Autonomic dysfunction syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Autonomic dysfunction syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Autonomic dysfunction syndromes US Medical PG Question 1: A 44-year-old man presents to the emergency department with weakness. He states that he has felt progressively more weak over the past month. He endorses decreased libido, weight gain, and headaches. His temperature is 97.0°F (36.1°C), blood pressure is 177/108 mmHg, pulse is 80/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for an obese man who appears fatigued. He has abdominal striae, atrophied arms, and limbs with minimal muscle tone. His ECG is notable for a small upward deflection right after the T wave. A fingerstick blood glucose is 225 mg/dL. The patient's underlying condition will be addressed definitively, but in the interim, which of the following is the most appropriate pharmacologic agent for managing his hypertension?
- A. Metoprolol (Correct Answer)
- B. Torsemide
- C. Hydrochlorothiazide
- D. Insulin
- E. Eplerenone
Autonomic dysfunction syndromes Explanation: ***Metoprolol***
- This patient presents with signs and symptoms consistent with **Cushing's syndrome**, including truncal obesity, thin extremities, striae, hypertension, hyperglycemia, and weakness (likely from hypokalemia, as evidenced by the U wave on ECG).
- The severe hypertension (177/108 mmHg) requires immediate management while the underlying Cushing's syndrome is being addressed definitively.
- **Beta-blockers like metoprolol** are appropriate for managing hypertension in Cushing's syndrome as they counteract the increased cardiac output and sympathetic activation caused by cortisol excess without worsening the metabolic complications.
- Unlike thiazide or loop diuretics, beta-blockers do not worsen hyperglycemia or hypokalemia, both of which are already present in this patient.
*Torsemide*
- **Torsemide** is a loop diuretic that can cause **hypokalemia**, which would worsen this patient's existing hypokalemia (U wave on ECG) and muscle weakness.
- Loop diuretics are not first-line agents for hypertension in Cushing's syndrome unless there is evidence of fluid overload, which is not present in this case.
*Hydrochlorothiazide*
- **Hydrochlorothiazide** is a thiazide diuretic that can worsen both **hyperglycemia** and **hypokalemia**.
- This patient already has hyperglycemia (225 mg/dL) and evidence of hypokalemia (U wave on ECG), making thiazides a poor choice.
- Thiazides would exacerbate the metabolic complications of Cushing's syndrome.
*Insulin*
- While insulin would address the hyperglycemia, the question specifically asks about managing the **hypertension**, not the hyperglycemia.
- Insulin does not lower blood pressure and would not address the immediate cardiovascular risk from severe hypertension.
*Eplerenone*
- **Eplerenone** is a selective aldosterone antagonist used primarily for primary hyperaldosteronism or heart failure.
- While it can lower blood pressure, the primary pathophysiology in Cushing's syndrome is **cortisol excess**, not aldosterone excess.
- Additionally, eplerenone can cause hyperkalemia, which, while potentially beneficial in this hypokalemic patient, makes it less predictable and not first-line for hypertension management in this context.
Autonomic dysfunction syndromes US Medical PG Question 2: A 31-year-old nurse presents to the emergency department with palpitations, sweating, and jitteriness. She denies chest pain, shortness of breath, and recent illness. She states that she experienced weakness in her arms and legs and a tingling sensation in her fingers before the palpitations occurred. Medical and surgical history is unremarkable. Her mother has Grave’s disease. The patient has been seen in the ED multiple times for similar symptoms and was discharged after appropriate medical management. Today, her temperature is 37°C (98.6°F), blood pressure is 128/84 mm Hg, pulse is 102/min and regular, and respirations are 10/min. On examination, the patient appears diaphoretic and anxious. Her pupils are dilated to 5 mm. The rest of the examination is normal. Urine toxicology and B-HCG are pending. Which of the following is the next best step in management?
- A. Fingerstick blood glucose (Correct Answer)
- B. D-dimer levels
- C. Echocardiogram
- D. TSH levels
- E. Urine metanephrines
Autonomic dysfunction syndromes Explanation: ***Fingerstick blood glucose***
- In the emergency department, **point-of-care glucose testing** is a critical first step for any patient presenting with autonomic symptoms (palpitations, sweating, diaphoresis), altered mental status, or neurological complaints (weakness, tingling).
