Sympathetic trunk anatomy US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sympathetic trunk anatomy. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sympathetic trunk anatomy US Medical PG Question 1: A 68-year-old male is diagnosed with squamous cell carcinoma in the upper lobe of his right lung. A chest radiograph can be seen in image A. Which of the following would you most expect to find in this patient?
- A. Anisocoria (Correct Answer)
- B. Superior vena cava syndrome
- C. Digital clubbing
- D. Polydipsia
- E. Lateral gaze palsy
Sympathetic trunk anatomy Explanation: ***Anisocoria***
- A tumor in the **upper lobe of the right lung** (a **Pancoast tumor**) can compress the **sympathetic chain**, leading to **Horner's syndrome**.
- **Horner's syndrome** classically presents with unilateral symptoms on the affected side, including **miosis** (constricted pupil), **ptosis** (drooping eyelid), and **anhydrosis** (decreased sweating), which would cause an apparent **anisocoria** due to the difference in pupil size.
- This is the **most expected finding** for an upper lobe lung tumor due to direct anatomical proximity to the sympathetic chain.
*Superior vena cava syndrome*
- This syndrome is usually caused by tumors in the **upper or middle mediastinum** compressing the **superior vena cava**, leading to facial and upper extremity edema, and distended neck veins.
- While it can occur with lung cancer, a tumor specifically located in the right upper lobe is **less likely** to directly compress the SVC compared to one in the mediastinum.
*Digital clubbing*
- **Digital clubbing** is a common paraneoplastic syndrome associated with various lung diseases, including **lung cancer**, particularly **adenocarcinoma**.
- While possible with squamous cell carcinoma, it is **not location-specific** and can occur with any lung tumor, making it less specific than the neurological findings expected with a Pancoast tumor.
*Polydipsia*
- **Polydipsia** (excessive thirst) can be a symptom of **hypercalcemia**, a paraneoplastic syndrome sometimes associated with **squamous cell carcinoma of the lung** due to the production of **parathyroid hormone-related peptide (PTHrP)**.
- While a possible paraneoplastic syndrome, it is a **metabolic feature** rather than a direct anatomical finding highly specific to an upper lobe tumor compressing local structures.
*Lateral gaze palsy*
- A **lateral gaze palsy** is caused by damage to the **abducens nerve (CN VI)** or its nucleus, leading to an **inability to move the eye laterally**.
- This symptom is **not typically associated** with a primary lung tumor in the upper lobe unless there is widespread metastatic disease affecting the brainstem or cranial nerves, which is not directly indicated.
Sympathetic trunk anatomy US Medical PG Question 2: A 50-year-old man presents to his primary care provider complaining of double vision and trouble seeing out of his right eye. His vision started worsening about 2 months ago and has slowly gotten worse. It is now severely affecting his quality of life. Past medical history is significant for poorly controlled hypertension and hyperlipidemia. He takes amlodipine, atorvastatin, and a baby aspirin every day. He smokes 2–3 cigarettes a day and drinks a glass of wine with dinner every night. Today, his blood pressure is 145/85 mm Hg, heart rate is 90/min, respiratory rate is 14/min, and temperature is 37.0°C (98.6°F). On physical exam, he appears pleasant and talkative. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. Examination of the eyes reveals a dilated right pupil that is positioned inferolateral with ptosis. An angiogram of the head and neck is performed and he is referred to a neurologist. The angiogram reveals a 1 cm berry aneurysm at the junction of the posterior communicating artery and the posterior cerebral artery compressing the oculomotor nerve. Which of the following statements best describes the mechanism behind the oculomotor findings seen in this patient?
- A. The parasympathetic nerve fibers of this patient’s eye are activated.
- B. The sympathetic nerve fibers of this patient’s eye are inhibited.
- C. The unopposed inferior oblique muscle rotates the eye downward.
- D. The unopposed superior oblique muscle rotates the eye downward. (Correct Answer)
- E. The unopposed medial rectus muscle rotates the eye in the lateral direction.
Sympathetic trunk anatomy Explanation: ***The unopposed superior oblique muscle rotates the eye downward.***
- The **oculomotor nerve** (CN III) innervates most extraocular muscles, including the **superior rectus, inferior rectus, medial rectus, and inferior oblique**, as well as the **levator palpebrae superioris** and **parasympathetic fibers** to the pupillary sphincter.
