Autonomic innervation of abdominal organs US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autonomic innervation of abdominal organs. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autonomic innervation of abdominal organs US Medical PG Question 1: A patient demonstrates decreased gastric acid secretion after vagotomy. Which cell type is directly affected by vagal denervation?
- A. Parietal cells (Correct Answer)
- B. ECL cells
- C. Chief cells
- D. G cells
Autonomic innervation of abdominal organs Explanation: ***Parietal cells***
- **Parietal cells** are responsible for secreting **hydrochloric acid (HCl)** in the stomach.
- They receive **direct vagal innervation** and vagal stimulation directly promotes acid secretion through the neurotransmitter **acetylcholine (ACh)** acting on M3 muscarinic receptors.
- After vagotomy, parietal cells lose this direct cholinergic stimulation, resulting in **decreased gastric acid secretion**.
*ECL cells*
- **Enterochromaffin-like (ECL) cells** produce and release **histamine**, which then acts on parietal cells via H2 receptors to stimulate acid secretion.
- ECL cells are also **directly innervated by vagal efferents** and release histamine in response to acetylcholine.
- However, ECL cells do not themselves secrete acid; they stimulate parietal cells to do so, making them indirectly involved in acid production.
*Chief cells*
- **Chief cells** primarily secrete **pepsinogen**, the inactive precursor of pepsin, and **gastric lipase**.
- While vagal stimulation does promote pepsinogen secretion, these cells are not responsible for gastric acid production.
*G cells*
- **G cells** secrete **gastrin**, a hormone that stimulates both parietal cells (directly) and ECL cells (indirectly) to increase acid secretion.
- Vagal stimulation enhances gastrin release, so vagotomy would reduce gastrin levels, but G cells themselves do not produce acid.
Autonomic innervation of abdominal organs US Medical PG Question 2: A scientist is studying the mechanism by which the gastrointestinal system coordinates the process of food digestion. Specifically, she is interested in how distension of the lower esophagus by a bolus of food changes responses in the downstream segments of the digestive system. She observes that there is a resulting relaxation and opening of the lower esophageal (cardiac) sphincter after the introduction of a food bolus. She also observes a simultaneous relaxation of the orad stomach during this time. Which of the following substances is most likely involved in the process being observed here?
- A. Neuropeptide-Y
- B. Secretin
- C. Ghrelin
- D. Vasoactive intestinal polypeptide (Correct Answer)
- E. Motilin
Autonomic innervation of abdominal organs Explanation: ***Vasoactive intestinal polypeptide***
- **VIP (Vasoactive intestinal polypeptide)** is a neuropeptide that mediates **relaxation** of the **smooth muscle** in the gastrointestinal tract, including the **lower esophageal sphincter** and the **orad stomach**, facilitating the passage of food.
- This relaxation is part of the **receptive relaxation** process, allowing the stomach to accommodate food without a significant increase in intragastric pressure.
*Neuropeptide-Y*
- **Neuropeptide-Y (NPY)** is primarily involved in stimulating **food intake** and **reducing energy expenditure**, acting as an orexigenic peptide.
- It does not directly mediate the relaxation of the **lower esophageal sphincter** or **orad stomach** in response to food bolus distension.
*Secretin*
- **Secretin** is a hormone released in response to **acid in the duodenum** and primarily stimulates the pancreas to release **bicarbonate-rich fluid**.
- Its main role is to neutralize stomach acid, not to mediate sphincter relaxation or stomach accommodation.
*Ghrelin*
- **Ghrelin** is known as the "**hunger hormone**" and primarily stimulates **appetite** and **growth hormone release**.
- It does not play a direct role in the relaxation of the **lower esophageal sphincter** or **orad stomach** during swallowing.
*Motilin*
- **Motilin** promotes **gastric and intestinal motility** during the **interdigestive phase**, responsible for the migrating motor complex (MMC).
- Its actions are generally prokinetic, rather than causing relaxation of the upper GI tract in response to a food bolus.