- **Hypoglycemia** is a life-threatening condition that can present with identical symptoms: palpitations, sweating, jitteriness, weakness, paresthesias, and altered mental status. It must be ruled out immediately as it requires urgent treatment.
- This test takes **seconds to perform** and provides immediate results that guide acute management, whereas other tests (TSH, D-dimer) take hours and do not address immediate life threats.
- The patient's recurrent ED visits with similar presentations that resolved with "appropriate medical management" suggest a functional or metabolic etiology rather than undiagnosed structural disease.
- **Standard ED protocol** dictates checking glucose in patients with these presentations before pursuing more extensive workups.
*TSH levels*
- While the family history of Grave's disease raises suspicion for hyperthyroidism, this is a **screening test for outpatient workup**, not an emergency intervention.
- **Hyperthyroidism** does not typically cause weakness and tingling as **preceding symptoms** before palpitations. The symptom progression described is more consistent with hyperventilation or panic attacks.
- **Thyroid storm** would present with fever (temperature >38.5°C), not the normal temperature of 37°C seen here.
- TSH results take hours to return and do not guide immediate ED management. After stabilizing the patient and ruling out acute emergencies, thyroid function testing may be appropriate for outpatient follow-up.
*D-dimer levels*
- **D-dimer** screens for thromboembolic disease such as pulmonary embolism, which typically presents with **chest pain, shortness of breath, and hypoxia**—all explicitly denied by this patient.
- The patient's presentation involves autonomic and neurological symptoms without cardiopulmonary complaints, making thromboembolism unlikely.
*Echocardiogram*
- An **echocardiogram** evaluates cardiac structure and function and would be indicated if there were concerns for structural heart disease, valvular abnormalities, or persistent arrhythmias.
- However, the patient has a **regular pulse** at 102/min (mild sinus tachycardia) without evidence of arrhythmia or hemodynamic instability.
- This is not the appropriate first diagnostic step for undifferentiated autonomic symptoms in the ED.
*Urine metanephrines*
- **Urine metanephrines** test for **pheochromocytoma**, a rare catecholamine-secreting tumor that causes paroxysmal hypertension, palpitations, and sweating.
- While pheochromocytoma is in the differential for recurrent autonomic episodes, it is **extremely rare** and would typically present with more severe hypertension during episodes.
- This is a **send-out test** taking days to result, not appropriate for immediate ED management. Point-of-care glucose testing takes precedence.
Autonomic dysfunction syndromes US Medical PG Question 3: A 62-year-old woman is referred to a tertiary care hospital with a history of diplopia and fatigue for the past 3 months. She has also noticed difficulty in climbing the stairs and combing her hair. She confirms a history of 2.3 kg (5.0 lb) weight loss in the past 6 weeks and constipation. Past medical history is significant for type 2 diabetes mellitus. She has a 50-pack-year cigarette smoking history. Physical examination reveals a blood pressure of 135/78 mm Hg supine and 112/65 while standing, a heart rate of 82/min supine and 81/min while standing, and a temperature of 37.0°C (98.6°F). She is oriented to time and space. Her right upper eyelid is slightly drooped. She has difficulty in abducting the right eye. Pupils are bilaterally equal and reactive to light with accommodation. The corneal reflex is intact. Muscle strength is reduced in the proximal muscles of all 4 limbs, and the lower limbs are affected more when compared to the upper limbs. Deep tendon reflexes are bilaterally absent. After 10 minutes of cycling, the reflexes become positive. Sensory examination is normal. Diffuse wheezes are heard on chest auscultation. Which of the following findings is expected?
- A. Thymoma on CT scan of the chest
- B. Incremental pattern on repetitive nerve conduction studies (Correct Answer)
- C. Periventricular plaques on MRI of the brain
- D. Antibodies against muscle-specific kinase
- E. Elevated serum creatine kinase
Autonomic dysfunction syndromes Explanation: ***Incremental pattern on repetitive nerve conduction studies***
- The patient's symptoms (diplopia, fatigue, proximal muscle weakness, absent reflexes that normalize with exercise) are highly suggestive of **Lambert-Eaton myasthenic syndrome (LEMS)**.