- With a complete **oculomotor nerve palsy**, the only remaining functional extraocular muscles are the **lateral rectus** (innervated by CN VI) and the **superior oblique** (innervated by CN IV), which causes the eye to be positioned **down and out** due to their unopposed actions.
*The parasympathetic nerve fibers of this patient’s eye are activated.*
- **Parasympathetic fibers** within the oculomotor nerve control **pupillary constriction** and lens accommodation.
- Compression of the oculomotor nerve, especially by an aneurysm, typically affects these superficial parasympathetic fibers first, leading to **pupillary dilation** (mydriasis) due to their impairment, not activation.
*The sympathetic nerve fibers of this patient’s eye are inhibited.*
- **Sympathetic innervation** to the eye controls pupillary dilation, eyelid elevation (via Müller's muscle), and sweat gland function.
- Inhibition of sympathetic fibers would lead to **miosis** (constricted pupil) and **ptosis** (drooping eyelid) as seen in **Horner's syndrome**, which is not the primary presentation of oculomotor nerve compression.
*The unopposed inferior oblique muscle rotates the eye downward.*
- The **inferior oblique muscle** elevates and abducts the eye; it is innervated by the **oculomotor nerve**.
- In an oculomotor nerve palsy, the inferior oblique muscle is **paralyzed**, thus it cannot exert any rotational force on the eye.
*The unopposed medial rectus muscle rotates the eye in the lateral direction.*
- The **medial rectus muscle** adducts the eye (moves it medially); it is innervated by the **oculomotor nerve**.
- In an oculomotor nerve palsy, the medial rectus is paralyzed, and its unopposed action would not cause lateral rotation; rather, the **lateral rectus** (innervated by CN VI) would cause the eye to deviate laterally.
Sympathetic trunk anatomy US Medical PG Question 3: A 72-year-old man presents to his primary care physician because he feels like his vision has been changing over the last 6 months. In particular, he feels that he cannot see as well out of his right eye as previously. His past medical history is significant for myocardial infarction as well as Lyme disease. On presentation, he is found to have a droopy right eyelid as well as persistent constriction of his right pupil. Additionally, the skin on his right half of his face is found to be cracked and dry. Which of the following is most likely associated with this patient's symptoms?
- A. Oculomotor nerve damage
- B. Drug use
- C. Syphilis
- D. Facial nerve damage
- E. Pancoast tumor (Correct Answer)
Sympathetic trunk anatomy Explanation: ***Pancoast tumor***
- The patient's symptoms (droopy eyelid, constricted pupil, and dry skin on one side of the face) are classic for **Horner's syndrome**, which results from damage to the **sympathetic nerves** to the eye and face.
- A **Pancoast tumor** (a tumor in the apex of the lung) can compress the **sympathetic chain** in the neck/chest, leading to Horner's syndrome.
*Oculomotor nerve damage*
- Oculomotor nerve damage would typically cause a **dilated pupil** (due to unopposed sympathetic innervation) and **ptosis** (drooping eyelid), but not miosis (constricted pupil) or anhidrosis (dry skin).
- The patient's **constricted pupil** points away from oculomotor nerve involvement.
*Drug use*
- While certain drugs can affect pupil size (e.g., opiates cause miosis), drug use alone is unlikely to explain the entire triad of **Horner's syndrome** (ptosis, miosis, anhidrosis) in combination with the focal neurological findings.
- No other information in the vignette suggests drug use.
*Syphilis*
- **Neurosyphilis** can cause pupillary abnormalities, such as **Argyll Robertson pupils** (small, irregular pupils that accommodate but do not react to light).
- However, it typically does not present with the specific combination of ptosis, miosis, and anhidrosis characteristic of Horner's syndrome.
*Facial nerve damage*
- **Facial nerve damage** (e.g., Bell's palsy) affects the muscles of **facial expression** and could cause ipsilateral facial weakness or droop.
- It would not cause pupillary changes or anhidrosis, as these symptoms are related to the sympathetic nervous system and superior cervical ganglion, not the facial nerve.
Sympathetic trunk anatomy US Medical PG Question 4: A 21-year-old man was involved in a motor vehicle accident and died. At autopsy, the patient demonstrated abnormally increased mobility at the neck. A section of cervical spinal cord at C6 was removed and processed into slides. Which of the following gross anatomic features is most likely true of this spinal cord level?