Autonomic innervation of abdominal organs US Medical PG Question 3: A 66-year-old man is brought to the emergency department after a motor vehicle accident. The patient was a restrained passenger in a car that was struck on the passenger side while crossing an intersection. In the emergency department, he is alert and complaining of abdominal pain. He has a history of hyperlipidemia, gastroesophageal reflux disease, chronic kidney disease, and perforated appendicitis for which he received an interval appendectomy four years ago. His home medications include rosuvastatin and lansoprazole. His temperature is 99.2°F (37.3°C), blood pressure is 120/87 mmHg, pulse is 96/min, and respirations are 20/min. He has full breath sounds bilaterally. He is tender to palpation over the left 9th rib and the epigastrium. He is moving all four extremities. His FAST exam reveals fluid in Morrison's pouch.
This patient is most likely to have which of the following additional signs or symptoms?
- A. Pain radiating to the back
- B. Gross hematuria
- C. Muffled heart sounds
- D. Free air on chest radiograph
- E. Shoulder pain (Correct Answer)
Autonomic innervation of abdominal organs Explanation: ***Shoulder pain***
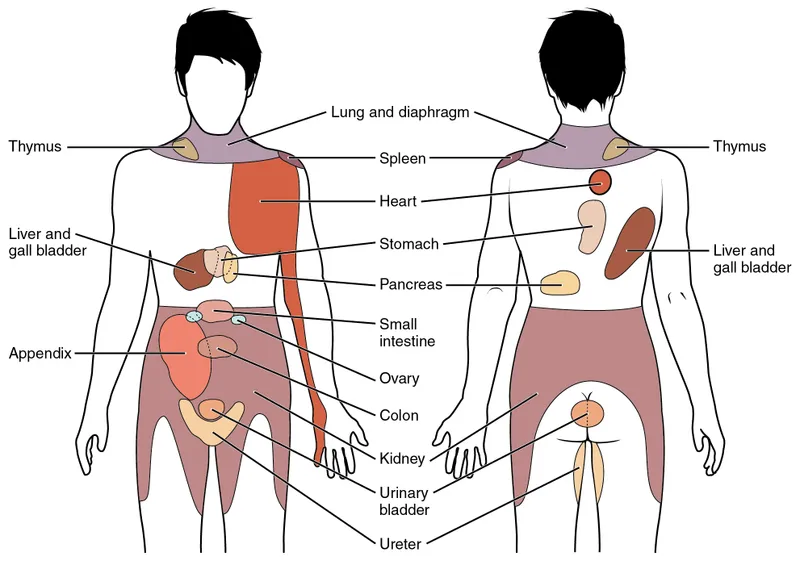
- The presence of **fluid in Morrison's pouch** (hepatorenal recess) on FAST exam indicates **intra-abdominal bleeding**, likely from a liver or spleen injury.
- **Diaphragmatic irritation** due to intra-abdominal hemorrhage often manifests as referred **shoulder pain** (Kehr's sign), especially on the left side with splenic injury or right side with liver injury.
*Pain radiating to the back*
- While pancreatic injury can cause pain radiating to the back, the primary finding of **fluid in Morrison's pouch** points towards hemoperitoneum, less specifically to pancreatic trauma.
- Significant pancreatic injury would likely involve more severe abdominal tenderness and potentially elevated **amylase/lipase**, which are not mentioned here.
*Gross hematuria*
- **Gross hematuria** would suggest a **renal or urologic injury**, but the patient's primary finding is intra-abdominal fluid in Morrison's pouch, which is more indicative of solid organ injury like the liver or spleen.
- Though concurrent injuries are possible in trauma, hepatorenal fluid points specifically to **hemoperitoneum**, not necessarily kidney damage.
*Muffled heart sounds*
- **Muffled heart sounds** are a component of **Beck's triad** (along with hypotension and jugular venous distension), indicative of **cardiac tamponade** due to fluid around the heart.
- There is no clinical information in the stem suggestive of cardiac injury or tamponade; the fluid is specifically mentioned in the abdomen.
*Free air on chest radiograph*
- **Free air on chest radiograph** (pneumoperitoneum) indicates a **perforated hollow viscus**, such as the bowel or stomach.
- The FAST exam finding of fluid in Morrison's pouch is characteristic of **hemoperitoneum** from a solid organ injury, not free air from a perforation.
