Autonomic plexuses US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autonomic plexuses. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autonomic plexuses US Medical PG Question 1: A 50-year-old male is brought to the dermatologist's office with complaints of a pigmented lesion. The lesion is uniformly dark with clean borders and no asymmetry and has been increasing in size over the past two weeks. He works in construction and spends large portions of his day outside. The dermatologist believes that this mole should be biopsied. To prepare the patient for the biopsy, the dermatologist injects a small amount of lidocaine into the skin around the lesion. Which of the following nerve functions would be the last to be blocked by the lidocaine?
- A. Pain
- B. Touch
- C. Temperature
- D. Sympathetic stimulation
- E. Pressure (Correct Answer)
Autonomic plexuses Explanation: ***Pressure***
- **Pressure** sensation is mediated by **Aβ fibers**, which are relatively **larger** and **myelinated**, making them more resistant to local anesthetic blockade.
- Nerve fibers are blocked in a specific order, typically starting with smaller, unmyelinated fibers and ending with larger, myelinated fibers.
*Pain*
- **Pain** sensation is primarily carried by **unmyelinated C fibers** and **small myelinated Aδ fibers**, which are among the **first to be blocked** by local anesthetics.
- These fibers have a **high surface-to-volume ratio**, making them more susceptible to the action of lidocaine.
*Touch*
- **Touch** sensation is mediated by a mix of **Aβ and Aδ fibers**; light touch is typically blocked relatively early due to the involvement of smaller fibers.
- However, **crude touch** often persists longer than pain and temperature but is usually blocked before pressure.
*Temperature*
- **Temperature** sensation is primarily carried by **Aδ and C fibers**, making it one of the **earliest sensations to be blocked** by local anesthetic.
- These fibers are generally small and have high sensitivity to local anesthetic agents.
*Sympathetic stimulation*
- **Sympathetic nerve fibers** are typically **small, unmyelinated C fibers** and are generally the **first to be blocked** by local anesthetics.
- This early blockade can lead to **vasodilation** in the area due to the loss of sympathetic tone.
Autonomic plexuses US Medical PG Question 2: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Autonomic plexuses Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
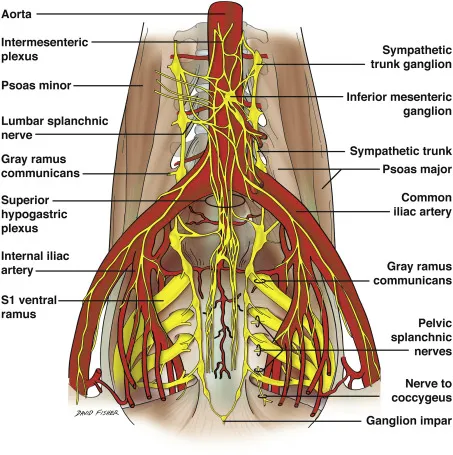
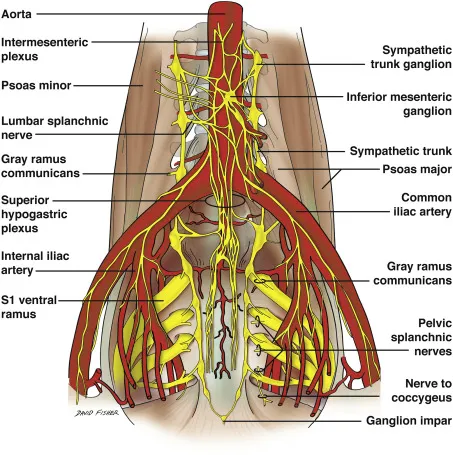
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Autonomic plexuses US Medical PG Question 3: A 16-year-old boy presents to the emergency department with abdominal pain and tenderness. The pain began approximately 2 days ago in the area just above his umbilicus and was crampy in nature. Earlier this morning, the pain moved laterally to his right lower abdomen. At that time, the pain in the right lower quadrant became severe and constant and woke him up from sleep. He decided to come to the hospital. The patient is nauseous and had a low-grade fever of 37.8°C (100.1°F). Other vitals are normal. Upon physical examination, the patient has rebound tenderness but a negative psoas sign while the remaining areas of his abdomen are non-tender. His rectal exam is normal. Laboratory tests show a white cell count of 15,000/mm3. Urinalysis and other laboratory findings were negative. What conclusion can be drawn about the nerves involved in the transmission of this patient’s pain during the physical exam?
- A. His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.
- B. His pain is transmitted by somatic afferent nerve fibers located in the right flank.
- C. His pain is transmitted by the pelvic nerves.
