Parasympathetic cranial outflow US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Parasympathetic cranial outflow. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Parasympathetic cranial outflow US Medical PG Question 1: An otherwise healthy 58-year-old man comes to the physician because of a 1-year history of episodic coughing whenever he cleans his left ear. There is no history of hearing loss, tinnitus, or vertigo. Stimulating his left ear canal with a cotton swab triggers a bout of coughing. The physician informs him that these symptoms are caused by hypersensitivity of a cranial nerve. A peripheral lesion of this nerve is most likely to manifest with which of the following findings on physical examination?
- A. Ipsilateral sensorineural hearing loss
- B. Ipsilateral deviation of the tongue
- C. Inability to raise ipsilateral eyebrow
- D. Decreased secretion from ipsilateral sublingual gland
- E. Ipsilateral vocal cord palsy (Correct Answer)
Parasympathetic cranial outflow Explanation: ***Ipsilateral vocal cord palsy***
- The sensation in the external auditory canal that triggers a cough reflex is mediated by the **auricular branch of the vagus nerve (CN X)**, also known as Arnold's nerve.
- A peripheral lesion of the vagus nerve would most likely affect its motor functions, including the innervation of the **larynx**, leading to **ipsilateral vocal cord palsy** and hoarseness.
*Ipsilateral sensorineural hearing loss*
- Hearing loss is primarily associated with pathology of the **vestibulocochlear nerve (CN VIII)**, not the vagus nerve.
- The patient's presentation does not describe any auditory symptoms.
*Ipsilateral deviation of the tongue*
- Tongue deviation is a sign of compromise of the **hypoglossal nerve (CN XII)**, which controls the intrinsic and extrinsic muscles of the tongue.
- This is not a function of the vagus nerve.
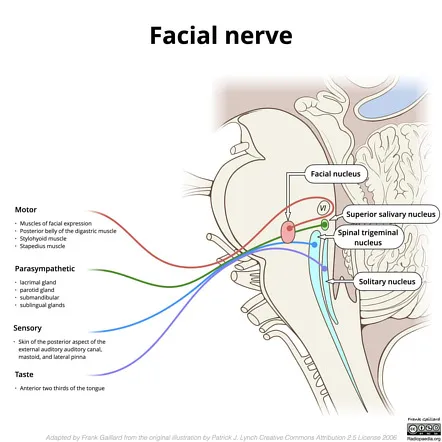
*Inability to raise ipsilateral eyebrow*
- The ability to raise the eyebrow is controlled by the **facial nerve (CN VII)**, which innervates the muscles of facial expression.
- Vagus nerve lesions do not typically present with facial weakness.
*Decreased secretion from ipsilateral sublingual gland*
- Secretion from the sublingual gland is controlled by the **facial nerve (CN VII)** via the submandibular ganglion.
- While the vagus nerve has autonomic functions, it does not directly control sublingual gland secretion.
Parasympathetic cranial outflow US Medical PG Question 2: A 55-year-old woman with a 1-year history of left-sided tinnitus is diagnosed with a tumor at the left cerebellopontine angle affecting the glossopharyngeal nerve. Sialometry shows decreased production of saliva from the left parotid gland. The finding on sialometry is best explained by a lesion of the nerve that is also responsible for which of the following?
- A. Protrusion of the tongue
- B. Afferent limb of the cough reflex
- C. Afferent limb of the gag reflex (Correct Answer)
- D. Equilibrium and balance
- E. Taste sensation of tip of the tongue
Parasympathetic cranial outflow Explanation: ***Afferent limb of the gag reflex***
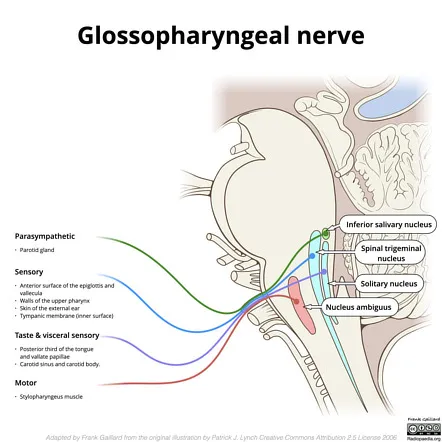
- The **glossopharyngeal nerve (CN IX)** provides **parasympathetic innervation** to the **parotid gland**, explaining the decreased saliva production on sialometry.