Autonomic innervation of abdominal organs US Medical PG Question 4: A 42-year-old woman presents to the emergency department complaining of abdominal pain, nausea, and vomiting for the last 4 hours. She says that symptoms onset right after she had 2 generous portions of pizza. She notes that she had prior similar episodes which resolved spontaneously within an hour. However, the pain today has persisted for 5 hours and is much more severe. She says the pain is located in the right upper quadrant of her abdomen and radiates to her upper back. She describes the pain as dull and cramping. She has had hypertension for the past 10 years, managed medically. Her vital signs are a blood pressure of 148/96 mm Hg, a pulse of 108/min, a respiratory rate of 18/min, and a temperature of 37.7°C (99.9°F). Her BMI is 28 kg/m2. On physical examination, the patient appears uncomfortable and is clutching her abdomen in pain. Abdominal exam reveals severe tenderness to palpation in the right upper quadrant with guarding. A positive Murphy’s sign is present. Her serum chemistry levels, including amylase, lipase, bilirubin, and liver function tests and urinalysis are normal. Urine hCG level is < 0.5 IU/L. Abdominal ultrasound reveals a large stone lodged in the neck of the gallbladder. Which of the following is the most likely pathway for referred pain in this patient?
- A. Right thoraco-abdominal intercostal nerves
- B. The phrenic nerve
- C. Greater splanchnic nerves to the spinal cord (Correct Answer)
- D. Left greater splanchnic nerve
- E. The pain endings of the visceral peritoneum
Autonomic innervation of abdominal organs Explanation: ***Greater splanchnic nerves to the spinal cord***
- The **greater splanchnic nerves** (T5-T9) carry **visceral afferent fibers** from the gallbladder, transmitting pain to the spinal cord segments corresponding to the upper back (T5-T9).
- This explains the **dull, cramping right upper quadrant pain** that **radiates to the upper back**, characteristic of visceral pain from the gallbladder.
*Right thoraco-abdominal intercostal nerves*
- These nerves primarily innervate the **parietal peritoneum** and abdominal wall, responsible for sharp, localized somatic pain.
- While they could be involved in localized pain, they don't typically account for the **referred dull, cramping pain to the back** originating from a visceral organ like the gallbladder.
*The phrenic nerve*
- The **phrenic nerve** innervates the diaphragm and carries pain from the **diaphragmatic pleura and peritoneum**, often resulting in referred pain to the shoulder tip.
- Gallbladder pain can sometimes irritate the diaphragm, but the primary referral to the **upper back** is more characteristic of splanchnic nerve involvement.
*Left greater splanchnic nerve*
- The **left greater splanchnic nerve** primarily innervates organs on the left side of the upper abdomen, such as the stomach and spleen.
- Since the gallbladder is on the **right side**, its afferent pain signals travel via the right greater splanchnic nerves.
*The pain endings of the visceral peritoneum*
- The **visceral peritoneum** itself is generally insensitive to pain from cutting or burning; it senses stretch and inflammation.
- However, the pain signals from the stretched or inflamed gallbladder are transmitted via **visceral afferent fibers within the splanchnic nerves**, not directly by the visceral peritoneum's own pain endings.
Autonomic innervation of abdominal organs US Medical PG Question 5: A 2-year-old boy is brought in to his pediatrician for a routine checkup. The parents mention that the child has been developing appropriately, although they have been noticing that the child appears to have chronic constipation. The parents report that their child does not routinely have daily bowel movements, and they have noticed that his abdomen has become more distended recently. In the past, they report that the patient was also delayed in passing meconium, but this was not further worked up. On exam, his temperature is 98.6°F (37.0°C), blood pressure is 110/68 mmHg, pulse is 74/min, and respirations are 14/min. The patient is noted to have a slightly distended abdomen that is nontender. Eventually, this patient undergoes a biopsy. Which of the following layers most likely reveals the causative pathologic finding of this disease?
- A. Submucosa
- B. Mucosa
- C. Lamina propria
- D. Muscularis mucosa
- E. Muscularis propria (between muscle layers) (Correct Answer)
Autonomic innervation of abdominal organs Explanation: ***Muscularis propria (between muscle layers)***
- This patient's presentation with **chronic constipation**, **abdominal distention**, and **delayed meconium passage** is highly suggestive of **Hirschsprung disease**.
- The causative pathology in Hirschsprung disease is the **absence of ganglion cells** in the **myenteric (Auerbach's) and submucosal (Meissner's) plexuses**, which is definitively diagnosed by a rectal biopsy showing this lack of innervation.