- A. Cuneate and gracilis fasciculi are present (Correct Answer)
- B. Least amount of white matter
- C. Prominent lateral horns
- D. Absence of gray matter enlargement
- E. Involvement with parasympathetic nervous system
Sympathetic trunk anatomy Explanation: **Cuneate and gracilis fasciculi are present**
- At the **C6 level** of the spinal cord, both the **fasciculus gracilis** (carrying information from the lower body) and the **fasciculus cuneatus** (carrying information from the upper body) are present in the dorsal column.
- The fasciculus cuneatus typically appears at **T6 and above**, making it visible at C6.
*Least amount of white matter*
- The cervical spinal cord, particularly at C6, contains a **significant amount of white matter** because it carries all ascending and descending tracts to and from the brain, including those for the upper and lower limbs.
- The **sacral segments** typically have the least amount of white matter due to fewer tracts remaining.
*Prominent lateral horns*
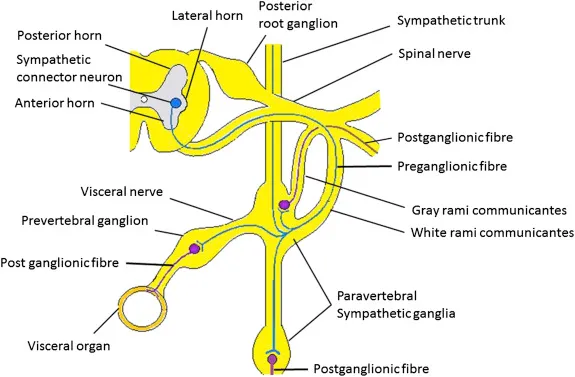
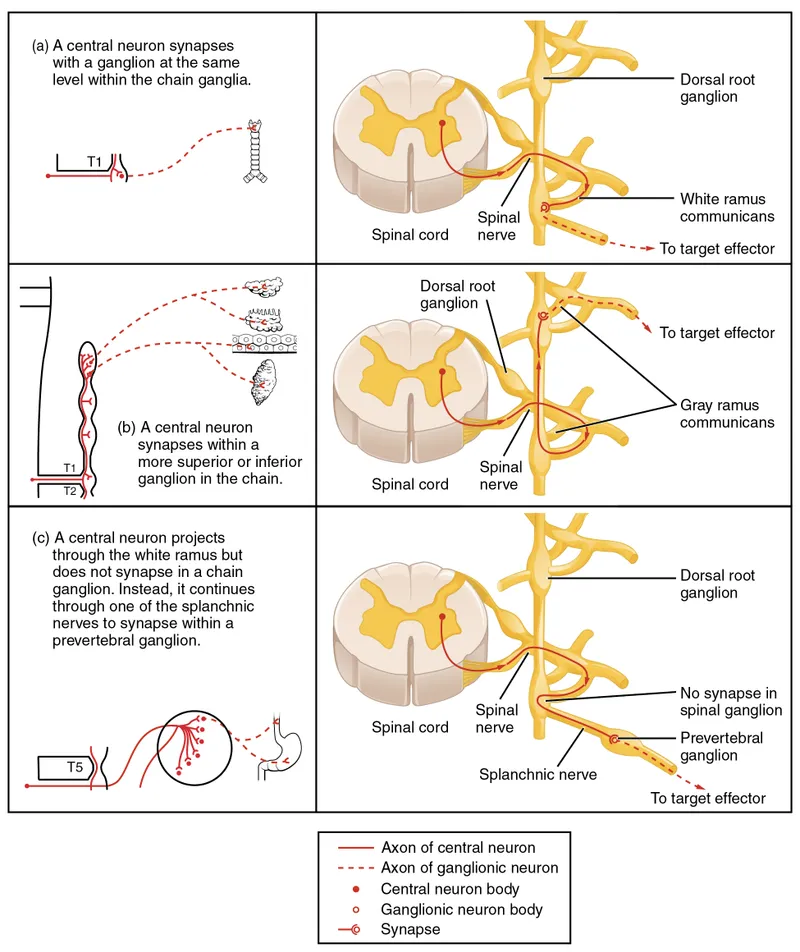
- **Lateral horns** are characteristic of the **thoracic and upper lumbar (T1-L2/L3)** spinal cord segments, where they house preganglionic sympathetic neurons.