- D. His pain is transmitted by right somatic nerve fibers. (Correct Answer)
- E. His pain is mainly transmitted by the right splanchnic nerve.
Autonomic plexuses Explanation: ***His pain is transmitted by right somatic nerve fibers.***
- The **migration of pain from the periumbilical region to the right lower quadrant** and becoming **severe and constant** indicates parietal peritoneal irritation.
- **Somatic nerve fibers** innervate the parietal peritoneum and are responsible for transmitting **sharp, localized pain** typically associated with appendicitis in the right lower quadrant.
*His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.*
- While **visceral pain** from the initial appendiceal inflammation can be perceived bilaterally in the periumbilical region due to **bilateral innervation of visceral organs**, the **localized right lower quadrant pain** signifies involvement of **unilaterally innervated parietal peritoneum**.
- The physical exam findings of **rebound tenderness** strongly suggest **localized peritoneal inflammation**, which is transmitted by **unilateral somatic nerves** at the site of inflammation, not bilaterally across the abdomen.
*His pain is transmitted by somatic afferent nerve fibers located in the right flank.*
- The **right flank** refers to the lateral aspect of the abdomen, while the pain is specifically localized to the **right lower quadrant**.
- Although somatic nerves are involved, stating "right flank" is **too broad and imprecise** given the very specific localization of the pain to the right lower quadrant where the inflamed appendix is typically situated.
*His pain is transmitted by the pelvic nerves.*
- **Pelvic nerves** primarily carry parasympathetic fibers and visceral afferent fibers from pelvic organs, not the somatic pain from the parietal peritoneum in the right lower quadrant.
- Pain from **pelvic organs** or **pelvic peritoneum** would be transmitted via these nerves, but the localized pain here is distinctly higher than typical pelvic organ pain.
*His pain is mainly transmitted by the right splanchnic nerve.*
- **Splanchnic nerves** primarily carry **visceral afferent fibers** responsible for the dull, poorly localized, initial periumbilical pain of appendicitis.
- They do not transmit the **sharp, well-localized somatic pain** associated with parietal peritoneal irritation, which is characteristic of the pain migrating to the right lower quadrant.
Autonomic plexuses US Medical PG Question 4: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Autonomic plexuses Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Autonomic plexuses US Medical PG Question 5: A 65-year-old man presents to the emergency department with vague, constant abdominal pain, and worsening shortness of breath for the past several hours. He has baseline shortness of breath and requires 2–3 pillows to sleep at night. He often wakes up because of shortness of breath. Past medical history includes congestive heart failure, diabetes, hypertension, and hyperlipidemia. He regularly takes lisinopril, metoprolol, atorvastatin, and metformin. His temperature is 37.0°C (98.6°F), respiratory rate 25/min, pulse 67/min, and blood pressure 98/82 mm Hg. On physical examination, he has bilateral crackles over both lung bases and a diffusely tender abdomen. His subjective complaint of abdominal pain is more severe than the observed tenderness on examination. Which of the following vessels is involved in the disease affecting this patient?
- A. Left anterior descending
- B. Celiac artery and superior mesenteric artery (Correct Answer)
- C. Left colic artery
- D. Right coronary artery
- E. Meandering mesenteric artery
Autonomic plexuses Explanation: **Celiac artery and superior mesenteric artery**
- The patient's presentation with **vague, constant abdominal pain** out of proportion to physical exam findings (**abdominal pain more severe than tenderness**) in the setting of **congestive heart failure** and **hypotension** is highly suggestive of **non-occlusive mesenteric ischemia (NOMI)**.
- NOMI results from **splanchnic vasoconstriction** leading to hypoperfusion of the bowel, primarily affecting the territories supplied by the **celiac artery** and **superior mesenteric artery**, which supply the foregut and midgut, respectively.
*Left anterior descending*
- The left anterior descending (LAD) artery primarily supplies the **left ventricle** and interventricular septum.
- Occlusion of the LAD typically causes a **myocardial infarction** with chest pain, EKG changes, and elevated cardiac enzymes, which is not the primary presentation here, although a degree of cardiac compromise exacerbates the NOMI.
*Left colic artery*
- The left colic artery is a branch of the **inferior mesenteric artery** and supplies portions of the **descending colon**.
- While bowel ischemia can affect this region, NOMI, a more widespread condition, is unlikely to be isolated to the left colic artery distribution, and the patient's symptoms are more consistent with multi-vessel involvement.
*Right coronary artery*
- The right coronary artery (RCA) supplies the **right ventricle**, inferior wall of the left ventricle, and often the **SA and AV nodes**.
- RCA occlusion typically leads to **inferior wall myocardial infarction** and can cause bradyarrhythmias, but it would not directly cause the described abdominal pain and out-of-proportion findings.