- The **myenteric plexus** is located **between the inner circular and outer longitudinal layers** of the **muscularis propria**, making this the primary layer examined for diagnostic findings.
*Submucosa*
- While the **submucosal (Meissner's) plexus** is also affected in Hirschsprung disease and the submucosa can show absent ganglion cells, the **myenteric plexus** in the muscularis propria is the primary diagnostic target in rectal biopsies.
- Both plexuses are affected, but the muscularis propria is considered the most definitive layer for diagnosis.
*Mucosa*
- The **mucosa** is the innermost layer of the gastrointestinal tract, consisting of epithelium, lamina propria, and muscularis mucosa.
- This layer does **not** contain the enteric nervous system plexuses (myenteric or submucosal) responsible for gut motility, so biopsy of this layer alone would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
*Lamina propria*
- The **lamina propria** is a thin layer of connective tissue found within the **mucosa**, beneath the epithelium.
- This layer primarily contains blood vessels, lymphatics, and immune cells, and it is **not** where the ganglion cells of the enteric nervous system are located or where the primary pathology of Hirschsprung disease is found.
*Muscularis mucosa*
- The **muscularis mucosa** is a thin layer of smooth muscle that forms the outermost layer of the **mucosa**.
- It does not contain the enteric plexuses (myenteric or submucosal) responsible for gut motility, so its biopsy would not reveal the absent ganglion cells characteristic of Hirschsprung disease.
Autonomic innervation of abdominal organs US Medical PG Question 6: Which neurotransmitter is primarily responsible for parasympathetic effects on heart rate?
- A. Norepinephrine
- B. Dopamine
- C. Acetylcholine (Correct Answer)
- D. Epinephrine
Autonomic innervation of abdominal organs Explanation: ***Acetylcholine***
- **Acetylcholine** is the primary neurotransmitter released by postganglionic parasympathetic neurons.
- It acts on **muscarinic receptors** (M2 receptors) in the heart to decrease heart rate.
*Norepinephrine*
- **Norepinephrine** is primarily associated with the **sympathetic nervous system**, increasing heart rate and contractility.
- It acts on **beta-1 adrenergic receptors** in the heart.
*Dopamine*
- **Dopamine** is a precursor to norepinephrine and epinephrine, and primarily functions as a neurotransmitter in the **central nervous system** and in regulating renal blood flow.
- While it can have cardiac effects, it is not the primary neurotransmitter for parasympathetic actions on heart rate.
*Epinephrine*
- **Epinephrine** (adrenaline) is a hormone released by the adrenal medulla and a neurotransmitter in the sympathetic nervous system, causing an **increase in heart rate** and contractility.
- It works through **beta-1 adrenergic receptors**, antagonistic to parasympathetic effects.
Autonomic innervation of abdominal organs US Medical PG Question 7: You have been asked to deliver a lecture to medical students about the effects of various body hormones and neurotransmitters on the metabolism of glucose. Which of the following statements best describes the effects of sympathetic stimulation on glucose metabolism?
- A. Norepinephrine causes increased glucose absorption within the intestines.
- B. Without epinephrine, insulin cannot act on the liver.
- C. Peripheral tissues require epinephrine to take up glucose.
- D. Epinephrine increases liver glycogenolysis. (Correct Answer)
- E. Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.
Autonomic innervation of abdominal organs Explanation: ***Epinephrine increases liver glycogenolysis.***
- **Epinephrine**, released during sympathetic stimulation, primarily acts to increase **glucose availability** for immediate energy.
- It achieves this by stimulating **glycogenolysis** (breakdown of glycogen into glucose) in the liver via **beta-adrenergic receptors**.
*Norepinephrine causes increased glucose absorption within the intestines.*
- **Norepinephrine** primarily causes **vasoconstriction** and can *decrease* **intestinal motility** and nutrient absorption due to shunting blood away from the digestive tract during stress.
- Glucose absorption is mainly regulated by digestive enzymes and transport proteins, not directly increased by norepinephrine.
*Without epinephrine, insulin cannot act on the liver.*
- **Insulin** acts on the liver independent of epinephrine to promote **glucose uptake**, **glycogenesis**, and **lipid synthesis**.
- Epinephrine and insulin have **antagonistic effects** on liver glucose metabolism; epinephrine increases glucose output, while insulin decreases it.
