageal plexus** near the **posterior wall of the left atrium**, making them vulnerable to energy during **pulmonary vein ablation**.
- Damage at this level can disrupt parasympathetic supply to the stomach, causing **gastroparesis**, while sparing the cardiac branches that already branched off superiorly, thereby preserving **heart rate variability**.
*Damage to the stellate ganglion causing isolated sympathetic denervation of the stomach*
- The **stellate ganglion** is located at the **C7-T1** level and supplies sympathetic fibers to the head, neck, and upper limbs; it is anatomically distant from the left atrium ablation site.
- Injury to this ganglion would present with **Horner Syndrome**, not isolated gastric dysmotility.
*Disruption of the entire vagal trunk causing pan-autonomic dysfunction*
- Complete **vagal trunk** damage would result in systemic symptoms, including significant changes in **heart rate variability** and loss of **baroreceptor reflex** sensitivity.
- The preservation of cardiovascular autonomic function indicates that the injury was localized and **distal to the cardiac branches**.
*Injury to the celiac ganglion via retrograde thermal conduction*
- The **celiac ganglion** is located in the **upper abdomen** around the root of the celiac trunk, making it an unlikely target for direct or retrograde thermal injury from the heart.
- This ganglion primarily handles **sympathetic output**; its injury would not typically cause the delayed gastric emptying characteristic of **vagal (parasympathetic) denervation**.
*Direct damage to the enteric nervous system myenteric plexus*
- The **myenteric (Auerbach’s) plexus** is located within the muscular layers of the **stomach wall**.
- Catheter ablation occurs in the **thoracic cavity** at the pulmonary veins; it cannot directly reach or damage the intrinsic nerves located within the abdominal viscus.
More Visceral afferent pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.