- CN IX is also responsible for the **afferent limb of the gag reflex** and taste sensation from the posterior one-third of the tongue.
*Protrusion of the tongue*
- **Protrusion of the tongue** is primarily controlled by the **hypoglossal nerve (CN XII)**.
- A lesion affecting the glossopharyngeal nerve would not directly impact the ability to protrude the tongue.
*Afferent limb of the cough reflex*
- The **afferent limb of the cough reflex** is primarily mediated by the **vagus nerve (CN X)**, which innervates the laryngeal and tracheobronchial mucosa.
- While there can be some overlap, the glossopharyngeal nerve is not the primary mediator for this reflex.
*Equilibrium and balance*
- **Equilibrium and balance** are primarily maintained by the **vestibulocochlear nerve (CN VIII)**, which is responsible for transmitting vestibular information.
- A lesion of the glossopharyngeal nerve would not primarily affect these functions, although cerebellopontine angle tumors can affect CN VIII.
*Taste sensation of tip of the tongue*
- **Taste sensation from the anterior two-thirds of the tongue** (including the tip) is conveyed by the **facial nerve (CN VII)** via the chorda tympani.
- The glossopharyngeal nerve (CN IX) provides taste sensation to the posterior one-third of the tongue.
Parasympathetic cranial outflow US Medical PG Question 3: A 50-year-old man presents to his primary care provider complaining of double vision and trouble seeing out of his right eye. His vision started worsening about 2 months ago and has slowly gotten worse. It is now severely affecting his quality of life. Past medical history is significant for poorly controlled hypertension and hyperlipidemia. He takes amlodipine, atorvastatin, and a baby aspirin every day. He smokes 2–3 cigarettes a day and drinks a glass of wine with dinner every night. Today, his blood pressure is 145/85 mm Hg, heart rate is 90/min, respiratory rate is 14/min, and temperature is 37.0°C (98.6°F). On physical exam, he appears pleasant and talkative. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. Examination of the eyes reveals a dilated right pupil that is positioned inferolateral with ptosis. An angiogram of the head and neck is performed and he is referred to a neurologist. The angiogram reveals a 1 cm berry aneurysm at the junction of the posterior communicating artery and the posterior cerebral artery compressing the oculomotor nerve. Which of the following statements best describes the mechanism behind the oculomotor findings seen in this patient?
- A. The parasympathetic nerve fibers of this patient’s eye are activated.
- B. The sympathetic nerve fibers of this patient’s eye are inhibited.
- C. The unopposed inferior oblique muscle rotates the eye downward.
- D. The unopposed superior oblique muscle rotates the eye downward. (Correct Answer)
- E. The unopposed medial rectus muscle rotates the eye in the lateral direction.
Parasympathetic cranial outflow Explanation: ***The unopposed superior oblique muscle rotates the eye downward.***
- The **oculomotor nerve** (CN III) innervates most extraocular muscles, including the **superior rectus, inferior rectus, medial rectus, and inferior oblique**, as well as the **levator palpebrae superioris** and **parasympathetic fibers** to the pupillary sphincter.
- With a complete **oculomotor nerve palsy**, the only remaining functional extraocular muscles are the **lateral rectus** (innervated by CN VI) and the **superior oblique** (innervated by CN IV), which causes the eye to be positioned **down and out** due to their unopposed actions.
*The parasympathetic nerve fibers of this patient’s eye are activated.*
- **Parasympathetic fibers** within the oculomotor nerve control **pupillary constriction** and lens accommodation.
- Compression of the oculomotor nerve, especially by an aneurysm, typically affects these superficial parasympathetic fibers first, leading to **pupillary dilation** (mydriasis) due to their impairment, not activation.