- They are generally **absent or poorly developed** in the cervical spinal cord.
*Absence of gray matter enlargement*
- The **cervical enlargement** of the spinal cord, particularly pronounced from C4 to T1, contains an increased amount of gray matter to accommodate the innervation of the **upper limbs**.
- Therefore, the C6 level would show **significant gray matter enlargement**.
*Involvement with parasympathetic nervous system*
- The **parasympathetic nervous system** exits the spinal cord at the **sacral levels (S2-S4)** and as cranial nerves, not primarily from the cervical spinal cord through distinct horns.
- The cervical spinal cord is primarily associated with **somatic motor and sensory pathways** for the neck, shoulders, and upper limbs, and receives some sympathetic input, but is not where parasympathetic outflow predominantly originates.
Sympathetic trunk anatomy US Medical PG Question 5: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Sympathetic trunk anatomy Explanation: ***S3–S4 nerve roots***
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Sympathetic trunk anatomy US Medical PG Question 6: During a physical examination, a physician tests the strength of hip adduction against resistance. Which of the following nerves innervates the primary muscles responsible for this action?
- A. Sciatic nerve
- B. Superior gluteal nerve
- C. Femoral nerve
- D. Obturator nerve (Correct Answer)
Sympathetic trunk anatomy Explanation: ***Obturator nerve***
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh, including the adductor longus, adductor brevis, adductor magnus (adductor part), gracilis, and pectineus (variable innervation).
- These muscles are responsible for **adducting the hip**, which is the action tested when a physician checks hip adduction strength against resistance.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and all muscles below the knee.
- It does not significantly contribute to the innervation of the primary hip adductors.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles.
- These muscles are primarily involved in **hip abduction** and medial rotation, not adduction.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) and the sartorius.
- Its primary actions are **knee extension** and hip flexion, with no direct role in hip adduction.
Sympathetic trunk anatomy US Medical PG Question 7: A 61-year-old man sustains an intracranial injury to a nerve that also passes through the parotid gland. Which of the following is a possible consequence of this injury?
- A. Changes in hearing (Correct Answer)
- B. Horner's syndrome
- C. Paralysis of lateral rectus muscle
- D. Loss of taste from posterior 1/3 of tongue
- E. Loss of general sensation in anterior 2/3 of tongue
Sympathetic trunk anatomy Explanation: ***Changes in hearing***
- The **facial nerve (CN VII)** is the only cranial nerve that has both an **intracranial course** and passes **through the parotid gland**.
- The facial nerve gives off the **nerve to stapedius muscle** within the facial canal (before it exits the stylomastoid foramen).
- Damage to this nerve can lead to **hyperacusis** (increased sensitivity to sound), as the stapedius normally dampens excessive sound vibrations.
- **Note**: Facial nerve injury would also cause facial paralysis (the most prominent feature), loss of taste from anterior 2/3 of tongue via chorda tympani, and decreased lacrimation/salivation, but these are not among the answer choices.
*Horner's syndrome*
- This syndrome results from damage to the **sympathetic pathway** (hypothalamus → spinal cord → superior cervical ganglion → eye).
- Characterized by **ptosis**, **miosis**, and **anhidrosis**.
- Not related to facial nerve injury.
*Paralysis of lateral rectus muscle*
- The **lateral rectus muscle** is innervated by the **abducens nerve (CN VI)**.
- CN VI does not pass through the parotid gland.
*Loss of taste from posterior 1/3 of tongue*
- Taste from the **posterior 1/3 of the tongue** is carried by the **glossopharyngeal nerve (CN IX)**.
- CN IX does not pass through the parotid gland.
- **Note**: The facial nerve actually carries taste from the **anterior 2/3** of the tongue via the chorda tympani branch.
*Loss of general sensation in anterior 2/3 of tongue*
- **General sensation** (touch, pain, temperature) from the **anterior 2/3 of the tongue** is carried by the **lingual nerve** (branch of CN V3).
- The lingual nerve does not pass through the parotid gland.