*Meandering mesenteric artery*
- The meandering mesenteric artery is an anatomical variant, an **anastomotic connection** between the superior and inferior mesenteric arteries.
- While it can be a source of collateral flow, it is not a primary vessel targeted in the pathogenesis of NOMI, which affects the main mesenteric arteries due to global hypoperfusion.
Autonomic plexuses US Medical PG Question 6: Which neurotransmitter is primarily responsible for parasympathetic effects on heart rate?
- A. Norepinephrine
- B. Dopamine
- C. Acetylcholine (Correct Answer)
- D. Epinephrine
Autonomic plexuses Explanation: ***Acetylcholine***
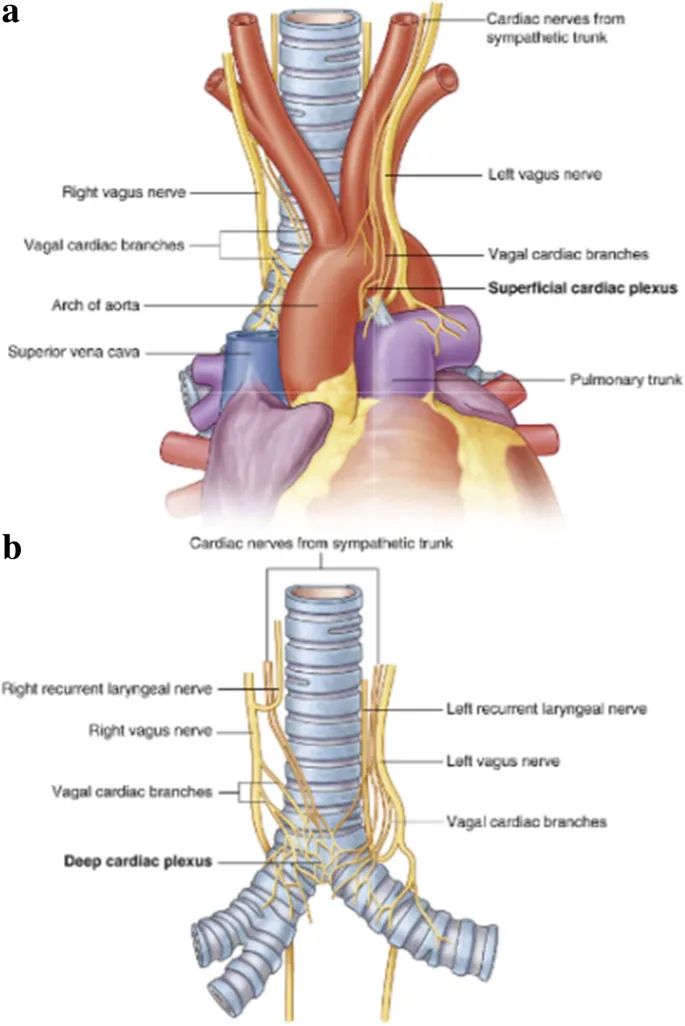
- **Acetylcholine** is the primary neurotransmitter released by postganglionic parasympathetic neurons.
- It acts on **muscarinic receptors** (M2 receptors) in the heart to decrease heart rate.
*Norepinephrine*
- **Norepinephrine** is primarily associated with the **sympathetic nervous system**, increasing heart rate and contractility.
- It acts on **beta-1 adrenergic receptors** in the heart.
*Dopamine*
- **Dopamine** is a precursor to norepinephrine and epinephrine, and primarily functions as a neurotransmitter in the **central nervous system** and in regulating renal blood flow.
- While it can have cardiac effects, it is not the primary neurotransmitter for parasympathetic actions on heart rate.
*Epinephrine*
- **Epinephrine** (adrenaline) is a hormone released by the adrenal medulla and a neurotransmitter in the sympathetic nervous system, causing an **increase in heart rate** and contractility.
- It works through **beta-1 adrenergic receptors**, antagonistic to parasympathetic effects.
Autonomic plexuses US Medical PG Question 7: During a physical examination, a physician tests the strength of hip adduction against resistance. Which of the following nerves innervates the primary muscles responsible for this action?
- A. Sciatic nerve
- B. Superior gluteal nerve
- C. Femoral nerve
- D. Obturator nerve (Correct Answer)
Autonomic plexuses Explanation: ***Obturator nerve***
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh, including the adductor longus, adductor brevis, adductor magnus (adductor part), gracilis, and pectineus (variable innervation).
- These muscles are responsible for **adducting the hip**, which is the action tested when a physician checks hip adduction strength against resistance.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and all muscles below the knee.