*The sympathetic nerve fibers of this patient’s eye are inhibited.*
- **Sympathetic innervation** to the eye controls pupillary dilation, eyelid elevation (via Müller's muscle), and sweat gland function.
- Inhibition of sympathetic fibers would lead to **miosis** (constricted pupil) and **ptosis** (drooping eyelid) as seen in **Horner's syndrome**, which is not the primary presentation of oculomotor nerve compression.
*The unopposed inferior oblique muscle rotates the eye downward.*
- The **inferior oblique muscle** elevates and abducts the eye; it is innervated by the **oculomotor nerve**.
- In an oculomotor nerve palsy, the inferior oblique muscle is **paralyzed**, thus it cannot exert any rotational force on the eye.
*The unopposed medial rectus muscle rotates the eye in the lateral direction.*
- The **medial rectus muscle** adducts the eye (moves it medially); it is innervated by the **oculomotor nerve**.
- In an oculomotor nerve palsy, the medial rectus is paralyzed, and its unopposed action would not cause lateral rotation; rather, the **lateral rectus** (innervated by CN VI) would cause the eye to deviate laterally.
Parasympathetic cranial outflow US Medical PG Question 4: A 26-year-old man comes to the physician for a follow-up examination. Two weeks ago, he was treated in the emergency department for head trauma after being hit by a bicycle while crossing the street. Neurological examination shows decreased taste on the right anterior tongue. This patient's condition is most likely caused by damage to a cranial nerve that is also responsible for which of the following?
- A. Facial sensation
- B. Parotid gland salivation
- C. Uvula movement
- D. Tongue protrusion
- E. Eyelid closure (Correct Answer)
Parasympathetic cranial outflow Explanation: ***Eyelid closure***
- The patient's **decreased taste on the right anterior tongue** indicates damage to the **facial nerve (CN VII)**, specifically the chorda tympani branch.
- The facial nerve is also responsible for innervating the muscles of **facial expression**, including the **orbicularis oculi** which closes the eyelid.
*Facial sensation*
- **Facial sensation** (touch, pain, temperature) is primarily mediated by the **trigeminal nerve (CN V)**, not the facial nerve.
- Damage to the trigeminal nerve would result in sensory deficits, not taste disturbances on the anterior tongue.
*Parotid gland salivation*
- **Parotid gland salivation** is primarily controlled by the **glossopharyngeal nerve (CN IX)** via the otic ganglion.
- The facial nerve (CN VII) innervates the **submandibular and sublingual glands**, but not the parotid gland.
*Uvula movement*
- **Uvula movement** and elevation of the soft palate are primarily controlled by the **vagus nerve (CN X)**, specifically through the pharyngeal plexus.
- Damage to CN X would typically lead to deviation of the uvula away from the paralyzed side.
*Tongue protrusion*
- **Tongue protrusion** (moving the tongue out) is the primary function of the **hypoglossal nerve (CN XII)**.
- Damage to the hypoglossal nerve would cause the tongue to deviate towards the lesioned side upon protrusion due to unopposed action of the healthy genioglossus muscle.
Parasympathetic cranial outflow US Medical PG Question 5: Which neurotransmitter is primarily responsible for parasympathetic effects on heart rate?
- A. Norepinephrine
- B. Dopamine
- C. Acetylcholine (Correct Answer)
- D. Epinephrine
Parasympathetic cranial outflow Explanation: ***Acetylcholine***
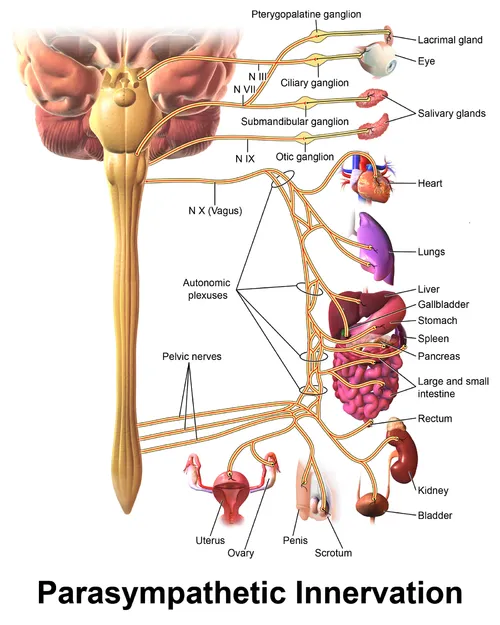
- **Acetylcholine** is the primary neurotransmitter released by postganglionic parasympathetic neurons.