Sympathetic trunk anatomy US Medical PG Question 8: A 39-year-old woman is brought to the emergency department following a stab wound to the neck. Per the patient, she was walking her dog when she got robbed and was subsequently stabbed with a knife. Vitals are stable. Strength examination reveals 2/5 right-sided elbow flexion and extension, wrist extension, and finger motions. Babinski sign is upward-going on the right. There is decreased sensation to light touch and vibration on the patient's right side up to her shoulder. She also reports decreased sensation to pinprick and temperature on her left side, including her lower extremities, posterior forearm, and middle finger. The patient's right pupil is 2 mm smaller than the left with drooping of the right upper eyelid. Which of the following is the most likely cause of the patient’s presentation?
- A. Hemisection injury (Correct Answer)
- B. Syringomyelia
- C. Anterior cord syndrome
- D. Posterior cord syndrome
- E. Central cord syndrome
Sympathetic trunk anatomy Explanation: ***Hemisection injury***
- The combination of **ipsilateral motor weakness** and **dorsal column deficits** (vibration, light touch) along with **contralateral loss of pain and temperature sensation** (spinothalamic tract) is the hallmark of a Brown-Séquard syndrome, which results from a hemisection injury to the spinal cord.
- The presence of **ipsilateral Horner's syndrome** (miosis and ptosis) indicates sympathetic nerve damage, further localizing the injury to the cervical spinal cord and supporting a hemisection.
*Syringomyelia*
- This condition is characterized by a **cavity (syrinx)** within the spinal cord, typically leading to a **cape-like distribution of pain and temperature loss** due to damage to the decussating spinothalamic fibers.
- It usually spares the dorsal columns and motor tracts in early stages, which contradicts the described ipsilateral motor and dorsal column deficits.
*Anterior cord syndrome*
- Results from damage to the **anterior spinal artery**, leading to **bilateral loss of motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts) below the level of injury.
- **Proprioception and vibration sensation** (dorsal columns) are typically preserved in this syndrome, which is inconsistent with the patient's presentation.
*Posterior cord syndrome*
- Involves damage primarily to the **dorsal columns**, resulting in **loss of proprioception, vibration, and light touch** below the level of injury.
- **Motor function, pain, and temperature sensation** are generally preserved, which is not consistent with the motor deficits and contralateral pain/temperature loss described.
*Central cord syndrome*
- Most commonly seen after **hyperextension injuries**, leading to greater **motor weakness in the upper extremities** than the lower extremities.
- It typically causes varying degrees of **sensory loss** and can preserve sacral sensation, but the specific pattern of ipsilateral motor/dorsal column deficits and contralateral spinothalamic loss is not characteristic of central cord syndrome.
Sympathetic trunk anatomy US Medical PG Question 9: A 48-year-old man with retroperitoneal sarcoma requires extensive resection including portions of the sympathetic chain from T10-L2 and the celiac/superior mesenteric ganglia. Preoperative evaluation is needed to predict postoperative autonomic consequences. The multidisciplinary team must evaluate which combination of deficits is most likely based on the precise anatomical structures being resected and the potential for compensation.
- A. Pan-sympathetic failure including cardiovascular collapse due to loss of all preganglionic outflow
- B. Minimal deficits due to complete bilateral compensation from contralateral sympathetic chain
- C. Complete loss of lower extremity sweating and thermoregulation with normal GI and genitourinary function due to enteric nervous system compensation
- D. Severe orthostatic hypotension, GI dysmotility, and ejaculatory dysfunction with preserved upper body sympathetic function (Correct Answer)
- E. Isolated loss of visceral pain sensation with completely preserved motor and secretory autonomic functions
Sympathetic trunk anatomy Explanation: ***Severe orthostatic hypotension, GI dysmotility, and ejaculatory dysfunction with preserved upper body sympathetic function***
- Resection of the **celiac and superior mesenteric ganglia** and the **sympathetic chain (T10-L2)** drastically reduces total peripheral resistance and venous return regulation, leading to **severe orthostatic hypotension**.
- Disrupting the **lumbar sympathetic chain (L1-L2)** interrupts the pathways for **emission**, while ganglionic resection causes **GI dysmotility** via loss of inhibitory sympathetic input.
*Complete loss of lower extremity sweating and thermoregulation with normal GI and genitourinary function due to enteric nervous system compensation*
- While **anhidrosis** occurs, the **enteric nervous system** cannot fully compensate for the loss of extrinsic sympathetic modulation, leading to significant GI dysfunction.