*Peripheral tissues require epinephrine to take up glucose.*
- **Insulin** is the primary hormone required for **glucose uptake** by most peripheral tissues, especially **muscle** and **adipose tissue**, via **GLUT4 transporters**.
- Epinephrine generally *reduces* glucose uptake by peripheral tissues to preserve glucose for the brain during stress.
*Sympathetic stimulation to alpha receptors of the pancreas increases insulin release.*
- Sympathetic stimulation, primarily acting through **alpha-2 adrenergic receptors** on pancreatic beta cells, actually **inhibits** **insulin secretion**.
- This inhibition helps to increase blood glucose levels by reducing insulin's glucose-lowering effects.
Autonomic innervation of abdominal organs US Medical PG Question 8: A 28-year-old female comes to the emergency department complaining of heart palpitations. She has had multiple episodes of these in the past few months. She has found that if she wears tight clothing then sometimes these episodes will stop spontaneously. On presentation to the ED, she feels like her heart is pounding and reports feeling nauseous. She appears mildly diaphoretic. Her blood pressure is 125/75 mmHg, pulse is 180/min, and respirations are 22/min with an O2 saturation of 99% on room air. A neck maneuver is performed and her pulse returns to 90/min with improvement of her symptoms. Stimulation of afferent fibers from which nerve are most responsible for the resolution of her symptoms?
- A. Facial
- B. Hypoglossal
- C. Glossopharyngeal (Correct Answer)
- D. Trigeminal
- E. Vagus
Autonomic innervation of abdominal organs Explanation: ***Glossopharyngeal***
- The question specifically asks about **afferent fibers** responsible for the resolution of symptoms during the neck maneuver (carotid sinus massage).
- The **glossopharyngeal nerve (cranial nerve IX)** provides the **afferent (sensory) limb** of the baroreflex by carrying signals from **baroreceptors in the carotid sinus** to the nucleus tractus solitarius in the medulla.
- When the carotid sinus is massaged, baroreceptors are stimulated → afferent signals travel via **CN IX** → medullary cardiovascular centers → efferent vagal output → heart rate slows.
- This is the afferent pathway that initiates the reflex response to terminate **supraventricular tachycardia (SVT)**.
*Vagus*
- The **vagus nerve (cranial nerve X)** is crucial for treating SVT, but it provides the **efferent (motor) limb** of the baroreflex, not the afferent limb.
- After afferent signals from CN IX reach the medulla, the vagus nerve carries parasympathetic output to the SA node to slow the heart rate.
- If the question asked about efferent fibers, vagus would be correct, but it asks specifically about **afferent fibers**.
*Facial*
- The **facial nerve (cranial nerve VII)** primarily controls **facial expressions**, carries taste sensation from the anterior two-thirds of the tongue, and innervates salivary glands.
- It has no role in the baroreflex or cardiac rhythm regulation via neck maneuvers.
*Hypoglossal*
- The **hypoglossal nerve (cranial nerve XII)** is responsible for **tongue movement**.
- It has no involvement in cardiac rhythm regulation or the afferent pathways of the baroreflex.
*Trigeminal*
- The **trigeminal nerve (cranial nerve V)** mediates sensation from the face and controls the muscles of **mastication (chewing)**.
- While trigeminal stimulation via the **diving reflex** (cold water on face) can cause bradycardia, this is not the mechanism involved in carotid sinus massage for SVT treatment.
Autonomic innervation of abdominal organs US Medical PG Question 9: A 28-year-old man is admitted to the emergency department with a gunshot wound to the abdomen. He complains of weakness and diffuse abdominal pain. Morphine is administered and IV fluids are started by paramedics at the scene. On admission, the patient’s blood pressure is 90/60 mm Hg, heart rate is 103/min, respiratory rate is 17/min, the temperature is 36.2℃ (97.1℉), and oxygen saturation is 94% on room air. The patient is responsive but lethargic. The patient is diaphoretic and extremities are pale and cool. Lungs are clear to auscultation. Cardiac sounds are diminished. Abdominal examination shows a visible bullet entry wound in the left upper quadrant (LUQ) with no corresponding exit wound on the flanks or back. The abdomen is distended and diffusely tender with a rebound. Aspiration of the nasogastric tube reveals bloody contents. Rectal examination shows no blood. Stool guaiac is negative. Which of the following is the next best step in management?