- LEMS is characterized by impaired acetylcholine release at the neuromuscular junction, which manifests as an **incremental response** (progressively larger muscle action potentials) during high-frequency repetitive nerve stimulation.
*Thymoma on CT scan of the chest*
- **Thymoma** is strongly associated with **myasthenia gravis**, which typically presents with fluctuating weakness that worsens with activity and improves with rest, unlike the LEMS presentation.
- While LEMS can be paraneoplastic, it is most commonly associated with **small cell lung carcinoma**, not thymoma, making this finding less likely.
*Periventricular plaques on MRI of the brain*
- **Periventricular plaques** are characteristic findings in **multiple sclerosis**, a demyelinating disease of the central nervous system.
- Multiple sclerosis presents with diverse neurological deficits, but not typically with this specific pattern of fluctuating muscle weakness and absent deep tendon reflexes that improve with exercise.
*Antibodies against muscle-specific kinase*
- **Anti-MuSK antibodies** are associated with a specific subtype of **myasthenia gravis**, often presenting with prominent bulbar and respiratory weakness.
- While myasthenic syndromes share some features, the specific clinical picture (especially the improvement of reflexes with exercise) points away from standard myasthenia gravis and towards LEMS.
*Elevated serum creatine kinase*
- **Elevated creatine kinase** is typically seen in **myopathies** (e.g., inflammatory myopathies, muscular dystrophies) where there is direct muscle damage.
- In LEMS, the primary defect is at the neuromuscular junction, not within the muscle itself, so creatine kinase levels are usually normal.
Autonomic dysfunction syndromes US Medical PG Question 4: A 29-year-old woman presents to the primary care office for a recent history of falls. She has fallen 5 times over the last year. These falls are not associated with any preceding symptoms; she specifically denies dizziness, lightheadedness, or visual changes. However, she has started noticing that both of her legs feel weak. She's also noticed that her carpet feels strange beneath her bare feet. Her mother and grandmother have a history of similar problems. On physical exam, she has notable leg and foot muscular atrophy and 4/5 strength throughout her bilateral lower extremities. Sensation to light touch and pinprick is decreased up to the mid-calf. Ankle jerk reflex is absent bilaterally. Which of the following is the next best diagnostic test for this patient?
- A. MRI brain
- B. Ankle-brachial index
- C. Electromyography (including nerve conduction studies) (Correct Answer)
- D. Lumbar puncture
- E. Hemoglobin A1c
Autonomic dysfunction syndromes Explanation: ***Electromyography (including nerve conduction studies)***
- The patient's symptoms of **progressive weakness**, **sensory deficits** (carpet feels strange, decreased sensation up to mid-calf), **muscular atrophy**, and **absent ankle reflexes**, along with a **family history**, are highly suggestive of a **hereditary peripheral neuropathy** (e.g., Charcot-Marie-Tooth disease).
- **Electromyography (EMG)** and **nerve conduction studies (NCS)** are essential for confirming peripheral neuropathy, differentiating between demyelinating and axonal involvement, and localizing the lesion.
*MRI brain*
- An MRI brain would be indicated for central nervous system pathology, but the patient's symptoms (distal weakness, sensory loss with a "stocking-glove" distribution, absent reflexes) are highly suggestive of a **peripheral neuropathy**.
- There is no indication of upper motor neuron signs or other CNS involvement to warrant a brain MRI at this stage.
*Ankle-brachial index*
- Ankle-brachial index (ABI) is used to diagnose **peripheral artery disease (PAD)**, which typically presents with claudication (pain with exertion) and ischemic changes.
- The patient's symptoms of sensory changes and progressive weakness are not characteristic of PAD.
*Lumbar puncture*
- A lumbar puncture is primarily used to analyze **cerebrospinal fluid (CSF)** for inflammatory, infectious, or neoplastic conditions affecting the CNS or nerve roots (e.g., Guillain-Barré syndrome, which has acute onset).