- It does not significantly contribute to the innervation of the primary hip adductors.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles.
- These muscles are primarily involved in **hip abduction** and medial rotation, not adduction.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) and the sartorius.
- Its primary actions are **knee extension** and hip flexion, with no direct role in hip adduction.
Autonomic plexuses US Medical PG Question 8: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Autonomic plexuses Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Autonomic plexuses US Medical PG Question 9: A 26-year-old woman presents to the obstetrics ward to deliver her baby. The obstetrician establishes a pudendal nerve block via intravaginal injection of lidocaine near the tip of the ischial spine. From which of the following nerve roots does the pudendal nerve originate?
- A. L4-L5
- B. S2-S4 (Correct Answer)
- C. L3-L4
- D. L5-S2
- E. L5-S1
Autonomic plexuses Explanation: ***S2-S4***
- The **pudendal nerve** originates from the **sacral plexus**, specifically from the ventral rami of spinal nerves **S2, S3, and S4**.
- Its origin from these segments is crucial for its function in innervating structures of the **perineum**, **external genitalia**, and the **anal and urethral sphincters**, making it highly relevant for procedures like **pudendal nerve blocks** during childbirth.
*L4-L5*
- Nerve roots **L4-L5** contribute significantly to the **lumbar plexus** and subsequently to nerves like the **femoral nerve** and portions of the **sciatic nerve**.
- These roots are primarily involved in innervating the **lower limbs** (e.g., quadriceps, tibialis anterior) and are not the primary origin of the pudendal nerve.
*L3-L4*
- The **L3-L4** nerve roots are also part of the **lumbar plexus**, chiefly contributing to the **femoral nerve**.
- They are essential for motor innervation of the **anterior thigh muscles** and sensation in this area, distinct from the pudendal nerve's role in the perineum.
*L5-S2*
- While **S2** is part of the pudendal nerve's origin, the inclusion of **L5** and **S1** primarily characterizes the origin of the **sciatic nerve** (which is formed by L4-S3) and its branches, such as the common fibular and tibial nerves.
- These roots are primarily concerned with the **posterior thigh** and **leg innervation**, not the perineum, which differentiates it from the pudendal nerve.
*L5-S1*
- The nerve roots **L5-S1** are key components of the **lumbosacral plexus** and contribute significantly to the **sciatic nerve**, particularly its innervation of the **hamstrings** and certain lower leg muscles.
- This origin does not align with the known roots of the **pudendal nerve** which stems from S2-S4.
Autonomic plexuses US Medical PG Question 10: An otherwise healthy 58-year-old man comes to the physician because of a 1-year history of episodic coughing whenever he cleans his left ear. There is no history of hearing loss, tinnitus, or vertigo. Stimulating his left ear canal with a cotton swab triggers a bout of coughing. The physician informs him that these symptoms are caused by hypersensitivity of a cranial nerve. A peripheral lesion of this nerve is most likely to manifest with which of the following findings on physical examination?
- A. Ipsilateral sensorineural hearing loss
- B. Ipsilateral deviation of the tongue
- C. Inability to raise ipsilateral eyebrow
- D. Decreased secretion from ipsilateral sublingual gland
- E. Ipsilateral vocal cord palsy (Correct Answer)
Autonomic plexuses Explanation: ***Ipsilateral vocal cord palsy***
- The sensation in the external auditory canal that triggers a cough reflex is mediated by the **auricular branch of the vagus nerve (CN X)**, also known as Arnold's nerve.
- A peripheral lesion of the vagus nerve would most likely affect its motor functions, including the innervation of the **larynx**, leading to **ipsilateral vocal cord palsy** and hoarseness.
*Ipsilateral sensorineural hearing loss*
- Hearing loss is primarily associated with pathology of the **vestibulocochlear nerve (CN VIII)**, not the vagus nerve.
- The patient's presentation does not describe any auditory symptoms.
*Ipsilateral deviation of the tongue*
- Tongue deviation is a sign of compromise of the **hypoglossal nerve (CN XII)**, which controls the intrinsic and extrinsic muscles of the tongue.
- This is not a function of the vagus nerve.
*Inability to raise ipsilateral eyebrow*
- The ability to raise the eyebrow is controlled by the **facial nerve (CN VII)**, which innervates the muscles of facial expression.
- Vagus nerve lesions do not typically present with facial weakness.
*Decreased secretion from ipsilateral sublingual gland*
- Secretion from the sublingual gland is controlled by the **facial nerve (CN VII)** via the submandibular ganglion.
- While the vagus nerve has autonomic functions, it does not directly control sublingual gland secretion.
More Autonomic plexuses US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.