- Genitourinary function is significantly impacted as the **sympathetic input** required for the contraction of the internal urethral sphincter and seminal vesicles is removed.
*Isolated loss of visceral pain sensation with completely preserved motor and secretory autonomic functions*
- Although **visceral afferents** are interrupted, the resection of **preganglionic and postganglionic motor fibers** guarantees motor and secretory deficits.
- Sympathetic fibers are essential for the **vasoconstriction** and inhibitory signaling to the gut, which cannot remain "completely preserved" after such extensive resection.
*Pan-sympathetic failure including cardiovascular collapse due to loss of all preganglionic outflow*
- **Pan-sympathetic failure** is avoided because segments above **T10** (supplying the head, neck, and upper extremities) and the **adrenal medulla** (if T10-L2 is the primary resection) provide partial function.
- Cardiovascular collapse is unlikely because the **cardiac sympathetic nerves (T1-T4)** remain intact, maintaining heart rate and contractility.
*Minimal deficits due to complete bilateral compensation from contralateral sympathetic chain*
- Sympathetic innervation of the viscera is **bilateral**, but the **celiac and superior mesenteric ganglia** are midline structures; their resection leaves no contralateral alternative.
- Extensive **bilateral resection** of the chain segments at this level ensures profound deficits that cannot be compensated for by remaining neural pathways.
Sympathetic trunk anatomy US Medical PG Question 10: A 62-year-old man with atrial fibrillation undergoes catheter ablation of the pulmonary vein ostia. Post-procedure, he develops gastroparesis, but his cardiologist notes preserved heart rate variability and normal baroreceptor responses. Surgical anatomy review suggests the ablation may have damaged autonomic structures. Evaluate the most likely anatomical explanation for isolated gastric dysmotility with preserved cardiovascular autonomic function.
- A. Injury to the celiac ganglion via retrograde thermal conduction
- B. Direct damage to the enteric nervous system myenteric plexus
- C. Thermal injury to epicardial vagal branches specifically innervating the stomach via the gastric plexus (Correct Answer)
- D. Damage to the stellate ganglion causing isolated sympathetic denervation of the stomach
- E. Disruption of the entire vagal trunk causing pan-autonomic dysfunction
Sympathetic trunk anatomy Explanation: ***Thermal injury to epicardial vagal branches specifically innervating the stomach via the gastric plexus***
- The **vagus nerves** descend behind the heart and form the **esophageal plexus** near the **posterior wall of the left atrium**, making them vulnerable to energy during **pulmonary vein ablation**.
- Damage at this level can disrupt parasympathetic supply to the stomach, causing **gastroparesis**, while sparing the cardiac branches that already branched off superiorly, thereby preserving **heart rate variability**.
*Damage to the stellate ganglion causing isolated sympathetic denervation of the stomach*
- The **stellate ganglion** is located at the **C7-T1** level and supplies sympathetic fibers to the head, neck, and upper limbs; it is anatomically distant from the left atrium ablation site.
- Injury to this ganglion would present with **Horner Syndrome**, not isolated gastric dysmotility.
*Disruption of the entire vagal trunk causing pan-autonomic dysfunction*
- Complete **vagal trunk** damage would result in systemic symptoms, including significant changes in **heart rate variability** and loss of **baroreceptor reflex** sensitivity.
- The preservation of cardiovascular autonomic function indicates that the injury was localized and **distal to the cardiac branches**.
*Injury to the celiac ganglion via retrograde thermal conduction*
- The **celiac ganglion** is located in the **upper abdomen** around the root of the celiac trunk, making it an unlikely target for direct or retrograde thermal injury from the heart.
- This ganglion primarily handles **sympathetic output**; its injury would not typically cause the delayed gastric emptying characteristic of **vagal (parasympathetic) denervation**.
*Direct damage to the enteric nervous system myenteric plexus*
- The **myenteric (Auerbach’s) plexus** is located within the muscular layers of the **stomach wall**.
- Catheter ablation occurs in the **thoracic cavity** at the pulmonary veins; it cannot directly reach or damage the intrinsic nerves located within the abdominal viscus.
More Sympathetic trunk anatomy US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.