- Given the chronic and progressive nature of her symptoms and a positive family history, it is less likely to be an acute inflammatory process of the nerve roots.
*Hemoglobin A1c*
- Hemoglobin A1c is used to screen for or monitor **diabetes mellitus**, which can cause a **diabetic neuropathy**.
- While diabetes can cause peripheral neuropathy, the patient's young age, lack of typical diabetic risk factors, and strong family history point more strongly towards a hereditary condition. Glycemic control does not fully explain her presentation.
Autonomic dysfunction syndromes US Medical PG Question 5: A 59-year-old man presents to his family practitioner with his wife. He has fallen several times over the past 3 months. Standing up from a seated position is especially difficult for him. He also complains of intermittent dizziness, excessive sweating, constipation, and difficulty performing activities of daily living. He denies fever, jerking of the limbs, memory disturbances, urinary incontinence, and abnormal limb movements. Past medical history includes a cholecystectomy 25 years ago and occasional erectile dysfunction. He takes a vitamin supplement with calcium and occasionally uses sildenafil. While supine, his blood pressure is 142/74 mm Hg and his heart rate is 64/min. After standing, his blood pressure is 118/60 mm Hg and his heart rate is 62/min. He is alert and oriented with a flat affect while answering questions. Extraocular movements are intact in all directions. No tremors are noticed. Muscle strength is normal in all limbs but with increased muscle tone. He is slow in performing intentional movements. His writing is small and he takes slow steps during walking with adducted arms and a slightly reduced arm swing. A trial of levodopa did not improve his symptoms. What is the most likely diagnosis?
- A. Huntington disease
- B. Shy-Drager syndrome (Correct Answer)
- C. Parkinson’s disease
- D. Progressive supranuclear palsy
- E. Wilson disease
Autonomic dysfunction syndromes Explanation: ***Shy-Drager syndrome***
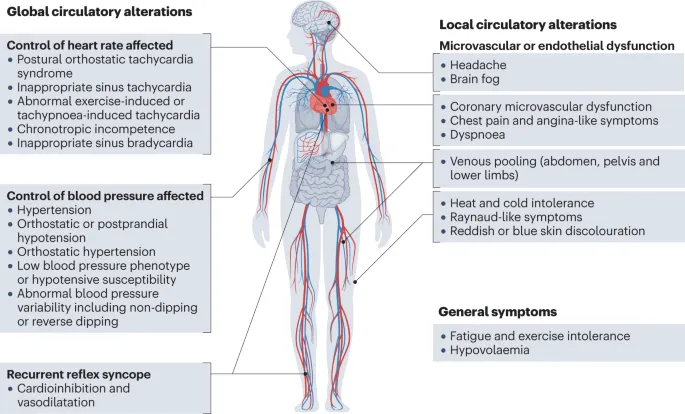
- The patient presents with **parkinsonism** (bradykinesia, rigidity, postural instability as evidenced by falls and difficulty standing) combined with severe **autonomic dysfunction** including orthostatic hypotension, intermittent dizziness, excessive sweating, constipation, and erectile dysfunction.
- The **lack of improvement with levodopa**, the prominent **autonomic features**, and the absence of specific Parkinson's disease red flags (like resting tremor or initial unilateral symptoms) strongly point to Shy-Drager syndrome, which is now classified under **Multiple System Atrophy (MSA)** with predominant parkinsonian features (MSA-P).
*Huntington disease*
- This is characterized by **chorea** (involuntary jerking movements) and psychiatric disturbances, which are not described in the patient's presentation.
- Typically presents with **cognitive decline** and **motor incoordination**, not the parkinsonian symptoms seen here.
*Parkinson’s disease*
- While this patient exhibits many features of **parkinsonism**, the prominent **autonomic dysfunction** and the **lack of response to levodopa** differentiate this case from typical Parkinson's disease.
- **Resting tremor** is a hallmark of Parkinson's disease, but it is explicitly noted that no tremors were noticed in this patient.
*Progressive supranuclear palsy*
- Key features include **supranuclear ophthalmoplegia** (especially vertical gaze palsy), prominent early falls, and neck dystonia (retrocollis).
- While early falls are present, the patient's **extraocular movements are intact in all directions**, making PSP less likely.