- It acts on **muscarinic receptors** (M2 receptors) in the heart to decrease heart rate.
*Norepinephrine*
- **Norepinephrine** is primarily associated with the **sympathetic nervous system**, increasing heart rate and contractility.
- It acts on **beta-1 adrenergic receptors** in the heart.
*Dopamine*
- **Dopamine** is a precursor to norepinephrine and epinephrine, and primarily functions as a neurotransmitter in the **central nervous system** and in regulating renal blood flow.
- While it can have cardiac effects, it is not the primary neurotransmitter for parasympathetic actions on heart rate.
*Epinephrine*
- **Epinephrine** (adrenaline) is a hormone released by the adrenal medulla and a neurotransmitter in the sympathetic nervous system, causing an **increase in heart rate** and contractility.
- It works through **beta-1 adrenergic receptors**, antagonistic to parasympathetic effects.
Parasympathetic cranial outflow US Medical PG Question 6: An 87-year-old male presents to his neurologist for a follow-up visit. He is being followed for an inoperable tumor near his skull. He reports that he recently noticed that food has started to lose its taste. He also notes increasing difficulty with swallowing. He has a history of myocardial infarction, diabetes mellitus, hyperlipidemia, hypertension, and presbycusis. He takes aspirin, metoprolol, metformin, glyburide, atorvastatin, lisinopril, and hydrochlorothiazide. On examination, the patient is a frail-appearing male sitting in a wheelchair. He is oriented to person, place, and time. Gag reflex is absent on the right side. A taste evaluation is performed which demonstrates a decreased ability to detect sour and bitter substances on the right posterior tongue. The nerve responsible for this patient’s loss of taste sensation also has which of the following functions?
- A. Somatic sensory innervation to the roof of the pharynx
- B. Parasympathetic innervation to the trachea
- C. Somatic sensory innervation to the lower lip
- D. Parasympathetic innervation to the parotid gland (Correct Answer)
- E. Parasympathetic innervation to the submandibular gland
Parasympathetic cranial outflow Explanation: ***Parasympathetic innervation to the parotid gland***
- The patient's symptoms, including loss of taste on the **right posterior tongue**, difficulty swallowing, and an absent gag reflex, point to an issue with the **glossopharyngeal nerve (CN IX)**.
- The glossopharyngeal nerve provides **parasympathetic innervation to the parotid gland** via the otic ganglion, stimulating saliva production.
*Somatic sensory innervation to the roof of the pharynx*
- The glossopharyngeal nerve (CN IX) does provide somatic sensory innervation to the pharynx, but specifically the **posterior 1/3 of the tongue**, tonsils, and part of the pharynx, not primarily the roof.
- While related to the pharynx, this option is not the most precise or unique function associated with the primary nerve implicated here.
*Parasympathetic innervation to the trachea*
- **Parasympathetic innervation to the trachea** is primarily mediated by the **vagus nerve (CN X)**, which innervates the smooth muscle and glands of the trachea and bronchi.
- The glossopharyngeal nerve (CN IX) does not have a direct role in tracheal innervation.
*Somatic sensory innervation to the lower lip*
- **Somatic sensory innervation to the lower lip** is primarily provided by the **mental nerve**, a branch of the **trigeminal nerve (CN V)**.
- The glossopharyngeal nerve (CN IX) is not involved in sensory innervation of the lower lip.
*Parasympathetic innervation to the submandibular gland*
- **Parasympathetic innervation to the submandibular and sublingual glands** is provided by the **facial nerve (CN VII)** via the submandibular ganglion.
- This function is distinct from the glossopharyngeal nerve's role in innervating the parotid gland.