- A. Focused assessment with sonography for trauma (FAST)
- B. Abdominal CT
- C. Exploratory laparotomy (Correct Answer)
- D. Abdominal X-ray
- E. Diagnostic peritoneal lavage
Autonomic innervation of abdominal organs Explanation: ***Exploratory laparotomy***
- The patient presents with clear signs of **hemodynamic instability** (BP 90/60 mmHg, HR 103/min, lethargy, cool extremities, diminished cardiac sounds) following a **gunshot wound to the abdomen**.
- In hemodynamically unstable trauma patients with penetrating abdominal injuries, immediate **exploratory laparotomy** is indicated to identify and control hemorrhage and repair organ damage.
*Focused assessment with sonography for trauma (FAST)*
- While FAST can detect free fluid (e.g., blood) in the abdomen, it is **not sufficient to rule out significant injury** in a hemodynamically unstable patient with a penetrating abdominal wound.
- A positive FAST in a stable patient might prompt further imaging, but in this unstable case, it would delay definitive surgical intervention.
*Abdominal CT*
- Abdominal CT is useful for evaluating intra-abdominal injuries in **hemodynamically stable** patients.
- Performing a CT on this unstable patient would delay critical surgical intervention and could lead to rapid deterioration in the scanner.
*Abdominal X-ray*
- An abdominal X-ray can sometimes identify the **location of a bullet** or **free air** under the diaphragm, but it has limited utility in assessing or quantifying intra-abdominal hemorrhage or solid organ injury.
- It is not the definitive diagnostic or therapeutic step for an unstable patient with a penetrating abdominal injury.
*Diagnostic peritoneal lavage*
- DPL is an invasive procedure that can detect intra-abdominal bleeding or perforation, but it has largely been **replaced by FAST and CT scans** in hemodynamically stable patients.
- For a hemodynamically unstable patient with a clear indication for surgery (penetrating trauma and instability), DPL would delay definitive surgical management and provides less information than direct visualization via laparotomy.
Autonomic innervation of abdominal organs US Medical PG Question 10: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
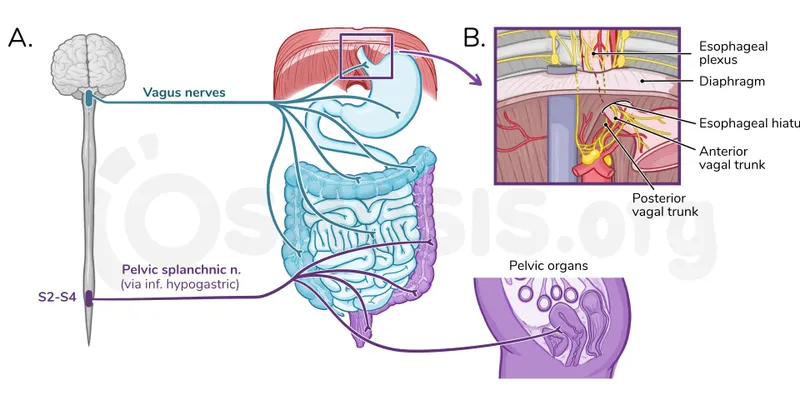
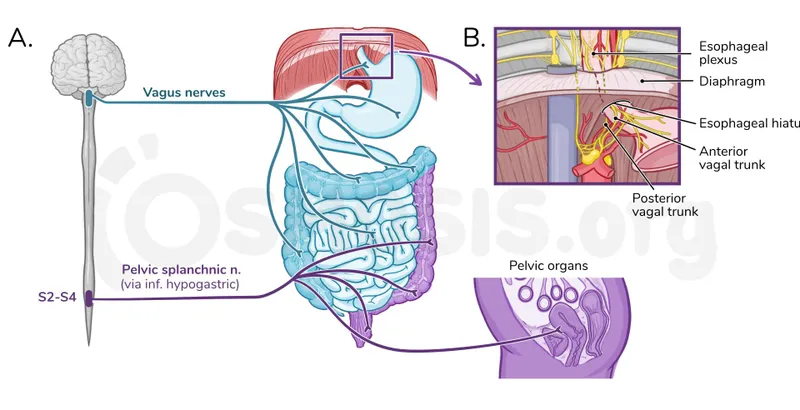
Autonomic innervation of abdominal organs Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
More Autonomic innervation of abdominal organs US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.