*Wilson disease*
- A rare genetic disorder characterized by **copper accumulation**, leading to hepatic, neurologic, and psychiatric symptoms.
- Manifestations include **hepatic dysfunction**, **Kayser-Fleischer rings** in the cornea, and a variety of movement disorders (e.g., tremor, rigidity), but not typically the severe orthostatic hypotension or lack of levodopa response seen here.
Autonomic dysfunction syndromes US Medical PG Question 6: A 15-year-old adolescent is brought to the physician by her parents. She is concerned that she has not started menstruating yet. She is also self-conscious because her chest has not yet developed and all of her friends are taller and much more developed. Past medical history is noncontributory. Her mother started menstruating around the age of 13 and her older sister at the age of 12. The patient is more concerned about her poor performance in sports. She says that she can not participate in sports like before and gets tired very early. Today, her heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature of 37.0°C (98.6°F). On physical exam, her heart has a regular rate and rhythm and lungs are clear to auscultation bilaterally. On physical exam, her brachial pulses appear bounding (4+) and her femoral pulses are diminished (2+). Her legs also appear mildly atrophic with poor muscle development bilaterally. Her neck appears short with excessive skin in the lateral neck area. This patient’s symptoms are most likely associated with which of the following conditions?
- A. Friedreich ataxia
- B. Marfan syndrome
- C. Turner syndrome (Correct Answer)
- D. Kartagener's syndrome
- E. Down syndrome
Autonomic dysfunction syndromes Explanation: ***Turner syndrome***
- The patient's presentation with **primary amenorrhea**, **lack of breast development**, **short stature**, **bounding brachial pulses** with **diminished femoral pulses** (suggesting coarctation of the aorta), and a **short neck with excessive skin** (webbed neck) are classic features of **Turner syndrome (45,XO)**.
- **Poor athletic performance** and **fatigue** can be attributed to the cardiovascular defect (coarctation), which reduces blood flow to the lower body and can lead to claudication or muscle weakness.
*Friedreich ataxia*
- This is a **neurodegenerative disorder** characterized by **progressive ataxia**, dysarthria, and scoliosis, often presenting in childhood or adolescence.
- While it can cause **cardiomyopathy** and fatigue, it does not typically present with the specific physical stigmata like webbed neck, short stature, or primary amenorrhea.
*Marfan syndrome*
- Characterized by tall stature, **arachnodactyly (long, slender fingers)**, **pectus excavatum**, **joint laxity**, and cardiovascular abnormalities like **aortic root dilation** and dissection.
- It does not cause short stature, webbed neck, primary amenorrhea, or coarctation of the aorta.
*Kartagener's syndrome*
- A subset of **primary ciliary dyskinesia**, characterized by the triad of **situs inversus**, **chronic sinusitis**, and **bronchiectasis**.
- This condition affects ciliary function and is not associated with the **gonadal dysgenesis**, **short stature**, or specific cardiovascular and physical anomalies seen in the patient.
*Down syndrome*
- Caused by **trisomy 21**, typically presenting with **intellectual disability**, **distinctive facial features** (e.g., epicanthic folds, upslanting palpebral fissures), single palmar crease, and often **congenital heart defects** (e.g., AV septal defects).
- While it can be associated with short stature and heart defects, it does not cause primary amenorrhea due to gonadal dysgenesis, webbed neck as a primary feature, or coarctation in the pattern described.
Autonomic dysfunction syndromes US Medical PG Question 7: A 68-year-old man comes to the physician because of double vision and unilateral right eye pain that began this morning. His vision improves when he covers either eye. He has hypertension, mild cognitive impairment, and type 2 diabetes mellitus. The patient has smoked two packs of cigarettes daily for 40 years. His current medications include lisinopril, donepezil, metformin, and insulin with meals. His temperature is 37°C (98.6°F), pulse is 85/minute, respirations are 12/minute, and blood pressure is 132/75 mm Hg. His right eye is abducted and depressed with slight intorsion. He can only minimally adduct the right eye. Visual acuity is 20/20 in both eyes. Extraocular movements of the left eye are normal. An MRI of the head shows no abnormalities. His fingerstick blood glucose concentration is 325 mg/dL. Further evaluation is most likely to show which of the following?