Parasympathetic cranial outflow US Medical PG Question 7: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Parasympathetic cranial outflow Explanation: ***Glossopharyngeal***
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
Parasympathetic cranial outflow US Medical PG Question 8: A 26-year-old man is brought to the emergency department by ambulance after being involved in a motor vehicle collision. He does not open his eyes on command or respond to verbal cues. A CT scan of the head shows a hyperdense fluid collection in the right medial temporal lobe with medial displacement of the uncus and parahippocampal gyrus of the temporal lobe. Which of the following cranial nerves is most likely to be injured as a result of this patient's lesion?
- A. Vagus
- B. Facial
- C. Oculomotor (Correct Answer)
- D. Abducens
- E. Trigeminal
Parasympathetic cranial outflow Explanation: ***Oculomotor***
- The description of **medial displacement of the uncus and parahippocampal gyrus** (uncus herniation) compresses the **oculomotor nerve (CN III)** as it passes between the posterior cerebral and superior cerebellar arteries.
- Compression of the oculomotor nerve leads to a **dilated pupil** (due to parasympathetic fiber involvement) and **down-and-out deviation of the eye** (due to paralysis of extraocular muscles it innervates).
*Vagus*
- The vagus nerve (CN X) is deep within the skull and brainstem, far from the temporal lobe, and is not directly affected by uncal herniation.
- Injury to the vagus nerve typically presents with dysphagia, hoarseness, or cardiac arrhythmias, symptoms not indicated here.
*Facial*
- The facial nerve (CN VII) exits the brainstem at the pontomedullary junction and is located more superiorly and laterally than the structures involved in uncal herniation.
- Damage to the facial nerve causes facial muscle weakness or paralysis, which is not the primary concern with uncal herniation.
*Abducens*
- The abducens nerve (CN VI) is a long, slender nerve that can be affected by **generalized increases in intracranial pressure**, but is less commonly directly compressed by an uncal herniation itself.
- Injury to the abducens nerve causes **lateral rectus muscle paralysis**, leading to medial deviation of the eye, whereas uncal herniation typically affects the oculomotor nerve.
*Trigeminal*
- The trigeminal nerve (CN V) exits the pons and is located superior to the tentorial notch and medial temporal lobe, making it unlikely to be directly compressed by uncal herniation.
- Injury to the trigeminal nerve causes sensory loss in the face or weakness of the muscles of mastication, which are not consistent with the described lesion.
Parasympathetic cranial outflow US Medical PG Question 9: A 29-year-old man presents to the emergency room with facial weakness. He first noticed that he was having trouble smiling normally while at dinner with friends the night before. He also noticed that his food had less taste than usual during the dinner. He woke up on the day of presentation with a complete inability to move the right side of his face. He recently returned from an extended camping trip in the Appalachian Mountains, but he did not find any tick bites following the camping trip. His past medical history is notable for Achilles tendonitis and carpal tunnel syndrome. He works as a computer programmer. He smokes marijuana occasionally but does not smoke cigarettes. His temperature is 98.6°F (37°C), blood pressure is 120/75 mmHg, pulse is 80/min, and respirations are 18/min. On exam, he is well-appearing in no acute distress. There is loss of facial wrinkles along the forehead, eyelids, and nasolabial folds. He is unable to completely close his right eye, raise his eyebrows, or smile with the right side of his mouth. Sensation is intact to light touch along the forehead, maxilla, and mandible bilaterally. Where is the most likely source of this patient’s lesion?
- A. Superior orbital fissure
- B. Petrotympanic fissure
- C. Inferior orbital fissure
- D. Dorsal frontal lobe
- E. Stylomastoid foramen (Correct Answer)
Parasympathetic cranial outflow Explanation: ***Stylomastoid foramen***
- The patient presents with classic signs of **Bell's palsy**, characterized by unilateral **facial weakness affecting both the upper and lower face**, including loss of forehead wrinkles, inability to close the eye, and loss of nasolabial folds.