- A. Ptosis (Correct Answer)
- B. Dilated and fixed pupil
- C. Bitemporal hemianopsia
- D. Miosis and anhidrosis
- E. Positive swinging-flashlight test
Autonomic dysfunction syndromes Explanation: ***Ptosis***
- The patient's presentation of an **abducted and depressed right eye with minimal adduction** is highly suggestive of an **ischemic (diabetic) third nerve palsy**.
- Ischemic third nerve palsies characteristically **spare the pupillary fibers** (pupil remains normal in size and reactive) but affect the **somatomotor fibers** that innervate the extraocular muscles and the **levator palpebrae superioris**, leading to **ptosis**.
- The key clinical feature distinguishing ischemic from compressive CN III palsy is **pupil-sparing**, which is present in this case.
*Dilated and fixed pupil*
- A dilated and fixed pupil would indicate **compression of the oculomotor nerve**, often by an aneurysm (e.g., posterior communicating artery aneurysm).
- Compressive lesions affect the superficial **pupillomotor fibers** first, while ischemic third nerve palsies, as seen in patients with **diabetes**, typically affect the inner somatomotor fibers while **sparing the pupil**.
*Bitemporal hemianopsia*
- This visual field defect is characteristic of **optic chiasm compression**, commonly caused by a **pituitary adenoma**.
- This patient's symptoms are localized to a single eye and involve extraocular muscle dysfunction, not visual field loss.
*Miosis and anhidrosis*
- **Miosis** (constricted pupil) and **anhidrosis** (decreased sweating) on one side of the face, accompanied by **ptosis**, are classic signs of **Horner syndrome**.
- Horner syndrome results from a lesion in the **sympathetic pathway**, which is inconsistent with the extraocular muscle deficits observed in this patient.
*Positive swinging-flashlight test*
- A positive swinging-flashlight test (Marcus Gunn pupil) indicates an **afferent pupillary defect**, often seen in conditions affecting the **optic nerve** (e.g., optic neuritis, severe retinal disease).
- This patient's symptoms point to a **cranial nerve III palsy**, which affects efferent ocular movements and typically does not cause an afferent pupillary defect.
Autonomic dysfunction syndromes US Medical PG Question 8: A 45-year-old man comes to the physician for the evaluation of limited mobility of his right hand for 1 year. The patient states he has had difficulty actively extending his right 4th and 5th fingers, and despite stretching exercises, his symptoms have progressed. He has type 2 diabetes mellitus. He has been working as a mason for over 20 years. His father had similar symptoms and was treated surgically. The patient has smoked one pack of cigarettes daily for 25 years and drinks 2–3 beers every day after work. His only medication is metformin. Vital signs are within normal limits. Physical examination shows skin puckering near the proximal flexor crease. There are several painless palmar nodules adjacent to the distal palmar crease. Active and passive extension of the 4th and 5th digits of the right hand is limited. Which of the following is the most likely underlying mechanism of this patient's symptoms?
- A. Ulnar nerve lesion
- B. Ganglion cyst
- C. Palmar fibromatosis (Correct Answer)
- D. Tendon sheath tumor
- E. Tenosynovitis
Autonomic dysfunction syndromes Explanation: ***Palmar fibromatosis***
- The patient's symptoms, including **painless palmar nodules**, skin puckering near the flexor crease, and inability to actively extend the 4th and 5th fingers (a classic presentation of **Dupuytren's contracture**), are indicative of palmar fibromatosis.
- Risk factors like **male sex**, **age > 40**, **smoking**, **alcohol use**, **diabetes mellitus**, and a **family history** of similar symptoms are all present in this patient, strongly supporting the diagnosis.
*Ulnar nerve lesion*
- An ulnar nerve lesion would primarily cause **sensory deficits** (numbness/tingling in the 4th and 5th digits) and **motor weakness** in intrinsic hand muscles, leading to a **claw hand deformity**, not typically the presence of palmar nodules or skin puckering.
- While it can affect the 4th and 5th digits, the mechanism of limitation would be due to muscle weakness rather than fixed contracture.
*Ganglion cyst*
- A ganglion cyst is a **fluid-filled sac** that typically presents as a smooth, mobile, sometimes painful lump, often on the dorsal aspect of the wrist or fingers.
- It does not cause progressive finger contracture, skin puckering, or diffuse palmar nodules.
*Tendon sheath tumor*
- A tendon sheath tumor (e.g., giant cell tumor of the tendon sheath) is a **benign soft tissue mass** that presents as a firm, localized nodule, usually associated with a tendon.
- While it can limit finger movement, it typically does so by mass effect and does not cause the characteristic diffuse fibrotic changes and skin puckering seen in Dupuytren's contracture.
*Tenosynovitis*
- Tenosynovitis is **inflammation of the tendon sheath**, often causing pain, swelling, and tenderness along the course of the tendon, and sometimes a "triggering" sensation with movement.
- It does not typically manifest as painless, firm palmar nodules or progressive contracture with skin puckering.
Autonomic dysfunction syndromes US Medical PG Question 9: A 28-year-old man presented with gradually progressive gait disturbances since 10 years of age. His gait was clumsy and slow, and it was very difficult for him to perform brisk walking and running. After a few years, he developed tremors involving both upper limbs along with progressively increasing fatigability. Over the last several months, his friends have noticed that his speech has become slow, slurred, and sometimes incomprehensible. He has also developed difficulty in swallowing recently. On physical examination, he is vitally stable with normal sensorium and normal higher mental functions. The neurological examination reveals absent deep tendon reflexes in the lower extremities and the extensor plantar response bilaterally. Muscle tone is normal in different muscle groups with significant distal muscle wasting in the extremities. There is a marked loss of vibration and position senses. His gait is ataxic and nystagmus is present. His speech is explosive and dysarthric. The neurologist suspected a specific condition and asked for genetic testing, which identified 2 GAA trinucleotide repeat expansions. Which of the following is a correct statement related to the diagnosis of this patient?
- A. Gait ataxia in this condition is a pure sensory ataxia
- B. Restrictive cardiomyopathy is seen in approximately 50% of the patients
- C. The gene locus which is mutated in this condition is on chromosome 9 (Correct Answer)
- D. The condition is inherited as autosomal dominant condition
- E. Vertical nystagmus is characteristically seen in patients with this condition
Autonomic dysfunction syndromes Explanation: ***The gene locus which is mutated in this condition is on chromosome 9***
- The patient's presentation with gradually progressive gait disturbances, tremors, dysarthria, dysphagia, absent lower extremity deep tendon reflexes, extensor plantar responses, distal muscle wasting, loss of vibration/position senses, ataxic gait, and nystagmus, along with **GAA trinucleotide repeat expansions**, is classic for **Friedreich's ataxia**.
- The genetic defect in Friedreich's ataxia involves a **GAA trinucleotide repeat expansion** in the **FXN gene** located on **chromosome 9q13**, leading to reduced frataxin protein levels.
*Gait ataxia in this condition is a pure sensory ataxia*
- While **sensory ataxia** due to dorsal column dysfunction (loss of vibration and position sense) is a prominent feature, the ataxia in Friedreich's ataxia also has a significant **cerebellar component** as evidenced by dysarthria and nystagmus.
- Therefore, it is a **mixed sensory and cerebellar ataxia**, not a pure sensory ataxia.
*Restrictive cardiomyopathy is seen in approximately 50% of the patients*
- **Hypertrophic cardiomyopathy** is a common cardiac manifestation in Friedreich's ataxia, affecting approximately 60-90% of patients, and is a significant cause of morbidity and mortality.
- **Restrictive cardiomyopathy** is not a characteristic feature of Friedreich's ataxia.
*The condition is inherited as autosomal dominant condition*
- Friedreich's ataxia is inherited in an **autosomal recessive** pattern, meaning an individual must inherit two copies of the mutated gene (one from each parent) to develop the condition.
- The presence of the disease in only one parent would not lead to the child having the condition in an autosomal recessive inheritance pattern.