- The **stylomastoid foramen** is the exit point of the **facial nerve (CN VII)** from the skull, and inflammation or compression at this site is the most common cause of idiopathic facial nerve paralysis (Bell's palsy).
*Superior orbital fissure*
- Lesions in the **superior orbital fissure** would primarily affect cranial nerves **III, IV, V1, and VI**, leading to symptoms like ophthalmoplegia, ptosis, and sensory loss in the V1 distribution of the face, not a facial nerve palsy.
- While it is a bony canal, it is not the primary exit for the facial nerve.
*Petrotympanic fissure*
- The **petrotympanic fissure** transmits the **chorda tympani nerve**, which carries taste sensation from the anterior two-thirds of the tongue and parasympathetic fibers to the submandibular and sublingual glands.
- A lesion here would cause **loss of taste** and potentially dry mouth, but would not typically explain the extensive motor deficits of the entire ipsilateral face as seen in this patient, which indicates a more proximal or complete facial nerve involvement.
*Inferior orbital fissure*
- The **inferior orbital fissure** transmits the **maxillary nerve (V2)**, the zygomatic nerve, and branches of the inferior ophthalmic vein, affecting sensation to the mid-face.
- Damage here would result in **sensory deficits in the V2 distribution** and potentially orbital symptoms, not motor weakness of the facial muscles.
*Dorsal frontal lobe*
- A lesion in the **dorsal frontal lobe**, specifically involving the **motor cortex**, would cause contralateral facial weakness. However, it would typically spare the forehead and eyelid muscles due to bilateral cortical innervation of the upper facial muscles.
- The patient's presentation of **forehead and entire facial weakness** is characteristic of a **lower motor neuron lesion** of the facial nerve, not a central (upper motor neuron) lesion.
Parasympathetic cranial outflow US Medical PG Question 10: A 27-year-old man comes to the physician because of a 1-day history of right-sided facial weakness and sound intolerance. Three days ago, he hit the right side of his head in a motor vehicle collision. He neither lost consciousness nor sought medical attention. Physical examination shows drooping of the mouth on the right side. Sensation over the face is not impaired. Impedance audiometry shows an absence of the acoustic reflex in the right ear. Which of the following muscles is most likely paralyzed in this patient?
- A. Anterior belly of the digastric
- B. Stylopharyngeus
- C. Cricothyroid
- D. Tensor tympani
- E. Stylohyoid (Correct Answer)
Parasympathetic cranial outflow Explanation: ***Stylohyoid***
- The patient presents with **facial nerve (CN VII) injury** following head trauma, evidenced by **facial weakness** and **hyperacusis** (sound intolerance).
- The **absent acoustic reflex** indicates paralysis of the **stapedius muscle** (the primary muscle responsible for the acoustic reflex and sound dampening).
- Among the options provided, **stylohyoid** is the only muscle innervated by the **facial nerve (CN VII)**, making it the correct answer in this context.
- The stylohyoid is innervated by the **nerve to stylohyoid**, a branch of CN VII.
*Anterior belly of the digastric*
- The **anterior belly of the digastric** is innervated by the **mylohyoid nerve**, a branch of the **trigeminal nerve (CN V3)**.
- This would not be affected in facial nerve injury.
*Stylopharyngeus*
- The **stylopharyngeus muscle** is innervated by the **glossopharyngeal nerve (CN IX)**.
- Damage would cause **dysphagia** and **loss of taste** on the posterior third of the tongue, not facial weakness or hyperacusis.
*Cricothyroid*
- The **cricothyroid muscle** is innervated by the **external branch of the superior laryngeal nerve** (from **vagus nerve, CN X**).
- Its paralysis causes **voice changes** and difficulty with high-pitched phonation, not facial nerve symptoms.
*Tensor tympani*
- The **tensor tympani muscle** is innervated by the **nerve to tensor tympani**, a branch of the **trigeminal nerve (V3)**.
- Although it dampens sound, it would not be affected in facial nerve injury; the **stapedius muscle** (CN VII) is responsible for the acoustic reflex and hyperacusis when paralyzed.
More Parasympathetic cranial outflow US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.