*Vertical nystagmus is characteristically seen in patients with this condition*
- Although nystagmus is common in Friedreich's ataxia, it is typically **horizontal nystagmus** or gaze-evoked nystagmus.
- **Vertical nystagmus** is more characteristic of other neurological conditions and is not a hallmark of Friedreich's ataxia.
Autonomic dysfunction syndromes US Medical PG Question 10: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Autonomic dysfunction syndromes Explanation: ***Pelvic splanchnic nerves***
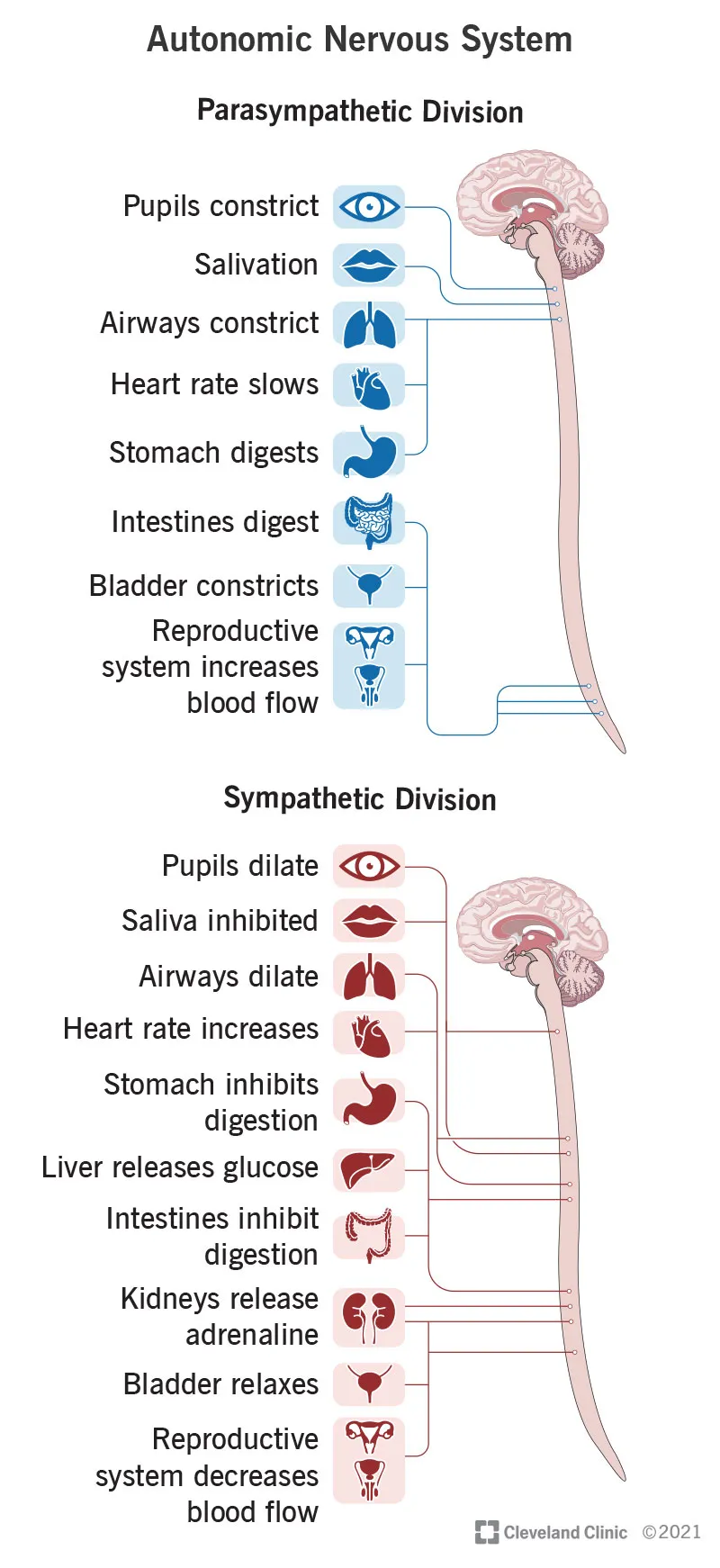
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
More Autonomic dysfunction syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.